© Author: Sazykina Oksana Yuryevna, therapist, cardiologist, especially for SosudInfo.ru (about the authors)
Injecting drugs directly into a patient's bloodstream via intravenous injection has long been common practice. It is this route of drug administration that ensures the rapid and effective occurrence of a therapeutic effect. But sometimes the patient’s veins are in a collapsed state or their wall is so fragile that normal access to a peripheral vein with a puncture of its wall (venipuncture) is extremely difficult. The healthcare professional then uses techniques such as catheterizing the vein or making a small incision in the vein (venesection). Due to the fact that a health worker of any specialty must have the technique of venipuncture, students begin to be taught this in their early courses. But venesection or venipuncture of central veins can only be used by anesthesiologists and resuscitators.
How is venipuncture different from venesection?
Puncture of a peripheral vein (any of the saphenous veins of the upper limb) is one of the simplest nursing or medical procedures that does not require special instruments or absolute sterility, as in an intensive care unit. In other words, puncture means puncture of the venous wall followed by insertion of a needle from a syringe, catheter, or intravenous infusion system. Venipuncture can be performed in the treatment room of a clinic, laboratory or hospital, as well as in the ward where the patient is receiving treatment. Both peripheral subcutaneous and central veins (subclavian, jugular) can be punctured. But in the latter case, the manipulation is carried out in an intensive care unit, where the patient is specially hospitalized or transferred.
Venesection differs from puncture in that after isolating the peripheral vein from the subcutaneous fat, the venous wall is fixed with clamps and then incised, followed by installation of a catheter or needle. The manipulation requires local anesthesia and is carried out under completely sterile conditions.
Tools
The list of tools for venesection is as follows:
- surgical knife;
- clamps to stop bleeding;
- anatomical and surgical tweezers;
- scissors with thin jaws;
- needle holders;
- silk and catgut ligatures;
- sharp hooks;
- syringe or intravenous system;
- anesthesia needles;
- vascular catheters.
In addition, the procedure requires:
- 50 ml of 0.25-0.5% novocaine solution;
- towels or sheets;
- latex gloves;
- dressing;
- gauze napkins and balls.
A set of tools for venesection must be prepared in advance. Often the procedure is needed for seriously ill patients, and preparation and processing activities take up the lion's share of time.
Indications for manipulation
Typically, venipuncture is necessary for the purpose of carrying out such therapeutic and diagnostic measures as:
- Intravenous administration of drugs as part of emergency care or routine treatment of a patient,
- Intravenous administration of radiopharmaceuticals or X-ray contrast agents for the purpose of radioscintigraphy (for example, myocardium, lungs) or radiography of internal organs (kidneys, brain),
- Exchange transfusion of blood or blood replacement solutions (fresh frozen plasma - FFP, erythromass, thrombomass),
- Carrying out parenteral nutrition - intravenous infusion of protein-saline solutions if it is impossible to feed by mouth,
- Administration of crystalloid solutions for detoxification purposes,
- Taking venous blood for research (for the purpose of a general clinical blood test, glucose analysis, biochemical indicators, HIV, syphilis, viral hepatitis and many other indicators).
Venipuncture of the central vein and venesection are carried out according to the same indications, but in cases where it is necessary to ensure rapid access of the drug to the bloodstream, and puncture of peripheral veins is not possible - in case of shock, collapse with low blood pressure, with collapsed veins due to high fever. Poor access to veins is also observed in people who use drugs intravenously for a long time. In addition, puncture of one of the internal jugular veins (right or left) is carried out if constant monitoring of central venous pressure (CVP) is necessary.
Forms of the disease
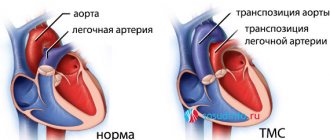
The classification of embolism is based on the type of embolus and its final location after migration has ceased.
Emboli carried by the venous system enter the heart, and from there to the lungs. Emboli carried by arteries can block blood vessels in different parts of the body.
Based on the origin of the embolus, the following types of embolism are distinguished:
- thromboembolism – emboli are blood clots in the arteries, veins and heart;
- air and gas - blockage of blood vessels when air enters the veins or from blood gas bubbles;
- adipose – fat cells act as emboli;
- tissue or cellular embolism – emboli are pieces of tissue or cell complexes;
- liquid embolism - blockage of amniotic fluid;
- bacterial embolism - blockage of blood vessels by accumulations of microbes;
- embolism with foreign bodies.
The most common are thromboembolism, fat embolism, air embolism, and gas embolism.
If the source of thromboembolism is thrombi in the chambers of the right half of the heart or in the veins of the systemic circulation, they enter the branches of the pulmonary artery system. In this case, spasms of the bronchial tree, coronary arteries of the heart, and branches of the pulmonary artery are observed. As a result of blockage of its small branches, hemorrhagic pulmonary infarction develops; damage to large branches can result in death.
With a fat embolism, a blockage of the venous bed occurs with drops of fat from destroyed or melted fat cells of the body. This becomes possible with extensive damage and trauma. Sometimes fat embolism occurs with the intravenous administration of fat solutions or preparations prepared in oil that are not intended for intravenous injection.
Once in the arterial bed, fat droplets do not dissolve in the blood, but accumulate in certain places. If the size of such a cluster exceeds the diameter of the vessel (6-8 microns), blood flow is disrupted. Fat embolism affects the small capillaries of the lungs and brain. It can have a subacute, acute (develops in the first hours after injury) and fulminant form (the onset of sudden death within a few minutes).
Air-gas embolism occurs when the lumen of the arterial vessels of the pulmonary circulation is blocked by bubbles of air or other gas, which accumulate in the cavity of the right heart and stretch it. If large veins are damaged, air can get into them, then air bubbles with the blood flow enter the heart and spread throughout all arterial basins. Even a small volume of air entering the peripheral veins can become fatal.
In the origin of gas embolism, the main role is played by sudden changes in atmospheric pressure (caisson disease, which develops during immersion and rapid rise from water), due to which undissolved gas bubbles block small arterial vessels without compromising their integrity.
Difference in the form of pathology:
- endogenous - the formation of free emboli from tissues and vessels occurs against the background of a sharp drop in ambient atmospheric pressure;
- exogenous - appears against the background of vascular damage, for example, with a chest injury, the appearance of negative pressure on inspiration is noted, which causes the absorption of free air.
Separation according to the location of VE in arteries and veins:
- subclavian;
- femoral or iliac;
- pulmonary;
- carotid (or its branches);
- aortic visceral branches.
Depending on the location of air bubbles in the vascular system, pathology is divided into two main types - venous and arterial.
Venous
Only with a large accumulation of emboli, especially in the right side of the heart, does a dysfunction of the organ occur that can pose a threat to human life.
Arterial
Arterial embolization is a more severe type of pathology that causes difficulty in the flow of blood to any internal organ, which leads to its dysfunction.
For example, blocking the lumen of the heart arteries can provoke a heart attack, and cerebral arteries - a stroke.
2-3 ml of free air is enough to lead to death in a person.
Are there possible contraindications for venipuncture and venesection?
There are no absolute contraindications for performing these manipulations, especially if intravenous administration of medications is vital. Relative contraindications include thrombophlebitis of the ulnar vein and violation of the integrity of the skin (abrasions, injuries) in the elbow bend. Venipuncture is a standard and fairly safe procedure, but should only be performed by a medically trained person. Venesection and puncture of one of the central veins are more complex in technique, and contraindications include a fracture of the collarbone and inflammatory processes on the skin of the punctured area. In this case, the manipulation can be performed on the healthy side.
Complications
During the operation, complications such as bleeding and damage to neighboring nerves are possible. A little later, the following consequences are possible:
- thrombosis;
- phlebitis;
- cannula blockage;
- wound infection.
Complications during venesection are most likely an exception if the procedure is performed by qualified medical personnel.
Peripheral vein puncture technique
The technique of performing venipuncture with therapeutic (administration of drugs) or diagnostic (blood sampling) is generally the same. Typically, the subcutaneous vein is used, a clearly visible vein in the area of the elbow, on the inner surface of the forearm (in its middle or lower third), as well as veins on the dorsum of the hand.
peripheral vein puncture technique
Before the procedure, the nurse must thoroughly clean their hands with an antiseptic and wear gloves (non-sterile disposable gloves are allowed). A tight tourniquet is applied to the skin of the middle third of the shoulder to reduce venous outflow from the limb, and the patient is asked to “work” with his fist, performing several flexion and extension movements with his fingers. This is necessary for better blood supply to the vein. Next, two swabs with an antiseptic (alcohol, chlorhexidine) are sequentially treated with a selected area of skin. Recently, small packaged sterile wipes have been used more often.
After treatment, the nurse presses the vein with the finger of the non-working hand (left for right-handers, right for left-handers) just above the site of the planned puncture, and places the index finger of the working hand on the needle cannula, clasping the syringe with the other fingers from above. At an angle of approximately 300, the needle is smoothly inserted into the vein, and when the needle enters the lumen of the vein, a feeling of “falling into the void” is felt. After this, you need to slightly pull the syringe plunger towards yourself to get a small amount of dark venous blood into the syringe and, thus, make sure that the needle is in the vein. Next, the tourniquet is untied with your free hand and the drug is administered, blood is drawn, or the system (“dropper”) is connected to the needle cannula.
Video: venipuncture for blood collection
Video: Venipuncture for intravenous injection
Video: detailed training film on venipuncture
I. Preparation for the procedure.
— Introduce yourself to the patient, explain the process and purpose of the procedure. Make sure that the patient has informed consent for the upcoming procedure of administering the drug and is not allergic to this drug.
If the patient is conscious and over 15 years of age; in other cases - from legal representatives.
If they are absent, the procedure is performed without obtaining informed consent:
— Invite the patient to empty the bladder, taking into account the duration of the procedure.
— Offer/help the patient take a comfortable position, which depends on his condition.
- Wash hands hygienically and dry.
— Fill the device for infusion of single-use infusion solutions and place it on the infusion stand.
Filling the device for infusion of single-use infusion solutions:
— Check the expiration date of the device and the tightness of the package.
— Read the label on the bottle: name, expiration date. Make sure of its suitability (color, transparency, sediment).
— Using non-sterile tweezers, open the central part of the metal cap of the bottle, treat the rubber stopper of the bottle with a cotton ball/napkin moistened with an antiseptic solution.
— Open the packaging bag and remove the device (all actions are performed on the desktop).
— Remove the cap from the air duct needle (a short needle with a short tube covered with a filter), insert the needle all the way into the stopper of the bottle, secure the free end of the air duct to the bottle (with a band-aid, pharmaceutical rubber band).
In some systems, the duct opening is located directly above the dripper. In this case, you only need to open the plug covering this hole.
— Close the screw clamp, remove the cap from the needle on the short end of the device, insert this needle all the way into the stopper of the bottle.
— Turn the bottle over and secure it on a tripod.
— Turn the dropper to a horizontal position, open the screw clamp: slowly fill the dropper to half the volume.
If the device is equipped with a soft dropper, and it is rigidly connected to the needle for the bottle, you must simultaneously squeeze it on both sides with your fingers and the liquid will fill the dropper.
— Close the screw clamp and return the dropper to its original position, with the filter completely immersed in the drug intended for infusion.
— Open the screw clamp and slowly fill the long tube of the system until the air is completely displaced and drops appear from the injection needle. It is better to pour drops of the drug into the sink under running water to avoid environmental contamination.
You can fill the system without putting on the injection needle, in which case drops should appear from the connecting cannula.
— Make sure there are no air bubbles in the long tube of the device (the device is full).
— Place a capped injection needle, napkins/cotton balls with skin antiseptic, and a sterile napkin in a sterile tray or packaging bag.
— Prepare 2 strips of narrow adhesive plaster, 1 cm wide, 4-5 cm long.
— Deliver to the room a manipulation table with the necessary equipment placed on it.
— Examine/palpate the site of the proposed venipuncture to avoid possible complications.
When performing venipuncture in the area of the ulnar fossa, invite the patient to extend the arm at the elbow joint as much as possible, for which place an oilcloth pad under the patient’s elbow.
— Apply a venous tourniquet (on a shirt or diaper) in the middle third of the shoulder so that the pulse on the radial artery is palpated and ask the patient to clench his hand into a fist several times and unclench it.
When performing venipuncture in the area of the ulnar fossa, apply a tourniquet in the middle third of the shoulder, check the pulse at the radial artery.
— When applying a tourniquet to a woman, do not use the hand on the side of the mastectomy.
— Wear gloves (non-sterile).
Subclavian vein puncture technique
Puncture of the subclavian vein, also called the “subclavian,” is performed only by an anesthesiologist-resuscitator. Typically, a catheter is installed in the subclavian vein for continuous administration of drugs to patients in serious condition.
The technique of this procedure is as follows. There are two types of subclavian - with a puncture of the vein under the collarbone and with a puncture of the vein above the collarbone. In both cases, the doctor’s hands and the selected area of skin are carefully treated with an antiseptic. The patient lies horizontally with his head turned in the opposite direction. Next, either a puncture of the skin or a small incision is made under local anesthesia (novocaine or lidocaine solution). The anesthetic is administered either with the same long needle that will puncture the vein (in the first case), or with a separate syringe before the incision (in the second case).
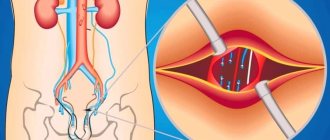
puncture of the subclavian vein: a – points of needle insertion, b – direction of the needle during puncture
The point of skin puncture is determined as follows: visually draw a horizontal line 1.5-2 cm down from the collarbone and vertical lines dividing it into three-thirds. The point of intersection of the horizontal line and the vertical line at the border of the middle and inner thirds of the clavicle will be the needle insertion point. The needle is inserted at an angle of 300 to the skin surface. When the needle enters the venous lumen, a sinking feeling is also determined, and after determining the presence of venous blood in the syringe, it is disconnected and a subclavian catheter is connected to the needle cannula (via a guide). The technique for placing a subclavian catheter is called Seldinger catheterization.
Quite often, a puncture of the subclavian vein is performed with a puncture of the skin in the supraclavicular area. To do this, the angle between the collarbone and the sternocleidomastoid muscle is visually determined, and then along the bisector of this angle at a distance of 0.5-1 cm from the collarbone, a long needle is inserted upward and towards the sternum at an angle to the skin surface of about 200.
Video: puncture and catheterization of the subclavian vein
Venipuncture in children
Intravenous urography: the essence of the method, research methodology
Performing V. in children, especially young children, is more difficult than in adults (small caliber of the veins, their deep location, restless behavior of the child during manipulation). The choice of veins for V. depends on their severity, goals and expected duration of infusions. With well-defined peripheral veins, for short infusions in children, the veins of the elbow, the saphenous veins of the leg, the dorsum of the foot and hand are punctured; in newborns and infants, the veins of the scalp are punctured. In case of poorly defined peripheral veins, when introducing concentrated or irritating solutions to the vein wall, or carrying out long-term infusions, central veins are used - subclavian, femoral, external and internal jugular; infusions are carried out through a needle or puncture catheterization is performed. The outer diameter of the needles used for V. in children is from 0.3 to 1.3 mm, depending on the purpose of V. and the diameter of the vein. The subclavian vein is punctured with the child in the supine position with a bolster under the shoulders, and the legs are raised above the level of the right heart. The puncture of the subclavian vein in children of the first year of life is performed from a point located in the middle of the clavicle, in children older than one year - at the border of the inner and middle third of it. During puncture, the needle forms an angle of 40-45° with the axis of the clavicle and 20-30° with the plane of the child’s chest. The femoral vein is punctured with the child in the supine position at a point located 1 - 2 cm downward from the inguinal ligament, slightly medial to the artery, determined by its pulsation. If long-term infusions are necessary and peripheral veins are poorly defined, venosections of the peripheral and central veins or puncture catheterization of the central veins are performed (see Puncture catheterization of veins).
Bibliography:
V. in children
— Doletsky S. Ya. and Isakov Yu. F. Pediatric surgery, part 1, p. 117, M., 1970; Operative surgery of children, ed. E. M. Margorina, p. 40, L., 1967; Timoschenko O.A. and Balagin B.M. Catheterization of the subclavian vein in children, Surgery, No. 7, p. 62, 1969, bibliogr.; A ubani a with R. Une nouvelle voie d'injection ou de ponction veineuse, Sem. Hop. Paris, t. 28, p. 3445, 1952; Lasfargues G. Les procedes pratiques de rehydration au cours des deshydratations aigues de l'enfant, Rev. Prat. (Paris), t. 14, p. 189, 1964; Y o ffa D. Supraclavicular subclavian venepuncture and catheterization, Lancet, v. 2, p. 614, 1965.
Technique for puncture of the internal jugular vein
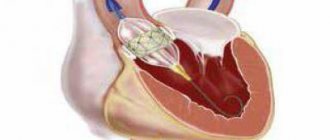
puncture of the internal jugular vein
Puncture of the jugular vein is also carried out using the installation of a guidewire according to the Seldinger method and is carried out in the department of anesthesiology and intensive care by a doctor. After cleaning the hands, the puncture site is determined. To do this, the patient's head with the foot end of the bed raised is turned in the direction opposite to the puncture and the skin is treated. Visually, the doctor determines the apex of the triangle, which is formed by the legs of the sternocleidomastoid muscle.
Next, the jugular vein is felt with a finger, and the pulse in the carotid artery is determined with the finger of the other hand. After injecting the anesthetic into the skin and subcutaneous fat, a long needle is inserted towards the nipple to a depth of 2-3 cm, often pulling the syringe plunger towards itself. After a little blood appears in the syringe, the needle is pulled out, and a thin conductor remains in the venous lumen to which the system is connected.
Features of the donor
When performing a vein puncture to donate blood, the requirements for sterility increase many times over. The procedure is carried out in specially equipped rooms; it is not allowed to use any consumables without checking the labeling and expiration date.
Pre-treat two elbow bends with antiseptics in an area of at least 7-8 cm in diameter twice. The puncture begins no earlier than 30 seconds after treatment. If a non-sterile object accidentally touches the puncture site, the disinfection procedure is repeated again.
A needle from a polymer container is used to pierce a vein and pass about 5 mm along its course. Then, after blood appears in the tube, the needle is advanced half the length and fixed throughout the entire blood sampling. It is necessary to achieve a fairly rapid flow of blood into the container. If this does not happen, then the following measures are taken:
- change the position of the needle cut;
- reinstall the tourniquet (it remains on the shoulder throughout the blood draw);
- use the other hand.
If repeated venipuncture is unsuccessful, the donor is removed from donating blood.
Venesection technique
Venesection is usually performed on a peripheral vein in cases where vein puncture cannot be performed. To do this, after treating the hands and the selected area of skin, a tourniquet is applied proximal to the puncture site.
venesection
After injecting the anesthetic into the skin and subcutaneous fat, a skin incision is made. A surgical thread is placed under the vein and the vein is ligated. Then, using a scalpel, a short incision is made in the venous wall proximal to the thread. The thread is removed, and a catheter is inserted into the section. Stitches are placed on the skin and removed after a few days.
Video: theory and examples of venesection
Possible difficulties
Venipuncture has no contraindications, but there are some nuances that sometimes interfere with this procedure.
- Anatomical features. For example, in people who take drugs for a long time by injecting drugs through a vein, the vessels are too thin and “dry”, so they are difficult to find. Therefore, sometimes doctors have to prick not the inner bend of the elbow, but some other place where the vein is visible.
- Injuries, burns and other extensive wounds in the area of the intended venipuncture. You also have to look for another vein, in a healthy area of the body.
- Hemophilia is a disease associated with reduced blood clotting. In this case, venipuncture should be performed only under the supervision of a physician, and the patient should be kept in the hospital for observation after the procedure.
Diagnostic Center – “Moscow Doctor”
Any medical professional is well aware that correct diagnosis is extremely important to prescribe effective treatment. And its full implementation is impossible without the use of modern equipment, laboratory reagents and other aids.
Basically, they are prescribed depending on what the patient's complaints are. As an option, it is possible to conduct a comprehensive examination initiated by a client who wants to learn as much as possible about the state of his health.
In order for the diagnosis to become truly effective, you should contact our clinic, your attending physician. He is the one who can give you directions for all the necessary types of tests and examinations.
In addition, it is important to remember one simple fact - even after learning the exact name of your disease, you should never self-medicate. Effective and at the same time safe therapy should be prescribed by a specialist
Types of diagnostics
One of the main diagnostic methods is to assess the composition of the blood and the presence of a number of substances in it, such as electrolytes, creatinine, as well as urea and much more. With liver tests, you can additionally obtain the level of concentration of the enzymes ALT, AST, as well as bilirubin, etc.
And these are not all ailments that can be determined by laboratory tests. Today, serological tests are mainly used to determine the types of infections affecting the patient’s body.
Thanks to them, it is possible to promptly identify various autoimmune diseases (in which there is a growth of antibodies that oppose the full functioning of the body’s own tissues). Urinalysis is used in combination with other types of examinations.
Thanks to him, the patient can find out about the presence of diseases of the genitourinary system, etc.
It is also important to study stool, guaranteeing the detection of the slightest signs of parasitic diseases, disturbances in the functioning of the gastrointestinal tract, etc. Hormonal blood tests are no less informative
Thanks to them, it is possible to identify any pathology of the endocrine system.
The diagnostic accuracy of this type of study is about 100%.
Moreover, if necessary, the doctor can take biological material (biopsy), thereby providing himself with the opportunity to make an extremely accurate diagnosis.
In particular, when visiting our clinic, you will be able to examine the stomach and duodenum by choosing a procedure such as gastroduodenoscopy. Thanks to it, you can determine the presence of erosions and ulcers, the first signs of gastritis, as well as any stenoses, localization, causes of bleeding, etc.
What it is
Translated from Latin vena – “vein” and sectio – “cut”. That’s right: during venesection, an incision is made on the wall of the vein, into which a cannula connected to a catheter is then inserted. Intravenous infusions (infusions) are administered through it. But it is impossible to cut a vein directly through the skin. Therefore, a small operation is first performed, exposing the vessel. To do this, they shallowly excise the skin and subcutaneous tissues with a scalpel, pry off the vein and begin to work with it directly.
Venesection has the following indications:
- a pronounced layer of subcutaneous fat;
- very low patient pressure (impossible to find a vein and get into it);
- Anatomically, the veins lie very deep.
Contraindications are problems on the skin at the site of excision. These are burns, fungal or purulent infections, unhealed wounds. A relative contraindication is thrombophlebitis: in this case, the advisability of venesection is decided, because sometimes this procedure is vital.
When performing venesection, they try to isolate large vessels so that the catheter can be freely installed. The following veins are best suited for this:
- ulna (on the inner bend of the elbow);
- internal and external jugular (in the neck);
- subclavian (in the area of the collarbone);
- femoral (in the lower leg area).