Artificial respiration (AR) is an urgent emergency measure if a person’s own breathing is absent or impaired to such an extent that it poses a threat to life. The need for artificial respiration may arise when providing assistance to those who have received sunstroke, drowned, suffered from electric current, as well as in case of poisoning with certain substances.
The purpose of the procedure is to ensure the process of gas exchange in the human body, in other words, to ensure sufficient saturation of the victim’s blood with oxygen and the removal of carbon dioxide from it. In addition, artificial ventilation has a reflex effect on the respiratory center located in the brain, as a result of which independent breathing is restored.
Mechanism and methods of artificial respiration
Content:
- Mechanism and methods of artificial respiration
- Indications and contraindications
- Preparing for artificial respiration
- Artificial respiration from mouth to mouth
- Artificial respiration from mouth to nose
- How long does artificial respiration last?
- Features of the procedure in children
- Manual methods of artificial respiration
- Hardware artificial respiration methods
- Complications of artificial respiration
Only through the process of breathing does a person’s blood become saturated with oxygen and carbon dioxide is removed from it. After air enters the lungs, it fills the lung sacs called alveoli. The alveoli are pierced by an incredible number of small blood vessels. It is in the pulmonary vesicles that gas exchange takes place - oxygen from the air enters the blood, and carbon dioxide is removed from the blood.
If the body's supply of oxygen is interrupted, vital activity is at risk, since oxygen plays the “first fiddle” in all oxidative processes that occur in the body. That is why, when breathing stops, artificially ventilating the lungs should be started immediately.
The air entering the human body during artificial respiration fills the lungs and irritates the nerve endings in them. As a result, nerve impulses are sent to the respiratory center of the brain, which are a stimulus for the production of response electrical impulses. The latter stimulate contraction and relaxation of the diaphragm muscles, resulting in stimulation of the respiratory process.
Artificially supplying the human body with oxygen in many cases makes it possible to completely restore the independent respiratory process. In the event that cardiac arrest is also observed in the absence of breathing, it is necessary to perform a closed cardiac massage.
Please note that the absence of breathing triggers irreversible processes in the body within five to six minutes. Therefore, timely artificial ventilation can save a person’s life.
All methods of performing ID are divided into expiratory (mouth-to-mouth and mouth-to-nose), manual and hardware. Manual and expiratory methods are considered more labor-intensive and less effective compared to hardware methods. However, they have one very significant advantage. They can be performed without delay, almost anyone can cope with this task, and most importantly, there is no need for any additional devices and instruments, which are not always at hand.
Respiratory support: Transferring children to independent breathing
The frequency of use of artificial ventilation has increased significantly in recent years, and is currently the main method of therapeutic intervention in intensive care units (ICU) of medical institutions.
Artificial pulmonary ventilation (ALV) is an event that allows you to save the lives of patients, but, due to a fairly large number of complications, it is rational to stop it immediately after detecting positive dynamics in the clinical picture of patients.
Rice. 1 Engstrom Carestation ventilator for adults, children and newborns
The appearance and further development of negative consequences can be reduced if the patient switches to spontaneous breathing in a timely manner.
The small proportion of patients who require prolonged weaning from mechanical ventilation leads to disproportionate costs and significant strain on hospital staff, which in turn leads to major ethical and clinical problems.
Approximately forty percent of the time patients spend on ventilators is spent transitioning them to spontaneous breathing.
Thanks to technological progress and optimization of technologies in microprocessor systems of ventilators, multiple new ventilation modes have begun to be introduced into clinical practice. But, since full-fledged operation requires a complex relationship between the capabilities of the device and the needs and respiratory activity of patients, most of them allow the implementation of a number of auxiliary modes.
The use of spontaneous breathing, in addition to facilitating the transition of patients to spontaneous breathing, also helps to eliminate the adverse effects that are associated with mechanical ventilation.
Today, a huge amount of research is being conducted aimed at identifying parameters that predict the ability to extubate a patient and select a ventilation mode that would be optimal. However, these studies have not yet led to the only correct and best solution to this issue.
This article describes how approaches to transferring patients to spontaneous breathing have developed: their main advantages and disadvantages.
The invention and development of new approaches and modes in ventilation has led to the evolution of approaches to transferring patients to independent breathing.
Carrying out a spontaneous breathing test was the very first approach to emerge. At that time, this test was the only possible option, since specialists only had access to mandatory controlled ventilation (CMV) or IPVV. In this mode, the device, without any reaction to the patient’s attempts, blew in a certain volume of oxygen-air mixture.
In order to ensure oxygen access during periods of spontaneous breathing and prevent recirculation of exhaled air, a T-tube is used. A humidified oxygen mixture is supplied to the proximal leg of this system, and the flow of the mixture must be sufficient to prevent exhaled gas from entering the lungs from the distal leg of the system.
Today, this method is widespread and is used both as a test to determine the patient's ability to breathe independently, and as a training method for the muscles of the respiratory tract before extubation.
At the time of the advent of respiratory support, medical professionals were very skeptical about ideas about ventilation modes that could allow patients to independently perform breathing activities, which is extremely difficult to imagine today.
For example, Petty TL (1975) was categorically against the use of such a ventilation mode as “intermittent mandatory ventilation” (IMV). He believed that medical professionals needed complete confidence in the patient's volume of ventilation, and that reducing respiratory support and relying on the patient's ability to provide normal and sufficient gas exchange could well endanger him and lead to irreversible tragic consequences.
Despite this, at the same time there was information that “intermittent mandatory ventilation” (IMV) allows a gradual transition of the patient to spontaneous breathing, and in addition has great advantages for those patients whose body would not be able to withstand the test for spontaneous breathing (SBT)
The use of this method made it possible to gradually reduce the frequency of mechanical breathing, and, consequently, increase the load on the patients’ own respiratory muscles.
Thus, at the end of the eighties, data appeared on the effectiveness of this method: reducing the duration of mechanical ventilation, reducing the number of various complications, including barotrauma. These data have allowed the IMV regimen to take a leading place among all available methods for transferring patients to spontaneous breathing.
In adult practice, the most widely used approach is one in which the patient is immediately released from the ventilator. If the doctor decides that the patient is ready for independent breathing, an SBT test is performed, and if the patient tolerates it well, then extubation is performed. If the test result is negative, then the patient is left on one of the modes for assisted ventilation, usually for a day, and then the procedure is repeated daily. The success of regularly administering such a simple intervention was noted by Cohen IL in 1994, who studied an approach in which patients were given the SBT test three times a week for a total duration of 20 to 40 minutes. These procedures provided significant improvements in ventilator-dependent patients.
Today, there are several different ways to conduct a spontaneous breathing test. Historically, the first was the use of a T-tube, as described above.
Since the advent of respirators capable of responding to patient attempts, the patient disconnection procedure began to change to minimal support (CPAP = 5 cmH2O or PS = 7 cmH2O) to overcome the increased work of breathing that is associated with endotracheal tube resistance.
Despite the presence of studies showing that the work of breathing after extubation is significantly greater than with minimal support through an endotracheal tube, the main advantage of methods that do not require disconnecting patients from the device is the ability to monitor respiratory parameters, the ability to set alarm limits and clear dosing oxygen fractions in the inhalation mixture, and, of course, the possibility of quickly resuming respiratory support if necessary.
According to a study by Yang KL and Perren A., 30 minutes is enough to conduct the SBT test, since those who are unable to tolerate the test fail within the first twenty minutes, although previously it was customary to conduct a test lasting 120 minutes. Based on the results of 6 large studies, if the test is successfully completed and extubated, the possible risk of reintubation is about 13 percent, while in patients extubated without an initial test, the risk of reintubation increased to 40 percent.
In a study in children, Сhavez A. et al. performed the SBT test, 91 percent of patients passed it successfully, among whom only 7.8 percent were reintubated. These results are no different from those obtained with extubation based on the physician's clinical judgment.
The most common option in pediatric practice is the gradual cessation of respiratory support. In patients of the pediatric age group, transfer to spontaneous breathing usually includes not only disconnection from the ventilator itself, but also often a long period of decreased respiratory support, gradual “weaning.”
To implement gradual weaning of the patient, various modes are used that can maintain and support independent breathing. Modes such as IMV and SIMV allow you to gradually reduce the number of mechanical breaths, which allows the work of your own respiratory muscles to make an increasing contribution to ventilation each time.
When PS mode is used as a stand-alone mode, an adequate level of support for normal ventilation is initially established and then gradually reduced. As a rule, in practice a combination of IMV/SIMV modes with PS is used.
Comparisons between SIMV, PS and T-tube testing were conducted in two large studies in which patients were entered into the study after failing the spontaneous breathing test, and in both studies the duration of weaning was increased with the SIMV regimen. While Esteban A. (study of 130 patients who failed the initial SBT test) prefers the T-tube test, and Brochard L. prefers to use the PS mode.
In order to improve the parameters of the SIMV mode, researchers are comparing its combinations with pressure support.
The combination of SIMV and PSV modes has a number of significant advantages compared to using the SIMV mode separately, which was shown in the work of Yu.M. Tselovalnikov. (1998). Based on the results of this work, it was revealed that the process of stopping the use of mechanical ventilation using the SIMV and PSV modes proceeds more smoothly and does not lead to significant stress in the main functional systems of the patients’ bodies.
Reyes ZC et al. The results of their study show that with the simultaneous use of SIMV and PS modes, minimal respiratory support and extubation were achieved faster than in the group using only one SIMV mode. Also, research results indicating a significant reduction in the “weaning” period with the simultaneous use of SIMV and PS modes were demonstrated in the work of Jounieaux V. et al.
There are also special ventilation modes that can provide a guaranteed volume of each breath: volume support (VS) and pressure support with guaranteed volume. Using Volume Maintenance (VS) mode, weaning occurs semi-automatically, as the pressure level required to achieve the target volume decreases spontaneously as the patient's respiratory system improves.
A study by Randolph AG et al., however, did not find much difference between the use of PS, VS and no specific protocol aimed at reducing respiratory support in children.
Studies have also been conducted on non-invasive ventilation for weaning a group of patients with chronic obstructive pulmonary disease from mechanical ventilation: Research group Nava S. et al. noted a reduction in the duration of mechanical ventilation and length of hospitalization, while the group of Girault C. et al noted that despite a reduction in the duration of mechanical ventilation and faster extubation, the duration of hospitalization remained the same.
In extubated patients who developed intolerance within the first 48 hours, 2 large randomized trials reported worse survival with noninvasive ventilation compared with standard reintubation.
It follows that the data presented in the literature do not support this use of non-invasive ventilation.
A study was conducted on two groups of surgical patients: a transition to ventilation was made in a non-invasive manner after extubation of patients with a predicted difficult transition to spontaneous breathing and a comparison was made with postoperative oxygen insufflation. Studies have shown that using non-invasive ventilation reduced the length of stay in the ICU and also improved patient survival.
The method of creating continuous positive pressure (CPAP) during a spontaneous breathing test can improve oxygenation and reduce the work of breathing, however, to date, there are few studies that can prove its effectiveness in “weaning”; the studies are not randomized and have a small sample. In this regard, at the 2005 consensus conference on the issue of CPAP, it was concluded that the frequency of its use together with PS is quite high, but there is extremely insufficient data on the benefits of its single use during “weaning”.
There is also very little information on the use of BIPAP as a weaning regimen, and these studies tend to look at slightly different aspects. In one of the works, Calzia E. et al. a comparison was made between the use of BIPAP and PS modes: respiratory work in both cases was approximately at the same level, but PTP (pressure/time derivative) was higher with BIPAP, which may indicate a much greater load on the respiratory muscles, although, in general, support breathing in both modes was significantly higher than the required values.
In a study by Rathgeber J. et al. 586 patients after cardiac surgery were involved: an advantage in the duration of “weaning” was shown when using the BIPAP regimen (42 patients) versus the IMV and SIMV regimens (431 patients). The mean amount of midazolam used in BIPAP was significantly less than in the other groups, which may indicate less need for sedation.
Work by Marchenkov Yu.V. showed that for patients who had severe thoracic trauma and were ventilated using the BIPAP mode, it was possible to use earlier “mobilization” of the alveoli (compared to the SIMV mode). In addition, its use makes it possible to accelerate the transition from total respiratory support to spontaneous breathing and helps to significantly reduce the number of complications, duration of use of mechanical ventilation and deaths.
A study was conducted on breathing comfort using the following modes: BIPAP, SIMV, CPAP with the involvement of non-intubated volunteers from Nepal, as a result of which the BIPAP mode was recognized as the most comfortable (according to the comfort scale) during breathing, both during inhalation and during exhalation.
The remainder of the research on BIPAP and APRV regimens largely shows their benefits for patients with ARDS, oxygenation support after a recruitment maneuver, etc.
Of course, the very approach of gradually transferring a mechanically ventilated patient to spontaneous breathing is a very controversial issue; for example, in the book by Fuhrman BP and Zimberman J., this approach was called outdated. These authors believe that it is necessary to apply the same rule for extubation that applies to adult patients: if the criteria are met, extubate after a successful SBT test, which would reduce the duration of mechanical ventilation, reduce the number of complications and reduce the cost of mechanical ventilation. However, these conclusions are made on the basis of experimental data obtained in adults, and this version can only be supported by data on unplanned extubations, which are usually successful, but this suggests that the patient had the ability for independent respiratory activity, but he was on mechanical ventilation, which was tightened.
Thus, the issue of conducting comparative studies between the classic “traditional” transfer of the patient to independent breathing and the “modern” immediate disconnection of patients from the ventilator in the pediatric age group is relevant.
Rationality in the approach to choosing a weaning regimen from the device in combination with an assessment of the clinical picture, the experience of an anesthesiologist-resuscitator and the use of various criteria and tests will increase the chance of successful extubation.
Indications and contraindications
Indications for the use of ID are all cases where the volume of spontaneous ventilation of the lungs is too low to ensure normal gas exchange. This can happen in many urgent and planned situations:
- For disorders of the central regulation of breathing caused by impaired cerebral circulation, tumor processes of the brain or brain injury.
- For medicinal and other types of intoxication.
- In case of damage to the nerve pathways and neuromuscular synapse, which can be caused by trauma to the cervical spine, viral infections, the toxic effect of certain medications, and poisoning.
- For diseases and damage to the respiratory muscles and chest wall.
- In cases of lung lesions of both obstructive and restrictive nature.
The need to use artificial respiration is judged based on a combination of clinical symptoms and external data. Changes in pupil size, hypoventilation, tachy- and bradysystole are conditions that require artificial ventilation. In addition, artificial respiration is required in cases where spontaneous ventilation is “turned off” with the help of muscle relaxants administered for medical purposes (for example, during anesthesia for surgery or during intensive care for a seizure disorder).
As for cases where ID is not recommended, there are no absolute contraindications. There are only prohibitions on the use of certain methods of artificial respiration in a particular case. So, for example, if venous return of blood is difficult, artificial respiration modes are contraindicated, which provoke even greater disruption. In case of lung injury, ventilation methods based on high-pressure air injection, etc., are prohibited.
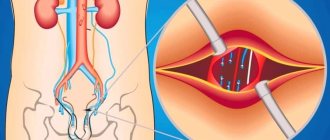
Invasive ventilation
An endotracheal tube is inserted into the trachea through the mouth or nose and connected to a ventilator.
With invasive respiratory support, the ventilator provides forced pumping of oxygen to the lungs and completely takes over the breathing function. The gas mixture is supplied through an endotracheal tube placed into the trachea through the mouth or nose. In particularly critical cases, tracheostomy is performed - a surgical operation to dissect the anterior wall of the trachea to insert a tracheostomy tube directly into its lumen.
Invasive ventilation is highly effective, but is used only if it is impossible to help the patient in a more gentle way, i.e. without invasive intervention.
Who needs invasive ventilation and when?
A person connected to a ventilator can neither speak nor eat. Intubation is not only inconvenient, but also painful. Because of this, the patient is usually placed in a medically induced coma. The procedure is carried out only in a hospital setting under the supervision of specialists.
Invasive ventilation is highly effective, but intubation involves placing the patient in a medically induced coma. In addition, the procedure is associated with risks.
Traditionally, invasive respiratory support is used in the following cases:
- lack of effect or intolerance of NIV in the patient;
- increased drooling or production of excessive sputum;
- emergency hospitalization and the need for immediate intubation;
- coma or impaired consciousness;
- possibility of respiratory arrest;
- presence of trauma and/or burns to the face.
How does an invasive ventilator work?
The operating principle of devices for invasive ventilation can be described as follows.
- For short-term mechanical ventilation, an endotracheal tube is inserted into the patient's trachea through the mouth or nose. For long-term mechanical ventilation, an incision is made in the patient's neck, the anterior wall of the trachea is dissected, and a tracheostomy tube is placed directly into its lumen.
- A breathing mixture is delivered through a tube into the lungs. The risk of air leakage is minimized, so the patient is guaranteed to receive the right amount of oxygen.
- The patient's condition can be monitored using monitors that display breathing parameters, the volume of supplied air mixture, saturation, cardiac activity, and other data.
Features of equipment for invasive ventilation
Equipment for invasive ventilation has a number of characteristic features.
- Completely takes over the breathing function, i.e. actually breathes instead of the patient.
- It requires regular checking of the serviceability of all valves, because... The patient’s life depends on the performance of the system.
- The procedure must be supervised by a doctor. Weaning the patient from the ventilator also requires the participation of a specialist.
- Used with additional accessories - humidifiers, cough cleaners, spare circuits, suction units, etc.
Preparing for artificial respiration
Before performing expiratory artificial respiration, the patient should be examined. Such resuscitation measures are contraindicated for facial injuries, tuberculosis, polio and trichlorethylene poisoning. In the first case, the reason is obvious, and in the last three, performing expiratory artificial respiration puts the person performing resuscitation at risk.
Before starting expiratory artificial respiration, the victim is quickly freed from clothing squeezing the throat and chest. The collar is unbuttoned, the tie is undone, and the trouser belt can be unfastened. The victim is placed supine on his back on a horizontal surface. The head is tilted back as much as possible, the palm of one hand is placed under the back of the head, and the other palm is pressed on the forehead until the chin is in line with the neck. This condition is necessary for successful resuscitation, since with this position of the head the mouth opens and the tongue moves away from the entrance to the larynx, as a result of which air begins to flow freely into the lungs. In order for the head to remain in this position, a cushion of folded clothing is placed under the shoulder blades.
After this, it is necessary to examine the victim’s oral cavity with your fingers, remove blood, mucus, dirt and any foreign objects.
It is the hygienic aspect of performing expiratory artificial respiration that is the most delicate, since the rescuer will have to touch the victim’s skin with his lips. You can use the following technique: make a small hole in the middle of a handkerchief or gauze. Its diameter should be two to three centimeters. The fabric is placed with a hole on the victim’s mouth or nose, depending on which method of artificial respiration will be used. Thus, air will be blown through the hole in the fabric.
Indications for CPR and diagnosis of clinical death
Almost the only indication for performing ID and NMS is the state of clinical death, which lasts from the moment of circulatory arrest until the onset of irreversible disorders in the body’s cells.
Before you start performing artificial respiration and chest compressions, you need to determine whether the victim is in a state of clinical death. Already at this very first stage, an unprepared person may have difficulties. The fact is that determining the presence of a pulse is not as easy as it seems at first glance. Ideally, the person providing assistance should feel the pulse in the carotid artery. In reality, he quite often does this incorrectly, moreover, he mistakes the pulsation of his blood vessels in his fingers for the pulse of the victim. It is because of such errors that the clause on checking the pulse in the carotid arteries when diagnosing clinical death, if assistance is provided by people without medical education, was removed from modern recommendations.
Currently, the following steps must be taken before starting NMS and ID:
- After locating a victim who you believe may be clinically dead, check for hazardous conditions around the victim.
- Then walk up to him, shake his shoulder and ask if he's okay.
- If he answered you or somehow reacted to your request, this means that he is not in cardiac arrest. In this case, call an ambulance.
- If the victim has not responded to your call, turn him on his back and open the airways (ensure airway patency). To do this, carefully straighten your head at the neck and move your upper jaw up.
- Once the airway is open, assess for normal breathing. Do not confuse agonal sighs, which may still be observed after cardiac arrest, with normal breathing. Agonal sighs are superficial and very rare, they are non-rhythmic.
- If the victim is breathing normally, turn him on his side and call an ambulance.
- If the person is not breathing normally, call others for help, call an ambulance (or have someone else do it), and begin CPR immediately.
Cardiopulmonary resuscitation according to the ABC principle
That is, for the onset of NMS and ID, the absence of consciousness and normal breathing is sufficient.
Indirect cardiac massage
Artificial respiration from mouth to mouth
To perform artificial respiration using the mouth-to-mouth method, the person who will provide assistance must be on the side of the victim’s head (preferably on the left side). In a situation where the patient is lying on the floor, the rescuer kneels. If the victim's jaws are clenched, they are forced apart.
After this, one hand is placed on the victim’s forehead, and the other is placed under the back of the head, tilting the patient’s head back as much as possible. Having taken a deep breath, the rescuer holds the exhalation and, bending over the victim, covers the area of his mouth with his lips, creating a kind of “dome” over the patient’s mouth. At the same time, the victim’s nostrils are pinched with the thumb and index finger of the hand located on his forehead. Ensuring tightness is one of the prerequisites for artificial respiration, since air leakage through the victim’s nose or mouth can nullify all efforts.
After sealing, the rescuer quickly, forcefully exhales, blowing air into the airways and lungs. The duration of exhalation should be about a second, and its volume should be at least a liter for effective stimulation of the respiratory center to occur. At the same time, the chest of the person receiving assistance should rise. If the amplitude of its rise is small, this is evidence that the volume of air supplied is insufficient.
Exhaling, the rescuer unbends, freeing the victim's mouth, but at the same time keeping his head thrown back. The patient should exhale for about two seconds. During this time, before taking the next breath, the rescuer must take at least one normal breath “for himself”.
Please note that if a large amount of air enters the patient's stomach rather than the lungs, this will significantly complicate his rescue. Therefore, you should periodically press on the epigastric region to empty the stomach of air.
Artificial respiration from mouth to nose
This method of artificial ventilation is carried out if it is not possible to properly unclench the patient’s jaws or there is an injury to the lips or oral area.
The rescuer places one hand on the victim’s forehead and the other on his chin. At the same time, he simultaneously throws back his head and presses his upper jaw to the lower. With the fingers of the hand that supports the chin, the rescuer must press the lower lip so that the victim’s mouth is completely closed. Taking a deep breath, the rescuer covers the victim’s nose with his lips and forcefully blows air through the nostrils, while watching the movement of the chest.
After artificial inspiration is completed, you need to free the patient's nose and mouth. In some cases, the soft palate may prevent air from escaping through the nostrils, so when the mouth is closed, there may be no exhalation at all. When exhaling, the head must be kept tilted back. The duration of artificial exhalation is about two seconds. During this time, the rescuer himself must take several exhalations and inhalations “for himself.”
How long does artificial respiration last?
There is only one answer to the question of how long ID should be carried out. You should ventilate your lungs in this mode, taking breaks for a maximum of three to four seconds, until full spontaneous breathing is restored, or until the doctor appears and gives other instructions.
At the same time, you should constantly ensure that the procedure is effective. The patient's chest should swell well, and the facial skin should gradually turn pink. It is also necessary to ensure that there are no foreign objects or vomit in the victim’s respiratory tract.
Please note that due to the ID, the rescuer himself may experience weakness and dizziness due to a lack of carbon dioxide in the body. Therefore, ideally, air blowing should be done by two people, who can alternate every two to three minutes. If this is not possible, the number of breaths should be reduced every three minutes so that the person performing resuscitation normalizes the level of carbon dioxide in the body.
During artificial respiration, you should check every minute to see if the victim’s heart has stopped. To do this, use two fingers to feel the pulse in the neck in the triangle between the windpipe and the sternocleidomastoid muscle. Two fingers are placed on the lateral surface of the laryngeal cartilage, after which they are allowed to “slide” into the hollow between the sternocleidomastoid muscle and the cartilage. This is where the pulsation of the carotid artery should be felt.
If there is no pulsation in the carotid artery, chest compressions in combination with ID should be started immediately. Doctors warn that if you miss the moment of cardiac arrest and continue to perform artificial ventilation, it will not be possible to save the victim.
Fundamentals of resuscitation techniques
The success of resuscitation largely depends on the time elapsed from the moment of circulatory arrest to the start of resuscitation.
The basis of measures to increase the survival rate of patients with circulatory and respiratory arrest is the concept of the “chain of survival”. It consists of a number of stages: at the scene, during transport, in the hospital operating room, in the intensive care unit and in the rehabilitation center. The weakest link in this chain is the effective provision of basic living standards at the scene. The outcome largely depends on it. It should be remembered that the time during which you can count on successful restoration of cardiac activity is limited. Resuscitation under normal conditions can be successful if started immediately or in the first minutes after the onset of circulatory arrest. The basic principle of resuscitation at all stages of its implementation is the provision that “resuscitation should prolong life, and not prolong death.” The final results of resuscitation largely depend on the quality of resuscitation. Errors in its implementation can subsequently be layered on the primary damage that caused the terminal condition.
The indication for resuscitation measures is a state of clinical death. Among the main causes of clinical death requiring resuscitation, the leading ones are: sudden circulatory arrest, airway obstruction, hypoventilation, apnea, blood loss and brain damage. Clinical death is the period between life and death, when there are no visible signs of life, but life processes are still ongoing, making it possible to revive the body. The duration of this period at normal body temperature is 5–6 minutes, after which irreversible changes develop in the tissues of the body. Under special conditions (hypothermia, pharmacological protection), this period is extended to 15-16 minutes.
Signs of clinical death are:
1. Arrest of blood circulation (lack of pulsation in the main arteries);
2. Lack of spontaneous breathing (no chest excursions);
3. Lack of consciousness;
4. Wide pupils;
5. Areflexia (no corneal reflex and pupillary reaction to light):
6. Appearance of the corpse (pallor, acrocyanosis).
When carrying out resuscitation, there are 3 stages and 9 stages. The symbolic abbreviation of resuscitation measures - the first letters of the English alphabet - emphasizes the fundamental importance of methodical and consistent implementation of all stages.
Stage I - basic life support. Consists of three stages:
A (airway open) - restoration of airway patency;
B (breath for victim) - emergency artificial ventilation and oxygenation;
C (circulation his blood) - maintaining blood circulation.
Stage II - further life support. It consists of restoring independent blood circulation, normalizing and stabilizing blood circulation and breathing parameters. Stage II includes three stages:
D (drug) - medications and infusion therapy;
E (ECG) - electrocardioscopy and cardiography;
F (fibrillation) - defibrillation.
Stage III - long-term maintenance of life in the post-resuscitation period. It consists of post-resuscitation intensive care and includes the stages:
G (gauging) - state assessment;
H (human mentality) restoration of consciousness;
I - correction of organ dysfunction.
In this manual, we will examine in detail only the first stage of resuscitation measures (A, B, C), leaving the remaining stages and stages for detailed study in subsequent courses.
So, stage A is the restoration of airway patency. When emergency conditions occur, the patency of the airways is often impaired due to the retraction of the tongue, which covers the entrance to the larynx and air cannot enter the lungs. In addition, in an unconscious patient there is always a danger of aspiration and blockage of the respiratory tract by foreign bodies and vomit.
To restore airway patency, it is necessary to perform a “triple airway maneuver”:
1) throwing back (hyperextension) of the head,
2) moving the lower jaw forward,
3) opening the mouth. To do this, with the II-V fingers of both hands, grab the ascending branch of the patient’s lower jaw near the auricle and push it forward (up) with force, shifting the lower jaw so that the lower teeth protrude in front of the upper teeth. During this manipulation, the anterior muscles of the neck are stretched, due to which the root of the tongue is raised above the back wall of the pharynx.
If the airways are obstructed by a foreign body, the victim should be placed in a lying position on his side and 3-5 sharp blows should be given with the lower part of the palm in the interscapular area. The oropharynx is cleaned with a finger, trying to remove the foreign body, then artificial respiration is attempted. If there is no effect, an attempt is made to restore the airways using the Greimlich maneuver - forced pressure on the abdomen. In this case, the palm of one hand is applied to the stomach in the midline between the navel and the xiphoid process. The second hand is placed on top of the first and presses on the stomach with quick movements up the midline. After ensuring airway patency, the next stage of resuscitation begins.
Stage B - artificial respiration. Artificial respiration is the injection of air or an oxygen-enriched mixture into the patient’s lungs, performed without or with the use of special devices, that is, temporary replacement of the function of external respiration. The air exhaled by a person contains from 16 to 18% oxygen, which allows it to be used for artificial respiration during resuscitation. It should be noted that in patients with respiratory and cardiac arrest, pulmonary tissue collapses, which is greatly facilitated by chest compressions. Therefore, it is necessary to provide adequate ventilation during cardiac massage. Each insufflation should take 1-2 seconds, since with a longer forced insufflation, air may enter the stomach. Insufflation must be done sharply and until the patient’s chest begins to rise noticeably. In this case, the victim exhales passively, due to the increased pressure created in the lungs, their elasticity and the mass of the chest. Passive exhalation should be complete. The respiratory rate should be 12-16 per minute. The adequacy of artificial respiration is assessed by periodic expansion of the chest and passive exhalation of air.
Technically, artificial ventilation of the lungs can be carried out by artificial respiration “mouth to mouth”, “mouth to nose”, artificial respiration through an S-shaped air duct and with the help of a mask and an Ambu bag. The most accessible and common method in prehospital intensive care is the simple method of mouth-to-mouth artificial respiration (Fig. 49 d, e, f). To do this, you need to pinch the patient’s nose with one hand, take a deep breath, press your lips tightly around the patient’s mouth (to the lips and nose of newborns and infants) and blow in air until the chest rises to the maximum. While blowing air, monitor the patient’s chest; it should rise when air is blown in. If the patient's chest rises, it is necessary to stop insufflation, lower the patient's mouth and turn his face to the side, giving the victim the opportunity to make a full passive exhalation; when the exhalation ends, take the next deep breath. First, two inflations of the lungs are made, each lasting 1-2 seconds. Then the pulse in the carotid artery is determined; if there is a pulse, repeat the inflation of the lungs - in adults there is approximately one inflation every 5 seconds (12 per minute); for children - one every 4 seconds (15 per minute); in infants - every 3 seconds (20 per minute) - until adequate spontaneous breathing is restored. Artificial respiration is performed at a frequency of 10-12 times per minute (once every 5-6 seconds).
Auxiliary ventilation is used against the background of preserved independent but inadequate breathing in the patient. Simultaneously with the patient's inhalation, additional air is injected through 1-3 respiratory movements. The inhalation should be smooth and correspond in time to the patient’s inhalation. It should be noted that restoring spontaneous breathing quickly restores all other functions. This is due to the fact that the respiratory center is the pacemaker for the brain.
Stage C – maintaining blood circulation. After circulatory arrest for 20–30 minutes, the heart’s automaticity and conductivity functions are preserved, which makes it possible to restore its pumping function. Regardless of the mechanism of cardiac arrest, cardiopulmonary resuscitation must be started immediately to prevent the development of irreversible damage to body tissues (brain, liver, heart, etc.) and the onset of biological death. The main purpose of cardiac massage is to create artificial blood flow. It should be understood that cardiac output and blood flow created by external cardiac massage are no more than 30% of normal and only 5% of normal cerebral blood flow. But, as a rule, this is enough to maintain the viability of the central nervous system during cardiopulmonary and cerebral resuscitation, provided that sufficient oxygenation of the body is achieved within several tens of minutes. At the prehospital stage, only indirect, or closed, cardiac massage is used (i.e., without opening the chest). Sharp pressure on the sternum leads to compression of the heart between the spine and sternum, reducing its volume and ejecting blood into the aorta and pulmonary artery, i.e. it is an artificial systole. At the moment the pressure stops, the chest expands, the heart takes on a volume corresponding to diastole, and blood from the vena cava and pulmonary veins enters the atria and ventricles of the heart. The rhythmic alternation of compressions and relaxations to some extent replaces the work of the heart, i.e., one of the types of artificial circulation is performed. The technique of performing indirect cardiac massage is as follows. The patient is placed on a hard, flat horizontal surface on his back (Fig. 50). Carrying out chest compressions on an armored bed does not make sense - the patient must be laid on the floor. Conductive massage
is located on the side of the patient and places his palms (one on top of the other) on the lower third of the sternum above the base of the xiphoid process by 2 - 3 cm.
You should pay attention to the fact that not the entire palm is located on the sternum, but only its proximal part in close proximity to the wrist (Fig. 51). Indirect cardiac massage itself consists of rhythmic (80 per minute) pressure on the patient’s sternum. In this case, the sternum should drop by at least 5–6 cm.
You should pay attention to the fact that in order to perform a massage correctly, the arms should be almost completely straightened at the elbow joints and pressure on the sternum should be applied with the entire mass of the torso. Many guidelines recommend starting chest compressions with a single strong blow to the patient’s sternum, since fibrillation is often the cause of impaired myocardial contractility and a precordial blow can stop the arrhythmia.
The actual sequence of actions during cardiopulmonary resuscitation is as follows. Option I – resuscitation is carried out by one person:
- if the victim is unconscious, his head is thrown back as much as possible, supporting his chin so that his mouth is slightly open. If necessary, the lower jaw is advanced. If injury to the cervical spine is suspected, moderate head tilting is used only to maintain airway patency. Check for spontaneous breathing (listening and feeling the flow of air at the victim’s mouth, nose, observing the excursion of the chest);
- if the victim is not breathing, perform two deep inflations of the lungs (the chest should rise). Each inflation is performed relatively slowly for 1-2 seconds, then pause to allow a complete passive exhalation;
- palpate the pulse in the carotid artery (5-10s). If a pulse is present, continue ventilation at a rate of about 12 inflations per minute in adults (one inflation every 5 seconds), 15 inflations per minute in children (about 4 seconds) and 20 inflations per minute (one every 3 seconds) in infants;
- if there is no pulse, begin chest compressions;
- carry out 15 compressions of the sternum with a frequency of 80-100 per 1 min. After 15 compressions, two inflations of the lungs are made and continue to alternate 15 compressions on the sternum with two inflations of the lungs;
- the sternum is pressed to the spine by approximately 4-5 cm in adults, 2.5-4 cm in young children and 1-2 cm in infants. The recovery of spontaneous pulse is checked every 1-3 minutes.
Option II – resuscitation is carried out by two people:
Those resuscitating should be on opposite sides of the victim to make it easier to change roles without interrupting resuscitation.
- if the victim is unconscious, the resuscitator (performing ventilation) tilts his head back;
- if the victim is not breathing, the first resuscitator performs two deep lung inflations;
- checks the pulse in the carotid artery;
- if there is no pulse, the second resuscitator begins compression of the sternum with a frequency of 80-100 per minute, the first resuscitator performing ventilation performs one deep inflation of the lungs after every 5 compressions of the sternum; while the lungs are being inflated, the second resuscitator makes a short pause;
- then continue alternating 5 pressures on the sternum with one inflation of the lungs until an independent pulse appears.
Signs of the effectiveness of the massage are the narrowing of previously dilated pupils, the disappearance of pallor and a decrease in cyanosis, pulsation of large arteries (primarily the carotid) in accordance with the frequency of the massage, and the appearance of independent respiratory movements. Indirect cardiac massage is not stopped for more than 5 seconds; it should be carried out until spontaneous heart contractions are restored, ensuring sufficient blood circulation. An indicator of this will be the pulse detected in the radial arteries and an increase in systolic blood pressure to 80-90 mm. Hg Art. The absence of independent heart activity with undoubted signs of the effectiveness of the massage is an indication for continued resuscitation. Carrying out a cardiac massage requires sufficient endurance; It is desirable to change the massager every 5-7 minutes, carried out quickly, without disturbing the rhythm of the heart massage.
Features of the procedure in children
When performing artificial ventilation for babies under one year of age, the mouth-to-mouth and nose technique is used. If the child is older than one year, the mouth-to-mouth method is used.
Small patients are also placed on their back. For babies under one year old, place a folded blanket under their back or slightly raise their upper body, placing a hand under their back. The head is thrown back.
The person providing assistance takes a shallow breath, seals her lips around the child’s mouth and nose (if the baby is under one year old) or just the mouth, and then blows air into the respiratory tract. The volume of air blown in should be less, the younger the patient. So, in the case of resuscitation of a newborn, it is only 30-40 ml.
If a sufficient volume of air enters the respiratory tract, chest movement occurs. After inhaling, you need to make sure that the chest drops. If you blow too much air into your baby's lungs, this can cause the alveoli of the lung tissue to rupture, causing air to escape into the pleural cavity.
The frequency of insufflations should correspond to the breathing frequency, which tends to decrease with age. Thus, in newborns and children up to four months, the frequency of inhalations and exhalations is forty per minute. From four months to six months this figure is 40-35. In the period from seven months to two years - 35-30. From two to four years it is reduced to twenty-five, in the period from six to twelve years - to twenty. Finally, in a teenager aged 12 to 15 years, the respiratory rate is 20-18 breaths per minute.
Indirect cardiac massage
NMS is the basis of resuscitation measures.
It is its implementation that ensures the minimum necessary blood supply to the brain and heart, so it is very important to know what actions are performed during indirect cardiac massage. Carrying out NMS should begin immediately after identifying the victim as lacking consciousness and normal breathing. For this:
- Place the heel of the palm of your right hand (for left-handers, the left hand) on the center of the victim’s chest. It should lie exactly on the sternum, slightly below its middle.
- Place your second palm on top of the first, then interlace their fingers. No part of your hand should touch the victim's ribs, as this increases the risk of fracture when performing NMS. The base of the lower palm should lie strictly on the sternum.
- Position your torso so that your arms rise above the victim’s chest perpendicularly and are extended at the elbow joints.
- Using your body weight (not arm strength), bend the victim's chest to a depth of 5-6 cm, then allow it to restore its original shape, that is, fully straighten, without removing your palm from the sternum.
- The frequency of such compressions is 100–120 per minute.
Current recommendations for CPR allow only NMS.
Performing NMS is hard physical work. It has been proven that after about 2–3 minutes, the quality of its performance by one person decreases significantly. It is therefore recommended that, if possible, people providing assistance change each other every 2 minutes.
Algorithm for indirect cardiac massage
Features of resuscitation in children
In children, resuscitation techniques differ from those in adults. The chest of babies under one year old is very tender and fragile, the heart area is smaller than the base of the palm of an adult, so pressure during indirect cardiac massage is performed not with the palms, but with two fingers.
- The frequency of clicks is at least 100 per minute.
- From 1 to 8 years of age, massage is done with one palm.
- The chest should move 2.5–3.5 cm.
- The massage should be performed at a frequency of about 100 pressures per minute.
- The ratio of inhalation to compression on the chest in children under 8 years old should be 2/15, in children over 8 years old - 1/15.
For children, artificial respiration can be performed using the mouth-to-mouth technique. Since babies have small faces, an adult can perform artificial respiration by immediately covering both the child’s mouth and nose. The method is then called “mouth to mouth and nose.” Artificial respiration is given to children at a frequency of 18–24 per minute.
Errors when performing NMS
- Delay in the start of the event. For a person in a state of clinical death, every second of delay in starting CPR can result in a lower chance of resumption of spontaneous circulation and a worsening neurological prognosis.
- Long breaks during NMS. It is allowed to interrupt compression for no longer than 10 seconds. This is done for ID, changing caregivers, or when using a defibrillator.
- Insufficient or too great compression depth. In the first case, the maximum possible blood flow will not be achieved, and in the second, the risk of traumatic injuries to the chest increases.
Artificial respiration
Manual methods of artificial respiration
There are also so-called manual methods of artificial respiration. They are based on changing the volume of the chest due to the application of external force. Let's look at the main ones.
Sylvester's method
This method is most widely used. The victim is placed on his back. A cushion should be placed under the lower part of the chest so that the shoulder blades and the back of the head are lower than the costal arches. In the event that artificial respiration is performed using this method by two people, they kneel on either side of the victim so as to be positioned at the level of his chest. Each of them holds the victim’s hand in the middle of the shoulder with one hand, and with the other just above the level of the hand. Next, they begin to rhythmically raise the victim’s arms, stretching them behind his head. As a result, the chest expands, which corresponds to inhalation. After two or three seconds, the victim’s hands are pressed to the chest, while squeezing it. This performs the functions of exhalation.
In this case, the main thing is that the movements of the hands are as rhythmic as possible. Experts recommend that those performing artificial respiration use their own rhythm of inhalation and exhalation as a “metronome”. In total, you should do about sixteen movements per minute.
ID using the Sylvester method can be performed by one person. He needs to kneel behind the victim’s head, grab his arms above the hands and perform the movements described above.
For broken arms and ribs, this method is contraindicated.
Schaeffer method
If the victim's arms are injured, the Schaeffer method can be used to perform artificial respiration. This technique is also often used for the rehabilitation of people injured while on the water. The victim is placed prone, with his head turned to the side. The one who performs artificial respiration kneels, and the victim’s body should be located between his legs. Hands should be placed on the lower part of the chest so that the thumbs lie along the spine and the rest rest on the ribs. When exhaling, you should lean forward, thus compressing the chest, and while inhaling, straighten, stopping the pressure. The elbows are not bent.
Please note that this method is contraindicated for fractured ribs.
Laborde method
The Laborde method is complementary to the Sylvester and Schaeffer methods. The victim's tongue is grabbed and rhythmically stretched, imitating breathing movements. As a rule, this method is used when breathing has just stopped. The resistance of the tongue that appears is evidence that the person’s breathing is being restored.
Kallistov method
This simple and effective method provides excellent ventilation. The victim is placed prone, face down. A towel is placed on the back in the area of the shoulder blades, and its ends are passed forward, threaded under the armpits. The person providing assistance should take the towel by the ends and lift the victim’s torso seven to ten centimeters from the ground. As a result, the chest expands and the ribs rise. This corresponds to inhalation. When the torso is lowered, it simulates exhalation. Instead of a towel, you can use any belt, scarf, etc.
Howard's method
The victim is positioned supine. A cushion is placed under his back. Hands are moved behind the head and extended. The head itself is turned to the side, the tongue is extended and secured. The one who performs artificial respiration sits astride the victim’s thigh area and places his palms on the lower part of the chest. With your fingers spread, you should grab as many ribs as possible. When the chest is compressed, it simulates inhalation; when the pressure is released, it simulates exhalation. You should do twelve to sixteen movements per minute.
Frank Eve's method
This method requires a stretcher. They are installed in the middle on a transverse stand, the height of which should be half the length of the stretcher. The victim is placed prone on the stretcher, the face is turned to the side, and the arms are placed along the body. The person is tied to the stretcher at the level of the buttocks or thighs. When lowering the head end of the stretcher, inhale; when it goes up, exhale. Maximum breathing volume is achieved when the victim's body is tilted at an angle of 50 degrees.
Nielsen method
The victim is placed face down. His arms are bent at the elbows and crossed, after which they are placed palms down under the forehead. The rescuer kneels at the victim’s head. He places his hands on the victim’s shoulder blades and, without bending them at the elbows, presses with his palms. This is how exhalation occurs. To inhale, the rescuer takes the victim’s shoulders at the elbows and straightens, lifting and pulling the victim towards himself.
Hardware artificial respiration methods
For the first time, hardware methods of artificial respiration began to be used back in the eighteenth century. Even then, the first air ducts and masks appeared. In particular, doctors proposed using fireplace bellows to blow air into the lungs, as well as devices created in their likeness.
The first automatic ID machines appeared at the end of the nineteenth century. At the beginning of the twenties, several types of respirators appeared at once, which created intermittent vacuum and positive pressure either around the entire body, or only around the patient’s chest and abdomen. Gradually, respirators of this type were replaced by air-injection respirators, which had less solid dimensions and did not impede access to the patient’s body, allowing medical procedures to be performed.
Best materials of the month
- Coronaviruses: SARS-CoV-2 (COVID-19)
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
All ID devices existing today are divided into external and internal. External devices create negative pressure either around the patient's entire body or around his chest, thereby inhaling. Exhalation in this case is passive - the chest simply collapses due to its elasticity. It can also be active if the device creates a positive pressure zone.
With the internal method of artificial ventilation, the device is connected through a mask or intubator to the respiratory tract, and inhalation is carried out by creating positive pressure in the device. Devices of this type are divided into portable, intended for work in “field” conditions, and stationary, the purpose of which is long-term artificial respiration. The former are usually manual, while the latter operate automatically, driven by a motor.