Assessing the state of breathing begins with determining its frequency and rhythm, taking into account the age of the child. It is better to calculate the respiratory rate in a sleeping child, although this is not always possible. When you are awake, your breathing rate is usually higher, so it is important to know the normal range.
The breathing rhythm of a healthy child is not regular; breathing varies both in frequency and depth. Periodically, the child takes a deep breath, which sometimes worries parents.
Features of the respiratory system in a child
During the period of intrauterine development of the fetus, the formation and development of vital organs occurs. Their formation is completed after birth. The respiratory system begins to function at full capacity only in adulthood.
Distinctive features of the respiratory system in children:
- At birth, the baby takes its first breath and the lungs open. Their volume is much smaller than the size of the chest. But it contains a sufficient number of blood vessels. To saturate their organs with oxygen, children make breathing movements more often than adults ;
- The large number of breathing movements of children is also due to the fact that the bulk of oxygen enters through the nasal passages. In children, they are narrow and short and contain a large number of lymphatic and blood vessels. At the slightest irritation (dust, infection or allergens), swelling of the mucous membrane occurs, which further complicates the passage of air into the lungs.
Children are not good at breathing through the mouth, so parents are advised to clean their nasal passages more often.
Differential diagnosis of poisonings accompanied by miosis
| Symptoms | Psychoactive substances | |||
| Opiates | Ethanol | Barbiturates | Benzodiazepines | |
| Pupil | Miosis | Miosis | Miosis | Miosis |
| Level of consciousness | Oppressed to coma | Excitement gives way to depression | Drowsiness, coma | Drowsiness, coma |
| Skin and mucous membranes | Pale, wet, sticky | Hyperemia gives way to pallor. Profuse sweating, hypersalivation. | “Barbiturate burn” - bubbles at the point of pressure | Sweating |
| Convulsions | Eat | Possible (a dangerous harbinger of coma) | No, muscle relaxation | No, muscle relaxation |
| Heart rate, pulse | Bradycardia, then thready pulse | Tachycardia gives way to bradycardia | Not changed | Not changed |
| HELL | Hypotension | Hypertension then hypotension | Hypotension | Hypotension |
| Breath | Depressed to the point of apnea | Tachyhypopnea | Oppressed | Oppressed |
| Pulmonary edema | Available | No | Eat | Eat |
| Bronchorea | No | No | No | No |
| T body | Demoted | Not changed | Not changed | Not changed |
| Abdominal pain | No | No | No | No |
| Dyspepsia | Vomit | No | Nausea, vomiting | Nausea, vomiting |
Differential diagnosis of poisonings accompanied by mydriasis
| Symptoms | Psychoactive substances | ||||||
| Tricyclic antidepressants | Cocaine | Ecstasy | Amphetamines | Hashish | LSD | Mushrooms are hallucinogens | |
| Pupil | Midriaz | Midriaz | Midriaz | Midriaz | Midriaz | Midriaz | Midriaz |
| Level of consciousness | Visual hallucinations, depression of consciousness up to coma | Excitement auditory hallucinations | Excitement, panic, delirium | Inducing psychosis | Excitement, possible hallucinations, delusions | Excitement, panic, hallucinations rave | Visual and auditory hallucinations |
| Skin and mucous membranes | Dry mucous membranes | Sweating, paleness, scratch marks, “cocaine bugs” | Sweating | Regular | Injected scleral vessels | Sweating | Sweating, hypersalivation |
| Convulsions | Possible | No | Reduction of jaws | No | Muscle reduction | No | No |
| Heart rate, pulse | Tachycardia, sudden cardiac arrest | Tachycardia | Tachycardia | Tachycardia | Tachycardia | Tachycardia | Bradycardia turns into tachycardia |
| HELL | Not changed | Hypertension | Not changed | Hypertension, then hypotension | Hypertension | Hypertension | Hypertension |
| Breath | Oppressed | Cocaine runny nose | Not changed | Bronchodilation | Not changed | Not changed | Not changed |
| Pulmonary edema | No | No | No | No | No | No | No |
| Bronchorea | No | No | No | No | No | No | No |
| T body | Hyperthermia | Hyperthermia | Hyperthermia | Hyperthermia | Not changed | Fever | Fever |
| Abdominal pain | Intestinal paresis | No | No | No | No | No | Eat |
| Dyspepsia | No | No | No | Nausea, vomiting | No | Nausea | Nausea, vomiting, diarrhea |
| Exicosis | No | No | Eat | No | No | No | Eat |
| Vision | Spasm of accommodation | Not changed | Not changed | Not changed | Not changed | Not changed | Diplopia |
Methods for calculating the breathing rate of a child
The respiratory rate in children (the norm by age has significant differences) is checked by pediatricians during monthly examinations and compared with indicators for the child’s age. Parents can count the number of inhalations and exhalations themselves. When determining indicators, you need to take into account the child’s age, weight category, general health condition and time of day.
Sequence of performing the procedure at home:
- Determine the child's breathing type. Up to 4 years of age, children predominate in belly breathing, that is, when inhaling and exhaling, the peritoneum (abdomen) rises and falls. From 4 to 10 years, predominantly chest breathing is observed. The rise and fall of the chest is visually noted. After 10 years, abdominal breathing predominates in males, and chest breathing in females.
- After determining the type of breathing, you need to prepare a watch with a second hand and bring the child into a calm state. Playing games, watching cartoons, or being scared about the upcoming procedure will not allow you to obtain accurate data. In infants, it is recommended to take measurements during sleep. The indicator will be slightly lower than during the waking period.
- A comfortable position for correctly counting inhalations and exhalations is a lying position. Children from 1 to 5 years old can be calmed with a rattle or calm conversation. In this case, the participation of 2 parents will be required.
- The number of breathing movements can be assessed visually or by placing your hand on your stomach or ribs.
- The most accurate indicators are those measured in 1 minute. If the child is fidgety, then it is allowed to make calculations for 15 or 30 seconds. Multiply the resulting number by 4 or 2. But the data will have an error.
- To increase the measurement accuracy, the procedure must be performed 3-4 times. The resulting arithmetic mean will give the exact number that needs to be compared with the age norm.
At the same time, it is recommended to measure the number of heartbeats. If there is a deviation in the indicators, the child should be shown to a pediatrician. The specialist will re-measure the indicator, taking into account accompanying factors (excess weight, presence of a runny nose).
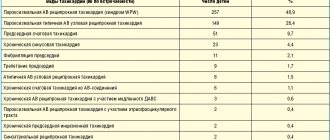
Treatment strategy
After a comprehensive examination of the child, a therapeutic program is developed. Taking into account the severity of the violations, the following technologies are often used:
- Rinsing the nasal passages and prescribing special medications.
- Creating positive pressure on a continuous basis in the airways so that air flow is continuously supplied to the body. This CPAP technique is safe for children.
- Removal of tonsils, that is, denotonsillectomy , is used for pathology and diseases of the ENT organs.
- Positional therapy , that is, treatment by changing body position .
- Surgical treatment vulopalatopharyngoplasty. Its purpose is to widen the airways when soft tissue is partially removed.
Purpose of research
Comparison of respiratory rate with standards is required to assess the development of the respiratory system and heart function. A change in indicators in any direction may indicate the presence of pathology (infectious and non-infectious in nature).
Timely identification of developmental deviations increases the likelihood of a child’s complete recovery, without the development of complications. If the measurements were taken over several days, then they need to be shown to the pediatrician. The data will allow you to make a diagnosis faster.
Norms of breathing rate in newborns
Newborns have the highest respiratory rates. Moreover, in premature babies, a reduced range may be important due to the irregularity of inhalations and exhalations. Deviations from the norm can only be determined by a pediatrician.
The permissible range of breathing rates in children under one year of age:
| Age parameter | Number of breathing movements in 1 minute | |
| Full-term babies | Premature | |
| From birth to 14 days | 40-60 | 20-80 |
| From 15 days to 3 months | 40-45 | 35-50 |
| From 3 to 6 months | 30-40 | 35-45 |
| Over 6 months and up to a year | 30-35 | 30-35 |
By the age of one year, the range of respiratory rates in full-term and premature infants narrows. In children born prematurely, breathing stops for 10-15 seconds, which is considered normal, if there is no blueness of the extremities and there is no developmental disorder of the child. If there are deviations, an urgent examination by a pediatrician is necessary.
Amount of water to cleanse the intestines
| Age | Amount of water for cleansing enema (ml) | Amount of water for siphon enema (ml) |
| 1-2 months | 30-40 | — |
| 2-4 months | 60 | 800-1000 |
| 6-9 months | 100-200 | 1000-1500 |
| 2-5 years | 200 | 1000-1500 |
| 6-10 years | 300 | 2000-3000 |
| Adults | 400-500 | 5000-8000 |
Norms of respiratory rate in children by age during wakefulness
The respiratory rate in children (the norm by age presented in the table does not take into account the characteristics of the child’s condition) gradually decreases until the child reaches 18 years of age. Since the lungs are fully expanded (over the entire chest), the condition of the nasal passages changes and the child learns to breathe through the mouth.
Respiratory rate indicators for children from one to 18 years of age:
| Age Ranges | Minimum number of breaths per minute | Maximum number of breaths per minute |
| From 1 year to 2 years | 30 | 35 |
| From 2 to 3 years | 25 | 35 |
| From 3 to 4 years | 25 | 30 |
| From 4 to 5 years | 20 | 30 |
| From 5 to 7 years | 20 | 25 |
| From 7 to 10 years | 18 | 25 |
| From 10 to 14 years old | 18 | 20 |
| From 14 to 18 years old | 16 | 20 |
When measuring the frequency of inhalations and exhalations yourself, it is recommended to pay attention to the depth of inhalations.
If your breathing is shallow, then it will naturally become more frequent to replenish the oxygen deficiency. If a child breathes deeply, but often, this signals the development of pathology. An examination of the pulmonary and cardiovascular systems is necessary.
Volume of liquid for gastric lavage
| Age | Single (ml) | Total (ml) |
| Newborn | 15-20 | 100 |
| 1 – 6 months | 60-100 | 500 |
| 7-12 months | 110-150 | 1000 |
| 2-5 years | 200-350 | 3000-5000 |
| 6-10 years | 350-450 | 6000-8000 |
| 11-15 years | 450-600 | 6000-10000 |
| Adults | 5-10 ml/kg | 2-5-10x |
How often should babies breathe in their sleep?
Indicators of the rhythm and frequency of breathing during night sleep differ from the values at the time of wakefulness. Infants, during rest, may experience periodic breathing (discussed below) or apnea (stopping breathing for 10-15 seconds with a frequency of repetitions of at least 15 times within 1 hour).
At the moment of sleep, the whole body rests (muscles and nervous system relax, heart rate slows down), as a result, oxygen consumption decreases, as a result, the frequency and depth of inhalations and exhalations decreases. If you are in doubt whether the child is breathing or not, you can determine the presence of breaths by the rise and fall of the ribs or peritoneum.
It is not recommended to wake up the child every 5-10 minutes. This will harm his nervous system.
In the presence of apnea in premature infants, parents are advised to monitor the rhythm of breathing. Sometimes the baby cannot resume the breathing process during sleep due to muscle relaxation. It is recommended to wake the child, if there is no reaction, urgently call emergency help , and additionally take the necessary measures to restore the respiratory process.
As you grow older, the rhythm and frequency of breathing during sleep stabilizes. In rare cases, these deviations are observed in adults.
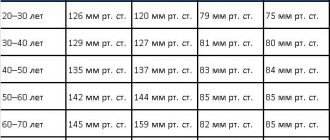
Arterial pressure
Blood pressure (BP) is one of the few health markers that can be measured at home. Today, almost every family has a device for independently measuring blood pressure. But not all adults know that the norm for children differs from the “120 to 80” we are all used to.
MedVedik reminds that blood pressure depends on the age of the baby. The younger the child, the lower his normal blood pressure. This is due to the fact that the child’s circulatory system and heart continue to develop after birth, so initially the child’s blood vessels and capillaries have less tone than those of adults.
Keep this helpful sign with BP limits for children. These are generalized indicators that are the result of many years of research. They correspond to the working pressure of 95% of healthy children.
Have you noticed a significant discrepancy in the child’s blood pressure readings and in the table? This is already a reason to see a doctor. He will calculate an individual rate specifically for your child and, if necessary, select treatment.
PS By the way, to obtain an accurate measurement result, the size of the tonometer cuff is important. A large cuff on a small child's hand may distort the readings somewhat.
Causes of decreased breathing rate
Factors that reduce the frequency of inhalation and exhalation can be natural or pathological:
| Natural processes | Pathological processes |
| Frequent attacks of apnea. | Injuries in the chest area. Perhaps damage to the lung tissue, or due to a bruise, the breathing process may be accompanied by severe pain, which will interfere with the normal breathing rhythm. |
| Strong relaxation of the respiratory muscles during sleep. | Damage to brain cells responsible for the respiratory reflex. |
| Physiological feature of the body (rare breathing rate). | The presence of a foreign object in the respiratory tract. |
| Formation of the pulmonary system as the child grows up. | Damage or inflammation of the nerve cells that regulate the frequency of inhalation and exhalation. |
| Temperature drop | Violation of the condition or functioning of the bronchi. |
| Side effects from taking medications. | |
| Electric shock may slow down your breathing. | |
| Poor blood supply, swelling or tumor formations in the brain affecting the functioning of the respiratory system. | |
| Spinal injury. There may be a disruption of the nerve cells that regulate the performance of the muscle tissue responsible for respiratory contractions. | |
| Severe poisoning of the body with poisons. There is a malfunction in the functioning of all organs and systems. | |
| Atrophy of muscle tissue as a result of paralysis or prolonged muscle inactivity. | |
| Curvature of the spine or rickets with subsequent deformation of the chest. | |
| Pathological processes in the cardiovascular system. |
Video on what to do if a child is holding his breath:
Whether a violation of the breathing process is a pathology or a natural process can be determined through regular monitoring of the child and a full examination by a pediatrician and pulmonologist.
Why are indicators changing?
If indicators change outside of diseases (for example, due to overheating), then after the end of the external factor they return to normal in 3-7 minutes. A constantly increased heart rate occurs when:
- viral, bacterial infection;
- blood acidification (acidosis);
- anemia (decreased hemoglobin and red blood cells);
- diseases of the bronchi and lungs with respiratory failure (for example, asthma, severe pneumonia);
- increased thyroid function (hyperthyroidism, thyrotoxicosis);
- tumors of the adrenal medulla (pheochromocytoma);
- the use of drugs that stimulate the heart (Eufillin, Atropine, asthma medications, hormones);
- autonomic dysfunction (neurocirculatory dystonia), more often developing in adolescents;
- inflammation of the heart - myocarditis, endocarditis, pericarditis;
- valve defects, large vessels, ventricular and atrial septal defects;
- tuberculosis;
- congenital disorders of the structure of the conduction system of the heart (for example, Wolff-Parkinson-White syndrome).
A slow heart rate is characteristic of increased intracranial pressure (tumor, cerebral edema, sinus thrombosis), severe malnutrition (hypotrophy), renal failure, viral hepatitis, typhoid fever. It may appear during the recovery period after an infectious disease.
The most severe decrease in heart rate occurs when conduction blockade in the myocardium occurs. In a child, such arrhythmia leads to rapid loss of consciousness. Children usually tolerate a moderately accelerated rhythm better.
The respiratory rate increases when:
- bronchospasm or inflammation (bronchial asthma, bronchitis);
- fever;
- lung diseases - pneumonia, tuberculosis, compression due to fluid accumulation in the pleural cavity, tumors;
- blockage of a branch of the pulmonary artery by a thrombus, embolus (thromboembolism);
- chest pain;
- diseases of the nervous system, hysteria;
- severe anemia;
- heart failure due to myocarditis, heart disease;
- fullness of the stomach, bloating.
A decrease in respiratory rate occurs with a brain tumor, edema, or inflammation of the meninges (meningitis). The cause may be severe failure of the kidneys, liver, acute onset of diabetes from a coma, or poisoning.
What does rapid breathing in children mean?
The frequency of inhalation and exhalation may deviate upward from age-related norms, also due to the influence of natural and pathological factors. This pathology occurs more often in children, since they cannot yet regulate the breathing process normally.
| Natural processes | Pathological processes |
| The air is too dry, hot, rarefied (found in the mountains). | Having a runny nose. Congestion and swelling of the nasal passages occurs. As a result, the child is forced to perform frequent breathing processes through the mouth. |
| Exercising and brisk walking. | Bronchial diseases. As a result, oxygen supply to tissues deteriorates. The brain sends signals to increase the breathing rate. |
| Excitement, fear or crying in a child. | Increased body temperature due to infection. |
| Clogged nasal passages with crusts of waste mucus. | Impaired functioning of brain cells due to injury, the presence of a tumor, or impaired blood supply. |
| Heavy weight of the child. For the normal functioning of all organs, more oxygen is required. | Tumor formations (of any nature) in the respiratory system. |
| Individual features of the functioning of the pulmonary system. | Chest injury. The pain prevents you from taking deep breaths, as a result the child switches to frequent, shallow breathing. |
| Overheating of the body | Impaired functioning of the cardiovascular system. Due to poor blood circulation, the body lacks oxygen. The brain sends signals to increase it (respiration rate increases). |
| Colic in the digestive tract. The pain does not allow me to breathe deeply. Less painful frequent and shallow breathing. | |
| Disruption of the functioning of the nervous system, areas responsible for the rhythm and depth of breathing. | |
| Presence of bronchial asthma. | |
| Due to the action of allergens. | |
| Increased levels of toxins or poisoning from poisons or medications. | |
| Side effects of drugs. | |
| Lack of iron in the blood. As a result, in order to sufficiently supply tissues with oxygen, the respiratory rate increases. |
Respiratory rate in children: the norm should be checked by a pediatrician during a monthly examination and compared with indicators according to the child’s age
In the absence of natural factors affecting the respiratory process, the child must be examined by a pediatrician.
What is periodic breathing, is it dangerous?
Periodic disturbances in the rhythm and depth of breathing are possible in 4 types:
- Cheyne-Stokes. This type is characterized by initially rare and shallow breathing with a gradual increase in inhalation amplitude and depth. When the maximum threshold is reached, the frequency and depth of inspiration gradually decreases, after which an interval of up to 1.5 minutes is possible. Then the process is repeated.
- Biotta. Rhythmic breathing is interrupted by pauses of 30 seconds or more.
- Kussmaul. The breathing process is accompanied by deep but rare breaths and accompanied by noise.
- Grocco. Breathing occurs according to the Cheyne-Stokes type, but instead of pauses there is shallow, weak breathing.
These types of respiratory processes cause harm to both adults and children:
- in children there is a disruption in the development of the respiratory system;
- Oxygen starvation of tissues and organs periodically occurs, which affects their performance. This is a decrease in the functioning of the brain, cardiovascular and nervous systems;
- the development of pathologies in these systems is possible, as well as deterioration of hearing, vision and the presence of constant headaches;
- there is a regular feeling of weakness. At the peak of rapid breathing, loss of consciousness is possible due to an excess of oxygen. At the peak of low breathing, fainting is possible due to lack of oxygen;
- Metabolic processes are disrupted, which leads to a delay in the child’s development (mental, weight and physical).
If pathological breathing is detected in a newborn or an older child, it is recommended to contact a pediatrician for an examination. The specialist will also explain how to behave to parents during prolonged respiratory arrest and the rules for emergency care before the ambulance arrives.
Relationship between breathing rate and heart rate
Respiratory rate in children (the norm by age is often measured together with the heart rate) and heart rate at rest:
| Age indicator | Range of values | |
| Breathing frequencies | Heart rates | |
| From birth to 14 days | 40-60 | 110-160 |
| From 15 days to 3 months | 40-45 | 135-160 |
| From 3 to 6 months | 30-40 | 130-140 |
| Over 6 months and up to a year | 30-35 | 105-155 |
| From 1 year to 2 years | 30-35 | 100-150 |
| From 2 to 3 years | 25-35 | 95-150 |
| From 3 to 4 years | 25-30 | 90-145 |
| From 4 to 5 years | 20-30 | 85-130 |
| From 5 to 7 years | 20-25 | 80-125 |
| From 7 to 10 years | 18-25 | 70-115 |
| From 10 to 14 years old | 18-20 | 65-105 |
| From 14 to 18 years old | 16-20 | 60-95 |
When the heart rate changes, the breathing process is disrupted and vice versa.
Rapid and slow breathing with a normal pulse
An increase or decrease in the respiratory rate value with normal pulse values is possible with the following deviations:
- individual physiological characteristics of the child’s body;
- poor indoor air quality (hot, dry, polluted);
- age-related changes in the child’s body;
- the presence of colic in the digestive tract;
- clogging of the respiratory tract (dried mucus).
These causes are not pathological in nature and go away on their own, without medical intervention. If in doubt, you should be examined by a pediatrician.
With an accelerated heart rate
An increase in the number of heart contractions is accompanied by a change in breathing rate.
Factors causing the violation:
- physical activity, running, as well as stress, fear or increased anxiety;
- increased body temperature due to overheating;
- disruption of the cardiovascular and respiratory systems;
- when an infection enters the body;
- severe poisoning by toxins and poisons;
- side effects from taking medications;
- development of oncology;
- presence of internal or external bleeding;
- entry of a foreign object into the respiratory tract. The body prevents normal breathing, and due to fear, the heart rate increases.
These symptoms (increased or decreased respiratory rate along with an increase in the number of heartbeats) require contact with specialists (pediatrician, pulmonologist, cardiologist) for examination.
With a slow heartbeat
When the heart beats slow down, the breathing process is disrupted in the following cases:
- pathological processes in the cardiovascular system;
- disruption of brain cell activity;
- electric shock;
- when the body is hypothermic;
- the effect of infection;
- side effect from taking medications.
Reduced heart rate and respiration rates are observed in children involved in sports. If a child does not engage in sports activities, then a change in indicators means the development of pathologies. An examination is required.
Clinical symptoms of poisoning
| Substance | Symptoms |
| Atropine (belladonna, henbane, datura) | Dilated pupils that do not respond to light. Hyperemia, dry skin and mucous membranes. Tachycardia. Hyperthermia. Hallucinations, convulsions. |
| Vapors of gasoline, kerosene, turpentine | Icteric skin. Shortness of breath, hemoptysis. Cyanosis. Cramps. |
| FOS | Constriction of the pupils. Pallor, hypothermia. Hypersalivation, bronchorrhea. Breathing problems. Stomach ache. Bradycardia, arterial hypotension. Cramps. |
| Saltpeter, nitrates | Diffuse cyanosis that does not improve after oxygen therapy. Dyspnea. Tachycardia. Cramps. |
| Carbon monoxide | Headache, dizziness. Chest pain. Cough. Vomit. Hyperthermia, then pallor. Convulsions, paresis and paralysis. Pulmonary edema. |
| Mushrooms: | Latent period from 6 to 24 hours. Stomach ache. Vomit. Cholera-like enterocolitis. Delirium, adynamia. Collapse. Coma. |
| Pale grebe (phalloin, phalloidin, amanite) | |
| Fly agaric (muscarine, muscaridine, etc.) | Latent period 1-2 hours. Drooling, nausea, abdominal pain, vomiting, diarrhea. Constriction of the pupils, difficulty breathing. Visual disturbances, delusions, hallucinations. Coma. |
| String, morel (galveolic acid) | Latent period 1/2-2 hours to 6 hours. Gastroenteritis. Hemolytic anemia, jaundice. Hematuria. |
Dependence of breathing rate on body temperature
The respiratory rate in children (the norm for age is a conditional indicator, since in diseases and certain characteristics of the body, breathing is often rapid or slow) depends on body temperature.
Until the child reaches 2 months, with an increase in temperature, only an increase in the respiratory rate occurs, the heartbeat remains normal. After the child reaches 2 months, both indicators increase. This reaction of the body is due to the protective and regenerative reaction of the body.
How to normalize your breathing rate
To restore breathing rate you need:
- during the period of night rest, take a horizontal position on your back, but at the time of an attack it is not recommended to put the child on your back;
- change your diet by increasing the amount of fresh vegetables and fruits;
- perform breathing exercises with the child for 15-20 minutes 3 times a day (slowly inhale through the nose, exhale through the mouth);
- in a playful way, breathe with the child into the bag and inflate the balloons;
- if the attack is caused by fear or stress, then you need to give children's sedatives or herbal decoctions;
- in the absence of breathing (during a prolonged attack of apnea), you need to rouse the child, let him smell ammonia (carefully so as not to burn the nasal mucosa). Sometimes it is recommended to hold the baby upside down for 1-3 minutes. In this case, you need to spank the baby on the buttocks. After this, splash the child’s face with cold water or wash it.
If the breathing rate is severely impaired, emergency assistance must be called.
Medicines, except for sedatives in liquid form, should not be given to a child until the symptoms are eliminated and the cause is determined. Normalization of the frequency of inhalation and exhalation in children varies by age towards a decrease in the indicator. If there are deviations, it is recommended to contact a pediatrician to determine the cause of the breathing disorder. Self-medication is unacceptable.
Author: Kotlyachkova Svetlana
Article design: E. Chaikina