The only way to know if you have high or low blood pressure is to measure your blood pressure. Understanding your results is key to controlling your blood pressure.
- Systolic blood pressure (First or top number) is the maximum pressure in the arteries when the heart contracts and pushes blood into the arteries.
- Diastolic blood pressure (Second or lower number) - shows the pressure in the arteries at the moment the heart muscle relaxes, it reflects the resistance of peripheral vessels.
Which number is more important?
Typically, more attention is paid to systolic blood pressure (the first number) as the main risk factor for cardiovascular disease for people over 50 years of age. For most people, systolic blood pressure rises steadily with age due to the loss of elasticity of the large arteries, an increase in heart rate, and the development of vascular disease.
However, an elevated systolic or elevated diastolic blood pressure value can be used to diagnose high blood pressure. The risk of death from coronary heart disease and stroke doubles with a 20 mmHg increase in systolic blood pressure. Art. or diastolic by 10 mm Hg. Art. among people aged 40 to 89 years.
Causes of headaches with normal blood pressure
In most cases, headache is observed at values of 125 to 70 in patients for whom these parameters are not normal. One of the causes of pain can be hypoxia, when brain cells experience oxygen deficiency, aching pain localized in the occipital and temporal regions.
Headaches can be a manifestation of hypertonicity of the cervical muscles, which causes spasm of the blood vessels that supply nutrition to the brain
In hypertensive patients, headache occurs against the background of vascular spasm and circulatory disorders. The pain syndrome is shooting and aching in nature with localizations in the occipital, frontal and temporal regions with irradiation to the bridge of the nose.
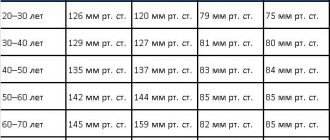
Blood pressure ranges
In our country, we adhere to the standards of the European Society for the Study of Hypertension, and there are also recommendations from the Ministry of Health of the Russian Federation dated 2021, which established the following ranges of numbers:
- Normal - systolic blood pressure less than 120-129 mmHg, diastolic blood pressure less than 80-85 mmHg.
- Highly normal - systolic blood pressure 130-139 mmHg, diastolic blood pressure 85-89 mmHg.
- 1st degree – 140-159/90-99 mmHg.
- 2nd degree – 160-179/100-109 mmHg.
- 3rd degree – more than 180/110 mmHg.
Note: The diagnosis must be confirmed by a doctor. Hypertension is a disease or diagnosis, and hypertension is the very fact of increased blood pressure. Your doctor may also evaluate any unusually low blood pressure readings and associated symptoms.
Normal pressure
- Optimal blood pressure is SBP less than 120 mmHg. Art. and/or DBP less than 80 mm Hg. Art.
- Normal blood pressure is pressure in the SBP range of 120–129 mmHg. Art. and/or DBP 80–84 mm Hg. Art.
If your results fall into this category, stick to heart-healthy habits such as a balanced diet and regular exercise.
High blood pressure
High blood pressure is when the readings are consistently in the range of above 140 mmHg for systolic and for diastolic more than 90 mmHg. Art. Measures must be taken to control this condition.
Hypertension 1st degree
Stage 1 hypertension is when blood pressure constantly fluctuates systolic between 140–159 and/or diastolic above 90–99 mmHg. Art. During this stage of high blood pressure, doctors may recommend lifestyle changes and may consider taking blood pressure medications. What you do next depends on your risk and risk factors for atherosclerotic cardiovascular disease (ASCVD), such as heart attack or stroke.
Hypertension 2 and 3 degrees
Stage 2 hypertension is when blood pressure is constantly at the level of 160/100 mmHg. or higher. During these stages of high blood pressure, doctors may prescribe a combination of blood pressure medications and recommend immediate lifestyle changes.
Hypertensive crisis
This stage of high blood pressure requires medical attention. If your blood pressure reading suddenly exceeds 180/120 mmHg. Art., wait five minutes, and then check your blood pressure again. If your readings are still unusually high, contact your doctor immediately. You may be experiencing a hypertensive crisis.
If your blood pressure is above 180/120 mmHg. Art. and you are experiencing signs of possible organ damage, such as chest pain, shortness of breath, back pain, numbness/weakness, changes in vision or difficulty speaking, do not expect pressure relief. Call 103
What to do to normalize the indicators?
Minor deviations in blood pressure that negatively affect the human body can be associated with stress, nervousness, and changes in weather conditions. The result is tachycardia, bradycardia, and headache. Treatment in this case is prescribed with the aim of normalizing the functioning of the nervous system.
The following treatment regimen is used:
- B vitamins (strengthen the walls of arteries, serve as the prevention of heart and vascular diseases).
- Sedatives (to normalize sleep, take at night).
To maintain stable blood pressure, additional magnesium intake is prescribed, which helps strengthen the nervous system.
A blood pressure of 120 over 70 is considered normal for some people, but for others it brings a feeling of discomfort due to the development of negative symptoms. A specialist will help assess the normal limits by determining not only the recorded level on the tonometer, but also identifying risk factors and the presence of chronic diseases.
Symptoms of low blood pressure
Most doctors consider chronic low blood pressure to be dangerous only if it causes noticeable signs and symptoms, such as:
- Dizziness
- Nausea
- Fainting
- Dehydration and unusual thirst
- Lack of concentration
- Blurred vision
- Cold, clammy, pale skin
- Rapid breathing
- Fatigue
- Depression
A single deviation from normal blood pressure readings is not a cause for concern unless you are experiencing any other symptoms.
How often should you measure your blood pressure?
If a person associates poor health with high blood pressure, to confirm this fact it is necessary to measure it for several days in a row, repeatedly during the day at approximately the same hours - usually in the morning and evening, unless a different frequency of measurements is recommended by the doctor. It is recommended to take 2-3 measurements at a time with an interval of 2-3 minutes.
Daily blood pressure measurements are also recommended in other cases. These include:
- first identified fact of increased blood pressure;
- changing the treatment regimen for arterial hypertension (changing drugs or their dosage);
- increased blood pressure during antihypertensive therapy;
- cardiovascular diseases, in addition to arterial hypertension;
- taking medications for other diseases that may affect blood pressure levels.
Diagnostics
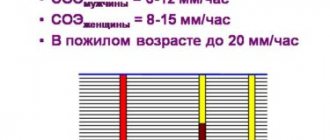
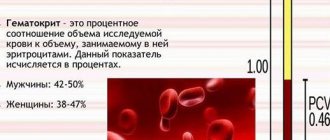
The diagnostic algorithm for men and women is standard; after collecting an anamnesis, physical examination, and consultation with specialized specialists (if necessary), the following is carried out:
- tonometry with calculation of pulse difference;
- UAC, OAM, biochemistry;
- 24-hour blood pressure monitoring;
- ECG, EchoCG, cardio-ultrasound;
- Dopplerography of the vessels of the neck, head;
- blood testing for hormones;
- Ultrasound of the kidneys.
Additionally, any laboratory or instrumental examination may be prescribed to determine the cause of pathological fluctuations.
conclusions
Hypertension is a leading cause of cardiovascular mortality and morbidity, but clinical BP measurements alone underestimate its prevalence in healthy individuals considered normotensive at these levels (66). We argue that CST BP measurements serve as a complementary assessment for clinical and outpatient assessment of hypertension and CVD risk, diagnosis, and prognosis. However, this approach is still hampered by the unreasonableness of previously proposed values and the lack of empirical diagnostic indicators of BP. To facilitate accurate classification of normal and excessive BP responses, existing guidelines need to be reinterpreted. Clinically significant abnormalities in BP response should be defined in terms of the rate of change in BP relative to workload or cardiac output in addition to peak values obtained during exercise. It is important to note the modulating influence of age, gender, level of training, health status and medications taken, which may be a consequence of an adaptive state (higher level of training), and not a connection with pathology. Finally, without positive clinical results, there is no need to stop CNT at high blood pressure thresholds, since there is no scientific evidence that such a reaction is associated with adverse events.
Source:
https://link.springer.com/
How to relieve the condition at home?
If pulse pressure increases or decreases, you must call an ambulance. It is impossible to normalize the condition and help the patient at home.
Before the ambulance arrives, you must follow the general recommendations:
- You should not take pills for hypertension or hypotension without a doctor’s prescription; taking medications not according to indications can lead to a worsening of the condition; before prescribing medications, the doctor will conduct a comprehensive examination, determine the cause of the disease, the severity of the problem, and then draw up a therapeutic treatment plan;
- if pulse pressure is disturbed, the patient should not be allowed to drink or eat, this can lead to loss of consciousness and involuntary vomiting; in this state, the patient may choke on vomit;
- to normalize the condition, you need to take a comfortable position, calm down, take a few deep breaths and exhales, think about the good;
- in the room you need to open a window or window to ensure the flow of fresh air into the room, you need to remove tight clothes from your body, unfasten the collar.
Upon arrival of the ambulance team, you must describe your condition in detail, as well as follow all the recommendations of medical workers. Specialists will provide first aid and decide whether hospitalization is necessary.
Why does pulse pressure drop?
Low pulse pressure is the difference between the upper and lower values of less than 40 units. In this case, doctors diagnose isolated arterial hypotension.
The causes of low human pulse pressure are always caused by pathologies:
- Ischemic nephropathy caused by vascular stenosis. Pulse pressure is regulated by biochemical mechanisms. The body produces the enzyme renin, which regulates vascular tone and the blood supply system. When kidney function is impaired, an imbalance occurs in metabolism, organ nutrition, and synthesis. This leads to a change in the glomerular filtration rate, impaired blood flow, and general destabilization. If left untreated, the condition can worsen and lead to a heart attack or severe kidney failure. Due to disorders occurring in the kidneys, the arterial value increases, which is reflected in the pulse value.
- Myocardial infarction. In case of acute disruption of blood supply, tissues and cells die. This is reflected in the value of pulse pressure, which decreases sharply. arterial parameters also drop to critical values.
- Extreme degree of left ventricular failure. Due to a sharp decrease in arterial parameters, failure develops in the left ventricle of the heart muscle. Factors influencing the development of the disorder are different: from aortic valve stenosis to a heart attack. Without medical intervention, a person can die.
- Heavy bleeding. Blood loss leads to a sharp drop in blood and pulse pressure. This is a protective reaction of the body, which tries to preserve tissue nutrition. Internal organs and vital systems do not receive sufficient nutrition and blood supply, which can lead to necrosis.
- Decompensation of chronic heart failure.
- Damage to the hypothalamus.
- Vegetovascular dystonia.
- A sharp decrease in cardiac output and cerebral ischemia.
A sharp decrease in pulse blood pressure can lead to death, so therapeutic intervention is required.
The lower the pulse pressure indicator, the greater the problems with the person’s condition it indicates
Symptoms of abnormalities
Deviations from the average pulse pressure can be determined by the appearance of characteristic symptomatic signs:
- pain in the head: throbbing pain in the back of the head in time with the heart rhythm;
- dizziness: loss of orientation in space, vestibular disorders, vertigo;
- vomiting: reflex vomiting, which does not bring relief, the feeling of nausea is caused by insufficiency of cerebral blood supply;
- increased sweating: the body receives false signals that force it to start thermoregulation, it produces more sweat due to imaginary cooling;
- clouding of consciousness: disorientation, auditory and visual hallucinations, memory loss, prosopagnosia;
- blue discoloration of the skin around the mouth;
- speech impairment, unintelligibility;
- unsteady gait;
- paralysis, lack of coordination of movements.
These are the main symptoms of dangerous pulse pressure that occur most often. The list of disorders is much wider.
What can be suspected if the indicator is low and what tactics should be taken in such a case?
A small difference between systolic and diastolic pressure means a deterioration in the pumping function of the heart, a decrease in stroke volume, which leads to hypoxia of organs and tissues. That is why low pulse pressure is often accompanied by the following symptoms:
- dizziness;
- drowsiness;
- weakness;
- headache.
A one-time deviation with a quick return to normal is not dangerous, however, a systematic decrease in PP may indicate the presence of the following diseases:
- vegetative-vascular dystonia (VSD);
- myocarditis;
- stenosis of cardiac or vascular valves;
- coarctation of the aorta
- shock of various origins (hypovolemic, cardiogenic);
- cardiosclerosis;
- impaired blood supply to the kidneys;
- myocardial hypertrophy.
What to do?
As in the previous case, it is critical to determine the exact cause of the decrease in PP. It is necessary to undergo a detailed examination, including laboratory tests, electrocardiography, ultrasound and other methods.
Depending on the specific disease, the cardiologist will prescribe certain medications or, if necessary, surgical treatments. A low blood pressure is considered a significant indicator of heart failure, which requires taking it very seriously.
Features of treatment
Deviations of normal blood pressure in any direction require identification of the root cause of the pathology and its elimination (relief). Without this, treatment is either useless or dangerous, since what helps with one disease can cause death in another.
Minor fluctuations in blood pressure do not require any intervention. They are most often one-time and physiological: temperature changes, climate zone changes, physical or psychological overload. The maximum that needs to be done is to consult a cardiologist in case of recurring abnormalities.
The doctor can prescribe folic acid - vitamin B9, which will support the heart and eliminate overload. The vitamin is produced by intestinal microflora and is responsible for cell growth and DNA preservation. During hyperloads, it is not enough, therefore, to stabilize the immune system, metabolic processes, and vascular elasticity, additional supply from the outside is necessary.
Patients with extra pounds and high pulse pressure are prescribed diuretics to normalize the total volume of circulating blood: from Furosemide, Diacarb, Hypothiazide to Triampur, Veroshpiron, Spironolactone. The treatment regimen is strictly individual, depending on the degree of obesity, blood pressure levels, and concomitant pathology.
In the presence of atherosclerosis, statins are added that normalize cholesterol metabolism: Atorvastatin, Rosuvastatin, Pitavastatin. They use nicotinic acid (niacin, vitamin PP, vitamin B) - a lipid-lowering agent, ion exchange resins (hemodialysis) or bile acid sequestrants: Cholestyramine, Colestipol, which reduce low-density lipoproteins that can destroy the arterial wall.
Age-related myocardial degeneration is stopped by prescribing cardiac glycosides: Digoxin, Celanide, Strophanthin. To reduce the diastolic index, Papaverine, calcium inhibitors: Amlodipine, Norvasc, Lacidipine, antispasmodics: Platiphylline, Scopolamine, Spazgan are prescribed.
To maintain vital functions, adrenergic drugs are used: Isadrin, Dobutamine, Dopamine. They act quickly, but only for a short time. For acute heart failure - intravenously - Amrinon and Milrinone.
Hormone replacement therapy can be used, and in extreme cases, surgical intervention: heart disease, aneurysms, total vascular atherosclerosis.
Danger of pathology
Fluctuations in pulse pressure are dangerous for the development of fatal complications in men and women, such as:
- acute heart failure resulting in stroke or heart attack;
- chronic heart failure with symptoms of stagnation in the systemic and pulmonary circulation, dystrophy of internal organs;
- myocardial ischemia;
- pre-fainting, traumatic fainting;
- acute and chronic kidney failure;
- dementia, vascular psychoses, Alzheimer's disease;
- visual impairment.
To prevent such conditions, timely diagnosis and preventive treatment are needed.
Generalization and directions for further research
Many clinicians express concern when the SBP response exceeds the “normal” range, but in such cases there is insufficient empirical evidence to make clinical recommendations. Moreover, arbitrarily set upper blood pressure values for stopping CST have the same drawback. We argue that the clinical utility of BP measurements can be improved under the following conditions:
In addition to the maximum/peak values obtained with CST, consider the rate of change of BP (slope of the curve), and establish the level of agreement between these two measurements.
Possibility of influence of age, gender, health status, medications and CST protocol on blood pressure values obtained in the test.
Standardize BP measurements as recommended by Sharman and LaGerche (1):
- Measure at the end of each CST step.
- Measure before ending the test, and if not possible, immediately after stopping the test.
- Use an automated device that can measure on the move (65). This limits interobserver variability. Prefer DBP data from auscultatory devices over oscillometric devices. However, caution is needed as there is little reliable data on these devices, mostly from small studies of healthy people.
- Manual measurements are suitable for experienced assessors. There are no empirical data to inform the threshold effects of training, but regular BP measurement during exercise is likely to be more beneficial than sporadic BP measurement.
Future studies should record and report BP values at which acute cardiovascular events occur during CST to properly assess risk and establish evidence-based upper limits.
First aid
It is impossible to stop a large or small pulse difference on your own; an ambulance is needed. Before her arrival:
| With high blood pressure | At low pressure |
| Do not take any medications unless previously approved by your doctor | |
| Do not drink or eat anything (fainting, vomiting, aspiration of vomit), you can take sedative drops: Corvalol, Valocordin, Valerian | Eat something salty, drink a couple of glasses of water, a cup of coffee, green tea |
| Take a comfortable position, open the windows for oxygen flow, loosen tight clothes | |
| Carry out tonometry, record the results for the doctor | Tonometry every 10 minutes with accurate recording |
The doctor may suggest hospitalization, the patient has the right to refuse, but it is more reasonable to stop the attack inpatiently, under the supervision of specialists.
Diet is an important factor in the fight against high blood pressure
A healthy lifestyle can work wonders. Some reduction in systolic (upper reading) blood pressure can be achieved by increasing physical activity, losing excess weight, and changing your eating strategy.
- Sodium, which is the main component of table salt, negatively affects kidney function and contributes to an increase in diastolic (lower) pressure. Therefore, limiting salt to 5 grams daily helps normalize the levels. Try to gradually replace NaCl with spices and herbs that have a beneficial effect on the body. They promote the removal of toxins and suppress the growth of pathogenic microflora.
- Hypertensive patients with extra pounds are advised to limit the consumption of fats, smoked and fried foods, and easily digestible hydrocarbons (sweets, potatoes, etc.).
- Food should be taken several times a day in small portions, without overeating and giving preference to lean meat and fish, cereals, low-fat fermented milk products, vegetable and low-fat meat soups, fresh vegetables and fruits.
- Products with a high content of potassium and magnesium will be extremely useful - fresh apricots, dried apricots, apples, etc.
- It is very important to limit the consumption of alcohol, which reduces the effectiveness of antihypertensive drugs.
- The effect of caffeine on blood pressure has not been fully studied. But it is known that an increase in blood pressure by 5-10 points after a cup of coffee may indicate high sensitivity to caffeine. Therefore, you should not abuse the aromatic drink.