The value of normal hematocrit in humans
The body of a healthy adult contains approximately 4.5-5 liters of blood. It contains formed elements and cells - red blood cells, platelets, leukocytes, as well as a liquid part called plasma.
Some blood components, for example, red blood cells, do not have all the necessary components of a human cell, losing them during the maturation process. Therefore, red blood cells and platelets are called blood cells, not cells.
In different categories of patients, the normal values of various parameters of the blood tested will differ. So, for most men, the hematocrit will be higher: 40-41%, and in some cases it can reach up to 51%, which is due to its slower renewal.
In healthy women, the hematocrit usually ranges from 36 to 42%. This is due to physiological features - due to regular menstrual bleeding, blood is renewed more often to replenish its volume. During pregnancy, from the 20th week, the indicator begins to decrease, which is also not considered a deviation.
In children, hematocrit differs at different age periods:
- 44-62% for newborns;
- 32-43% for babies up to three months;
- 36-43% for children under one year of age;
- 35-47% (up to 52% for boys) - in the first ten years.
In subsequent years, the hematocrit norm depends on gender and practically corresponds to the values of an adult.
Norms
The normal hematocrit level depends on the age and gender of the person. For a mature woman it is 37-50%, for a man 34-45%. For newborns, this figure may be higher and ranges from 35 to 65%. As people grow older, the hematocrit decreases, reaching minimal levels in the elderly. This is the result of decreased bone marrow activity and decreased production of blood cellular elements.
A decrease in normal hematocrit in women is associated with regular blood loss during menstruation. High values in children are a manifestation of active processes in the development of red bone marrow and other hematopoietic organs.
It is important to consider that after massive blood losses and blood transfusions, determining the hematocrit level will give results with a large error. To reliably assess this indicator in such cases, it is necessary to wait a certain time.
It may take up to 3 months for complete physiological restoration of red blood cell levels to normal levels. This period is the life cycle of red blood cells, during which the cellular composition of the blood is renewed.
Methods for determining hematocrit
The indicator is determined as a percentage by calculating the amount of formed elements in whole blood. It is calculated using special instruments or manually.
Centrifugation using the Wintrobe method
The blood is exposed to centrifugal force for 10-30 minutes. The formed elements are heavier than plasma, so they settle to the bottom of the test tube. The hematocrit is determined by the ratio of sediment to the total volume of biomaterial.
Calculation of the indicator using the formula
The ratio of the number of red blood cells to the total blood volume can be calculated mathematically. To do this, the following indicators are required:
- total hemoglobin concentration (ctHB);
- red blood cell count (RBC);
- mean erythrocyte volume (MCV);
- mean erythrocyte hemoglobin concentration (MCHC).
The hematocrit number (HCT) is determined by one of the formulas:
- HCT (%)=(ctHB (mmol/l)*0.0485+0.0083)*100
- HCT (%)=0.1*MCV*RBC
- HCT (%)=ctHB/MCHC*100
Direct blood cell counting method
In a given volume of biomaterial, visible blood elements are counted manually or using hematological analyzers. The method is highly accurate, and the measurement process does not take much time - no more than five minutes, but the equipment required is very expensive.
Manual counting method
Blood collected using an anticoagulant is placed in a dry, clean tube and allowed to settle. In this case, the formed elements that have greater weight settle to the bottom of the container, and the light plasma rises to the top, forming two fractions of red and yellow colors, respectively. The hematocrit indicator can be determined by the divisions on the test tube. This method is the least accurate, its error is up to 20%, so it is currently not used in laboratories.
What is hematocrit
Our blood is one of many types of tissue in our body. Like any tissue, it consists of cells and intercellular substance. Its main feature is that it is liquid, the cells are not connected to each other and are free floating. Only in this form can blood perform its circulatory function.
Blood cells are red blood cells, leukocytes and platelets, with the main position here being occupied by red blood cells - erythrocytes. There are a thousand times more of them than leukocytes and platelets.
The liquid part of blood is plasma. It consists of 90% water, the rest being proteins and other organic and mineral substances.
The content of the liquid part in the blood is approximately 60%, the content of cells is respectively 40%.
So the percentage or volume content of cell mass in relation to plasma is the hematocrit. The term comes from the Greek roots hemat (blood) and krites (judge). Here we can talk about all blood cells or only red blood cells, which does not significantly change the essence of the concept (leukocytes and platelets occupy no more than 1% of the total cell mass).
It is determined either as a percentage or as a decimal fraction.
When is a hematocrit test performed?
Most often, hematocrit is determined as part of a general (clinical) blood test. Therefore, at present this parameter of a clinical blood test is not prescribed separately. The hematocrit level changes when:
- disorder of the blood coagulation system;
- dehydration;
- anemia or polycythemia;
- bleeding.
Assessing the hematocrit level is important when determining indications for the need for blood transfusion or the effectiveness of blood transfusion, during hemodialysis, and some operations. To determine the hematocrit number, venous or capillary blood is taken.
Indications and preparation for analysis
The hematocrit indicator is always indicated in the results of a general blood test. This means that it can be assessed:
- During any medical examination or mandatory medical examination.
- In preparation for surgery.
- During hospitalization and before discharge.
But besides this, there are certain indications when it is necessary to determine the hematocrit. In this case, a direct measurement is performed: the plasma is separated by centrifuging the material and an accurate indicator is obtained. Indications for this:
- Bleeding.
- Blood clotting problems
- Dehydration of the body.
- Anemia.
- Polycythemia.
In order to get a reliable result, you should refuse food 6-10 hours before taking blood from a vein or from a finger. As a rule, the analysis is taken in the morning. It is also necessary to avoid drinking alcohol 2-3 days and refrain from smoking 2-3 hours before the procedure.
Increased hematocrit
An increase in hematocrit occurs with an increase in the number of blood cells - polycythemia - and a lack of fluid in the body. An increase in the indicator may indicate serious diseases accompanied by blood thickening and thrombotic complications.
Causes
Hematocrit increases due to stress, taking corticosteroid drugs and diuretics, traumatic shock accompanied by intense pain, as well as when climbing to high altitudes, smoking, or playing sports using anabolic steroids to gain muscle mass.
An increase in the indicator may indicate the following diseases:
- dehydration due to vomiting, profuse diarrhea, overheating or heat stroke, excessive sweating, insufficient fluids;
- heavy bleeding in the midst or immediately after it stops;
- pathologies accompanied by a decrease in blood plasma volume, for example, peritonitis, thrombosis, diabetes, burn disease;
- renal dysfunction - hydronephrosis, oncology, polycystic disease;
- vitamin B12 or iron deficiency anemia;
- leukemia;
- erythrocytosis;
- defects and coronary heart disease, heart failure;
- intestinal obstruction;
- bronchial asthma, pulmonary emphysema, obstructive bronchitis.
Symptoms
An increase in blood viscosity leads to thrombus formation. The latter can manifest itself in the form of tingling or various pains and numbness in the limbs. If the cause of increased blood viscosity is not determined in time, serious complications such as myocardial infarction, stroke, gangrene and even death may develop.
Treatment
Treatment is carried out not for the changed hematocrit level itself, but for the conditions or diseases that caused these changes. In some situations, when serious causes for a slightly changed hematocrit level have been excluded, no treatment is required. But usually such situations are short-lived, in the case of physiological reasons for changes in hematocrit levels.
How does increased hematocrit manifest?
An increase in the specific gravity of red blood cells may not manifest itself in any way, or there may be individual, completely nonspecific symptoms:
- headache;
- dizziness;
- feeling of pressure in the head;
- dyspnea;
- fast fatiguability;
- skin itching;
- redness of the skin.
With such symptoms, a person may not see a doctor for a long time, but the problem may grow and lead to serious consequences.
See: Thick blood, Why I'm always cold, Complete blood count.
Decreased hematocrit
A decreased hematocrit occurs when the number of red blood cells or their size decreases - erythrocytopenia. The cause may also be the accumulation of water in the body when the blood becomes thinner - hyperhydration, as well as hyperproteinemia or the accumulation of proteins in the plasma, which contributes to fluid retention.
Causes
A decrease in hematocrit is facilitated by prolonged immobility, fasting or a strict diet, taking anticoagulants and antiplatelet agents, and intravenous infusions in large volumes; heavy drinking, chronic alcoholism, excessive salt intake, menstruation in women.
Also, a downward change in the indicator may indicate the following pathologies:
- iron-, B12- or folate-deficiency anemia;
- severe bleeding;
- impaired hemoglobin production in sickle cell anemia;
- fibrous degeneration of the liver - cirrhosis;
- disruption of the urinary system;
- hemolysis of erythrocytes - destruction of red blood cells due to hereditary mutation, autoimmune processes or toxic effects on blood cells;
- malaria, typhoid fever;
- oncological diseases of the bone marrow or its metastatic lesions from other organs;
- an increase in the amount of protein in plasma due to vomiting, diarrhea, blood cancer and other conditions.
During pregnancy, a decrease in hematocrit can be observed in the case of toxicosis, a very young age of the mother, multiple pregnancies, a short period of time between pregnancies, and also after the 20th week of gestation due to a physiological increase in fluid in the body.
Symptoms
A decrease in hematocrit in the blood is accompanied by hypoxia of various organs, since it is the red blood cells that normally carry oxygen throughout the body. This condition is manifested by the following symptoms:
- fast fatiguability;
- general weakness;
- drowsiness;
- increased heart rate and breathing;
- feeling of lack of air;
- headache, dizziness;
- decreased memory and concentration;
- hair loss;
- marbling or pallor of the skin.
Increased Ht in diseases
The causes of pathological growth of Ht are various diseases that can be divided into three categories:
- diseases in which the amount of plasma in the blood decreases;
- kidney diseases, in which the body’s ability to absorb fluid is reduced or there is increased synthesis of a hormone that promotes the production of blood cells;
- malignant diseases associated with pathological changes in red blood cells, as well as their quantity and intensity of formation.
A high hematocrit with intense production of erythropoietin, which enhances the maturation of red cells, is observed in the following cases:
- with ischemic kidney disease, which can be observed with polycystic diseases, tumors, hydronephrosis, traumatic shock;
- when undergoing a course of treatment with glucocorticosteroids;
- in stressful situations;
- for anemia (iron deficiency, B12 deficiency, folate deficiency);
- for erythremia caused by bone marrow pathologies.
To obtain more reliable results, hematocrit calculation is carried out in modern hemoanalyzers
An increased hematocrit may occur when plasma volume decreases, while red cell and hemoglobin levels remain normal. This occurs in the following conditions:
- peritonitis, or inflammation of the peritoneum;
- burns, 10 percent of them are deep and 15% are superficial;
- pulmonary insufficiency associated with COPD (chronic obstructive pulmonary disease);
- chronic cardiac failure, accompanied by edema and accumulation of large amounts of fluid in the abdominal cavity (ascites);
- late toxicosis during pregnancy;
- diabetes.
Causes of high hemoglobin
Increased level of hemoglobin in the blood in women, what is it? If this indicator changes, it means that there is a problem with a specific organ and system. Although sometimes high hemoglobin is the norm - for example, in people who live in the mountains or in elevated areas. The main reasons why high hemoglobin occurs in women are as follows:
- Hemoglobin often increases in those who smoke, as well as in those who have recently been in a fire. The fact is that hemoglobin easily transports air or carbon dioxide, replacing them with each other.
- A high level of water deficiency raises blood counts, resulting in an increase in the amount of circulating plasma.
- Congenital heart disease caused by high pressure in the pulmonary artery blood flow. In this situation, the skin color changes from infancy and has a blue tint. The child coughs frequently and has shortness of breath. Ultrasound of the heart allows you to determine an accurate diagnosis. Treatment of such pathologies with severe symptoms is only surgical.
- Pulmonary diseases.
- Excessive amounts of vitamins B6 and B12 in the human body.
- Cancerous neoplasms.
However, a high level of hemoglobin in the blood can not only indicate various diseases, but also signal that you lead a different lifestyle and live in an unfavorable place.
increased hemoglobin in women
General clinical blood test
It is carried out as part of a general clinical examination of the patient and allows you to learn about the condition of the blood and the body as a whole. The main indicators of this analysis are: hemoglobin, the number of leukocytes (white blood cells), erythrocytes (red blood cells) and platelets (nuclear-free plates of blood responsible for clotting).
Due date and how to prepare
A general blood test is taken in the morning on an empty stomach, often from a finger, less often from a vein. You should not drink or eat 4 hours before the test.
Metrics collected
Now a general blood test is carried out on automatic hematological analyzers, which can simultaneously determine values from 5 to 24 parameters.
The main indicators collected are:
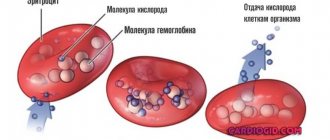
- Hemoglobin (HGB - hemoglobin)
- the main component that is involved in the transfer of oxygen in the blood from the lungs to organs and tissues, and carbon dioxide back to the lungs, is the blood pigment of red blood cells. - Red blood cells (RBC - red blood cells)
are red blood cells that carry oxygen in the blood to organs and tissues. - Leukocytes (WBC - white blood cells)
are white blood cells produced in the bone marrow that carry out immune control and protect the body from foreign cells. - Thrombocytes (PLT - platelets)
are nuclear-free platelets of blood responsible for clotting. - Lymphocytes (LYM - lymphocyte)
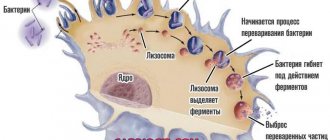
are cells of the immune system that respond to viruses and microbes. - Monocytes (MON - monocyte)
are large cells of the immune system. - Hematocrit (HCT - hematocrit)
is the volume of red blood cells in the blood. - Blood color index (BI)
, demonstrating the concentration of hemoglobin in red blood cells. - Erythrocyte sedimentation rate
, which, if deviated from the norm, may indicate a pathological condition of the body. - Various erythrocyte, leukocyte and platelet indices
.
Decoding the results: norm and deviation
The normal values of the blood parameters studied in each laboratory are different and depend on the gender, age and condition of the patient. Only a doctor can make a correct interpretation of the blood test results and make a diagnosis, taking into account all aspects of the patient’s health. Below are frequently examined blood parameters, their normal values, and what a deviation from the norm may indicate in the general case, and not in the specific case. To obtain an individual interpretation and diagnosis, you should consult a doctor.
Hemoglobin (HGB - hemoglobin)
Normal hemoglobin level in blood:
Men:
- from 12 to 15 years: 120 - 160 g/l;
- from 15 to 18 years: 117 - 166 g/l;
- from 18 to 45 years: 132 - 173 g/l;
- from 45 to 65 years: 131 - 172 g/l;
- over 65 years old: 126 - 174 g/l.
Women:
- from 12 to 15 years: 115 - 150 g/l;
- from 15 to 18 years: 117 - 153 g/l;
- from 18 to 45 years: 117 - 155 g/l;
- from 45 to 65 years: 117 - 160 g/l;
- over 65 years old: 120 - 161 g/l.
Children:
- up to 2 weeks: 134 - 198 g/l;
- from 2 to 4.3 weeks: 107 - 171 g/l;
- from 4.3 to 8.6 weeks: 94 - 130 g/l;
- from 8.6 weeks to 4 months: 103 - 141 g/l;
- at 4 to 6 months: 111 - 141 g/l;
- from 6 to 9 months: 114 - 140 g/l;
- from 9 to 1 year: 113 - 141 g/l;
- from 1 year to 5 years: 100 - 140 g/l;
- from 5 years to 10 years: 115 - 145 g/l;
- from 10 to 12 years: 120 - 150 g/l;
Deviation of hemoglobin in the blood from the norm may indicate:
when decreasing by:
- overhydration - increased water content in the body due to impaired water-salt metabolism;
- anemia - disruption of the oxygen transport function in the body and the development of hypoxia.
when increasing by:
- dehydration - loss of water in the body;
- polycythemia vera - increased blood viscosity and decreased blood flow;
- excessive smoking.
Red blood cells (RBC - red blood cells)
Norm of red blood cells in the blood:
Men:
- from 12 - 18 years: 4.5 - 5.3 * 10^12/l;
- over 18 years old: 4.0 - 5.0 * 10^12/l.
Women:
- from 12 - 18 years: 4.1 - 5.1 * 10^12/l;
- over 18 years old: 3.5 - 4.7 * 10^12/l.
Children:
- newborn: 3.9 - 5.5 * 10^12/l;
- from 1 to 3 days: 4.0 - 6.6 * 10^12/l;
- in 1 week: 3.9 - 6.3 * 10^12/l;
- in week 2: 3.6 - 6.2 * 10^12/l;
- at 1 month: 3.0 - 5.4 * 10^12/l;
- in the 2nd month: 2.7 - 4.9 * 10^12/l;
- from 3 to 6 months: 3.1 - 4.5 * 10^12/l;
- from 6 months to 2 years: 3.7 - 5.3 * 10^12/l;
- from 2 to 6 years: 3.9 - 5.3 * 10^12/l;
- from 6 to 12 years: 4.0 - 5.2 * 10^12/l.
Normal erythrocyte indices:
- MCV
: 80 - 95 fl - average erythrocyte volume; - MCH
: 27 - 31 pg - average hemoglobin content in an individual red blood cell; - MCHC
: 320 - 360 g/l - average hemoglobin concentration in the erythrocyte mass; - RDW
: 11.5% - 14.5% - red blood cell distribution width; - RDW-SD
: 37 - 54 fl - deviation of the distribution of red blood cells by volume; - RDW-CV
: 11.5 - 14.5% (adults), 14.9 - 18.7% (children up to 6 months) and 11.6 - 14.8% (children over 6 months) - deviation of red blood cell size from averages; - P-LCR
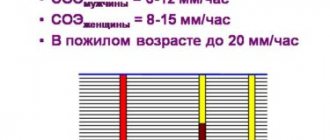
: 13 - 43% - large platelet ratio; - ESR
: 10 mm/hour (men), 15 mm/hour (women) - erythrocyte sedimentation rate, deviation of which from the norm may indicate a pathological or inflammatory process in the body.
Deviation of red blood cells from the norm may indicate:
when decreasing by:
- anemia;
- blood loss;
- pregnancy;
- overhydration;
- decrease in the intensity of red blood cell formation in the bone marrow;
- therapy with diuretics;
- accelerated destruction of red blood cells.
when increasing by:
- burn;
- diarrhea;
- hydrocele of the renal pelvis;
- true polycythemia;
- Cushing's syndrome;
- neoplasms;
- steroid use;
- the effect of corticosteroids;
- taking diuretics.
Leukocytes (WBC - white blood cells)
Norm of leukocytes in the blood:
Men and women:
- from 16 years and older: 4.0 - 9.0 * 10^9/l.
Children:
- up to 1 year: 6.0 - 17.5 * 10^9/l;
- from 1 year to 2 years: 6.0 - 17.0 * 10^9/l;
- from 2 to 4 years: 5.5 - 15.5 * 10^9/l;
- from 4 to 6 years: 5.0 - 14.5 * 10^9/l;
- from 6 to 10 years: 4.5 - 13.5 * 10^9/l;
- from 10 to 16 years: 4.5 - 13.0 * 10^9/l.
Norm of leukocyte indices:
- LYM% (LY%)
: 25 - 40% - relative content of lymphocytes; - LYM# (LY#)
: 1.2 - 3.0 * 10^9/l (1.2-3.0 x 10^3/μl) - absolute lymphocyte content; - MXD% (MID%)
: 5 - 10% - the relative content of a mixture of monocytes, eosinophils and basophils; - MXD# (MID#)
: 0.2 - 0.8 * 10^9/l - absolute content of a mixture of monocytes, eosinophils and basophils; - NEUT% (NE%)
: 40% - 75% - relative content of neutrophils; - NEUT# (NE#)
: 2 - 7.5 * 10^9/l - absolute content of neutrophils; - MON% (MO%)
: 4 - 11% - relative content of monocytes; - MON# (MO#)
: 0.1 - 0.6 * 10^9 cells/l - absolute content of monocytes; - EO%
: 1 - 5% - relative content of eosinophils; - EO#
: 0.4 * 109/l - absolute eosinophil content; - BA%
: less than 1% - relative content of basophils; - BA#
: 0 - 0.08 * 10^9/l - absolute content of basophils; - IMM%
: 1 - 5% - relative content of immature granulocytes; - IMM#
: 1.2 - 6.8 * 10^9/l - absolute content of immature granulocytes; - ATL%
: less than 5% - the relative content of atypical lymphocytes; - ATL#
: 0.06 - 0.15 * 10^9/l - absolute content of atypical lymphocytes; - GR% (GRAN%)
: 47 - 72% - relative content of granulocytes; - GR# (GRAN#)
: 1.2 - 6.8 * 10^9/l (1.2 - 6.8 * 10^3/μl) - absolute granulocyte content.
Deviation of leukocytes in the blood from the norm may indicate:
when decreasing by:
- typhus;
- viral diseases;
- bone marrow diseases and damage;
- anaphylactic shock;
- leukemia;
- viral diseases;
- radiation sickness;
- Addison-Biermer disease;
- collagenosis;
- myelodysplastic syndromes;
- hypersplenism;
- myelofibrosis;
- plasmacytoma;
- taking certain antibiotics and anti-inflammatory drugs;
- anemia.
when increasing by:
- the presence of inflammatory processes in the body;
- sepsis;
- purulent processes;
- tissue injuries;
- myocardial infarction;
- infectious diseases;
- the presence of malignant neoplasms;
- last trimester of pregnancy;
- period of feeding the baby with breast milk;
- great physical activity.
Thrombocytes (PLT - platelets)
Normal platelet count in blood:
Men, women and children:
- all ages - 180 - 320 * 10^9 cells/l.
Normal platelet indices:
- MPV (mean platelet volume): 7 - 10 fL - average platelet volume;
- PDW: 9 - 16% - width of platelet distribution by volume;
- PCT (platelet crit): 0.108 - 0.282% - the proportion of blood volume occupied by platelets.
Deviation of platelets in the blood from the norm may indicate:
when decreasing by:
- bronchial asthma;
- malaria;
- thrombocytopenia;
- malignant neoplasm;
- Sumter's syndrome.
when increasing by:
- essential thrombocythemia
Lymphocytes (LYM - lymphocyte)
Norm of lymphocytes in the blood:
Men and women:
- from 16 years and older: 20 - 40%.
Children:
- newborns: 15 - 35%;
- up to 2 weeks: 22 - 55%;
- from 2 weeks to 1 year: 45 - 70%;
- from 1 year to 2 years: 37 - 60%;
- from 2 to 5 years: 33 - 55%;
- from 6 to 7 years: 30 - 50%;
- from 8 to 9 years: 30 - 50%;
- from 9 to 11 years: 30 - 46%;
- from 12 to 15 years: 30 - 45%.
Deviation of lymphocytes in the blood from the norm may indicate:
when decreasing by:
- autoimmune diseases;
- diseases of the nervous system;
- HIV infection;
- side effects from taking medications.
when increasing by:
- viral diseases;
- bacterial infections;
- fungal diseases;
- toxoplasmosis;
- tuberculosis;
- whooping cough;
- vasculitis;
- malignant neoplasms;
- initial stage of HIV;
- excess carbohydrates in the body compared to fats and proteins;
- thyroid diseases;
- starvation.
Monocytes (MON - monocyte)
Norm of monocytes in the blood:
Men and women:
- from 16 years and older: 3 - 9%.
Children:
- newborns: 3 - 12%;
- up to 2 weeks: 5 - 15%;
- from 2 weeks to 1 year: 4 - 10%;
- from 1 year to 2 years: 3 - 10%;
- from 2 to 5 years: 3 - 9%;
- from 6 to 7 years: 3 - 9%;
- from 8 to 9 years: 3 - 9%;
- from 9 to 11 years: 3 - 9%;
- from 12 to 15 years: 3 - 9%.
Deviation of monocytes in the blood from the norm may indicate:
when decreasing by:
- use of immunosuppressants;
- hereditary diseases.
when increasing by:
- stress;
- diabetes;
- atherosclerosis;
- bacterial infections;
- malignant neoplasms;
- sepsis;
- collagenosis;
- sarcoidosis
Hematocrit (HCT - hematocrit)
Hematocrit norm:
Men:
- from 12 to 15 years: 35 - 45%;
- from 15 to 18 years: 37 - 48%;
- from 18 to 45 years old: 42 - 50%;
- from 45 to 65 years: 39 - 50%;
- over 65 years old: 37 - 51%.
Women:
- from 12 to 15 years: 34 - 44%;
- from 15 to 18 years: 34 - 44%;
- from 18 to 45 years old: 38 - 47%;
- from 45 to 65 years: 35 - 47%;
- over 65 years old: 35 - 47%.
Children:
- up to 2 weeks: 41 - 65%;
- from 2 to 4.3 weeks: 33 - 55%;
- from 4.3 to 8.6 weeks: 28 - 42%;
- from 8.6 weeks to 4 months: 32 - 44%;
- from 4 to 6 months: 31 - 41%;
- from 6 to 9 months: 32 - 40%;
- from 9 to 12 months: 33 - 41%;
- from 1 year to 3 years: 32 - 40%;
- from 3 to 6 years: 32 - 42%;
- from 6 to 9 years: 33 - 41%;
- from 9 to 12 years: 34 - 43%.
A hematocrit deviation from the norm may indicate:
when decreasing by:
- pregnancy;
- anemia;
- children's age;
- hypoproteinemia;
- overhydration.
when increasing by:
- true polycythemia;
- hypoxia;
- kidney hydronephrosis;
- kidney neoplasm;
- polycystic kidney disease;
- peritonitis;
- burn disease;
- leukemia;
- dehydration.
Blood color index (BC)
Normal blood color index:
Men, women and children:
- all ages: 0.9 - 1.1.
A deviation of the blood color indicator from the norm may indicate:
when decreasing by:
- anemia;
- purulent infections;
- cirrhosis of the liver;
- tuberculosis;
- Iron-deficiency anemia;
- iron-saturated hypochromia;
- malignant neoplasms;
- thalassemia;
- microcytosis.
when increasing by:
- lack of vitamin B12;
- lack of folic acid;
- dysbacteriosis;
- chronic pancreatitis;
- stomach diseases;
- diseases of the small intestine;
- cirrhosis of the liver;
- long-term treatment with glucose-lowering drugs;
- long-term treatment with anti-tuberculosis drugs;
- poor nutrition.
When to take it
A general clinical blood test must be taken:
- As prescribed by a doctor;
- As a preventative measure to assess general health;
- As part of routine medical examinations and examinations.
How to reduce hemoglobin in the blood?
If what causes hemoglobin to rise has nothing to do with serious illnesses, then you can influence it with a specific diet or medications. Among the pharmaceutical medications that can be easily purchased at the pharmacy, there are those that are aimed at thinning the blood: Trental, Cardiomagnyl, Curantil, Aspirin. Only a doctor should prescribe them! To reduce hemoglobin at home, you need to adjust your diet:
- Drink plenty of fluids per day. To do this you need to drink warm water. If you cannot do this, then saline drips are used.
- Reduce fats, sweets, eggs, as they increase cholesterol and so in a viscous environment.
- You should not take multivitamins or products that contain copper and iron.
- It is better to choose shrimp, fish, white meat, nuts, legumes, and vegetables.
- Also limit your intake of foods that increase hemoglobin. This is food enriched with protein and iron - red meat, red fruits and vegetables, offal, fish roe, butter, buckwheat, sweets.
Now you know why increased hemoglobin appears in a woman .
Blood chemistry
A laboratory blood test that gives an idea of the condition of internal organs and their functionality. Allows you to evaluate metabolism and find out about the lack of microelements in the body.
Due date and how to prepare
A biochemical blood test is taken in the morning on an empty stomach from a vein. You should not eat 12 hours before the test. You can only drink clean water, but drinks, including tea, coffee and any others, are not allowed. 24 hours before the test you must give up alcohol, smoking and physical activity.
Metrics collected
- Glucose
- blood sugar level; - Urea
is a parameter important for assessing kidney function; - Cholesterol
is an element that determines the risk of cardiovascular diseases; - LDL cholesterol
is an element that determines the risk of cardiovascular disease; - HDL cholesterol
is an element that determines the risk of cardiovascular disease; - Residual blood nitrogen
is a parameter important for assessing kidney function; - Atherogenicity coefficient (Ka)
- shows the risk of developing atherosclerosis; - Total bilirubin
is an indicator that may indicate the presence of jaundice; - Total protein
is an indicator that allows you to evaluate liver function; - AST (AST)
is an indicator that allows you to evaluate the work of the heart; - AlAt (ALT)
is an indicator that allows you to evaluate liver function; - Lipase
is an indicator that allows you to evaluate the functioning of the pancreas; - Amylase
is an indicator that allows you to evaluate the functioning of the pancreas; - Gamma-GTP
is an indicator that allows you to evaluate liver function; - Antistreptolysin-O
is an indicator that is used in the diagnosis of rheumatism; - Rheumatic factor
is an indicator that is used in the diagnosis of autoimmune diseases; - CRP (C-reactive protein)
is an indicator that can indicate inflammation in the body; - Alkaline phosphatase
is an indicator of many different diseases and health problems; - Albumin
is a protein that performs many functions in the body; - General lipids
are fats that perform structural and regulatory functions in the body; - Triglycerides
are fats that perform structural and energy functions in the body; - Phospholipids
- an indicator that assesses the metabolism of fats in the body, indicating liver and kidney diseases, and indirectly diabetes mellitus; - Protein fractions
are indicators that may indicate inflammatory processes, infectious and other diseases in the body; - Calcium
is an important element for the nervous and cardiovascular systems; - Potassium
is an element that normalizes heart rhythm and regulates water balance; - Sodium
is an element that regulates the volume of extracellular fluid; - Chlorine
is an element that regulates the acid-base balance of the blood; - Iron
is an element important for binding, transporting and transmitting oxygen throughout the body.
Decoding the results: norm and deviation
The normal values of the blood parameters studied in each laboratory are different and depend on the gender, age and condition of the patient. Only a doctor can make a correct interpretation of the blood test results and make a diagnosis, taking into account all aspects of the patient’s health. Below are frequently examined blood parameters, their normal values, and what a deviation from the norm may indicate in the general case, and not in the specific case. To obtain an individual interpretation and diagnosis, you should consult a doctor.
Glucose
Norm
: 3.33 - 6.38 millimoles per liter;
Deviation
: May indicate diabetes mellitus or hypoglycemia.
Urea
Norm
: 2.5 - 8.3 millimoles per liter;
Deviation
: May indicate a kidney problem.
Cholesterol
Norm
: 3.6 mmol/l - 7.8 mmol/l;
Deviation
: may indicate obesity, endocrine disorders, genetic diseases and others.
LDL cholesterol (bad cholesterol)
Norm
: 2.02 - 4.79 mmol/l (men), 1.92 - 4.51 mmol/l (women);
Deviation
: Excess may indicate liver disease, kidney disease, obesity and other diseases.
HDL cholesterol (good cholesterol)
Norm
: 0.72 - 1.63 mmol/l (men), 0.86 - 2.28 mmol/l (women);
Deviation
: A decrease may indicate various diseases and poor nutrition.
Residual blood nitrogen
Norm
: 14.3 - 28.6 mmol/l;
Deviation
: May indicate a kidney problem.
Atherogenic coefficient (Ka)
Norm
: 14.3 - 28.6 mmol/l;
Deviation
: May indicate a kidney problem.
Total bilirubin
Norm
: 8.5 - 20.55 µmol/liter;
Deviation
: May indicate liver problems and jaundice.
Total protein
Norm
: 48 - 73 grams per liter (newborns), 47 - 72 grams per liter (children up to one year old), 61 - 75 grams per liter (from 1 to 4 years), 52 - 78 grams per liter (from 5 to 7 years) , 58 - 76 grams per liter (from 8 to 15 years), 65 - 85 grams per liter (adults);
Deviation
: May indicate liver problems or nutritional deficiencies.
AsAt (AST)
Norm
: 10 - 38 IU/l;
Deviation
: May indicate problems with the heart.
AlAt (ALT)
Norm
: 7 - 41 IU/l;
Deviation
: May indicate liver problems.
Lipase
Norm
: 0 - 190 units per 1 ml of blood (adults), 0 - 130 units per 1 ml of blood (children);
Deviation
: may indicate problems with the pancreas.
Amylase
Norm
: less than 53 U/l;
Deviation
: may indicate problems with the pancreas.
Gamma-GTP
Norm
: 15 - 106 µmol/l (men), 10 - 66 µmol/l (women);
Deviation
: may indicate problems with the liver and a number of other diseases.
Antistreptolysin-O
Norm
: less than 200 units;
Deviation
: May indicate rheumatism.
Rheumatic factor
Norm
: less than 14 IU/ml;
Deviation
: May indicate autoimmune diseases.
CRP (C-reactive protein)
Norm
: 0 - 10 mg/l;
Deviation
: May indicate inflammation in the body.
Alkaline phosphatase
Norm
: 20 - 140 IU/l;
Deviation
: Can indicate many different diseases and health problems.
Albumen
Norm
: 35 - 52 g/l;
Deviation
: Can indicate many different diseases and health problems.
General lipids
Norm
: 4 - 8 g/l;
Deviation
: Can indicate many different diseases, aging and diets.
Triglycerides
Norm
: 0 - 2.25 mmol/l;
Deviation
: may indicate pathology of internal organs.
Phospholipids
Norm
: 2.52 - 2.91 mmol/l;
Deviation
: may indicate liver and kidney diseases, and indirectly diabetes mellitus.
Protein fractions
Norm
: total protein 65 - 85 g/l;
Deviation
: may indicate inflammatory processes, infectious and other diseases in the body.
Calcium
Norm
: 2.15 - 2.50 mmol/l;
Deviation
: can lead to diseases of the nervous and cardiovascular systems and others.
Potassium
Norm
: 3.5 - 5.5 mmol/l;
Deviation
: can lead to diseases of the cardiovascular, muscular system and others.
Sodium
Norm
: 136 - 145 mmol/l;
Deviation
: may indicate a malfunction of the kidneys, liver, endocrine system and other body systems.
Chlorine
Norm
: 98 - 107 mmol/l;
Deviation
: may indicate metabolic disorders and other diseases.
Iron
Norm
: 8.95 - 30.43 µmol/l;
Deviation
: Can lead to disruption of various body functions.
When to take it
A biochemical blood test must be taken:
- As prescribed by a doctor;
- As part of routine medical examinations and examinations;
- To assess the functioning of internal organs and the functionality of the body;
- To determine the need for microelements;
- For information about metabolism;
- After suffering from infectious or somatic diseases.