According to statistical studies, 15% of menstruating women suffer from anemia of varying severity, and not every one of them notes signs of this insidious disease.
And among pregnant women, the percentage of those suffering from a lack of hemoglobin in the blood doubles, so during this period of a woman’s life it is important to regularly take blood tests to detect anemia.
Iron deficiency anemia is most often diagnosed when the hemoglobin protein contains an insufficient amount of iron. However, the human body is designed in such a way that when there is a lack of iron, internal reserves are primarily used, so anemia does not always manifest itself with characteristic symptoms in the initial stages of the disease.
The effect of hemoglobin on the female body
The main task of iron-containing protein is to supply every cell of the body with oxygen and, as a result, ensure the normal functioning of internal organs and systems. Hemoglobin production and menstruation are interdependent processes. For any woman, blood loss, including in the form of spotting, means a decrease in iron, the deficiency of which is dangerous:
- the occurrence of various types of skin pathologies;
- blood pressure disorders;
- rapid fatigue;
- brittle hair and hair loss;
- decreased immunity and, as a result, the body’s susceptibility to any infectious diseases;
- the appearance of problems of the reproductive system.
To avoid this effect, a few days before the onset of menstruation, the hemoglobin level rises sharply, which makes the blood more viscous and prevents heavy bleeding. The onset of menstruation is accompanied by a decrease in hemoglobin: the blood becomes liquid and gradually leaves the vagina. Such changes in the level of hemoglobin in the blood allow you to regulate the menstrual cycle. If the deviation exceeds any norms, this may contribute to a malfunction of some systems, including the reproductive system, and the menstrual cycle will be completely disrupted (there will be a delay or, conversely, premature bleeding).
Can hemoglobin decrease during menstruation? Undoubtedly. A decrease in the content of this protein in the blood is both a cause and a consequence of menstruation. A decrease in hemoglobin levels helps to dilate blood vessels and reduce the viscosity of blood secretions, as a result of which menstruation occurs normally. As menstruation progresses, the amount of hemoglobin in the blood will become even less, because it will leave the body along with menstrual mucus.
Why should you go to the gynecologist if you have anemia?
When diagnosing anemia in women, it is mandatory to visit a gynecologist and undergo appropriate diagnostic procedures: examination using gynecological mirrors, colposcopy, ultrasound of the uterus and, if necessary, tests. First of all, anemia can develop in a woman due to heavy menstruation, when a large amount of blood is lost during menstruation, and the menstruation itself lasts longer than usual. In this case, properly selected hormonal therapy aimed at regulating hormonal levels in the body can help. A test for sex hormones can help identify dishormonal disorders.
When identifying anemia in a woman, it is important to find the cause that provoked this disease. It is its elimination that will allow you to quickly get rid of the pathology. In women, the following diseases often lead to recurrent uterine bleeding, which can affect the amount of iron in the blood:
- endometriosis – proliferation of cells of the inner layer of the uterine mucosa, their localization in atypical tissues or organs;
- fibroids and polyps - benign neoplasms in the uterine cavity;
- malignant changes in the uterus and other female genital organs.
Timely detection of these diseases is a factor in their successful treatment and, as a result, relief from anemia, subject to an integrated approach to therapy.
How to determine hemoglobin level
The simplest and most common option is to go to the nearest clinic and get your blood tested. It is very important not to have breakfast on this day: this test must be taken in the morning and always on an empty stomach, 8-12 hours after the last meal. The doctor will take blood from your finger, after which it will be sent to the laboratory for testing. A few days later (sometimes on the day of the tests), you will be presented with a report - a form with the results, which will indicate the following data:
- hemoglobin concentration;
- total number of leukocytes and erythrocytes;
- ESR (erythrocyte sedimentation rate).
We need exactly the first indicator, which can be presented in the following units of measurement: g/l, U/l or µmol/l. A woman’s blood should be saturated with this substance within 120-140 grams per liter, but if you were tested during your period, lower concentrations are possible. Moreover, the norm of the same results of a general blood test for people of different ages will be different. Only a doctor can evaluate and decipher the results obtained, so you should not rely only on your own conclusions.
Please note that to identify problems in the body or any diseases, a general blood test is required over time. For preventive purposes, it is recommended to do this at least once a year, however, if any suspicion of certain diseases is detected, the doctor may prescribe and more frequent laboratory visits.
It is noteworthy that you can check the level of hemoglobin in your blood even at home. Similar to visits to the doctor, the patient should be tested on an empty stomach in the morning. To get accurate results, avoid smoking or drinking alcohol the day before, as well as exercising or exercising. Women planning to find out their hemoglobin content at home have several “tools” to choose from:
- Rack with test tubes and glass scale. The blood is sent into a test tube and diluted with hydrochloric acid. After a few minutes, the solution will acquire a new shade, after which you need to add distilled water (no more than 10-40 milliliters) to it. The results obtained are compared on the scale provided in the kit.
- Test strips. Read the instructions for use carefully and use one test strip from the package to find out the result.
Blood condition after menstruation
The state of the blood, or more precisely, the level of hemoglobin (the number of red blood cells) after menstruation is an important indicator of health. To make sure that the body is working normally or, on the contrary, there are some abnormalities, a woman can do a blood test for hemoglobin before and after the start of menstruation. During the normal functioning of all organs and systems of the female body, a cyclical change is observed within the permissible limits of the hormonal level. During critical days, it is not recommended to donate blood, since the result will probably not be entirely accurate: the hemoglobin level during menstruation is always underestimated, but from this indicator it is difficult to determine which -reasons for concern.
During critical days, the female body loses approximately 15–30 mg of iron. This is a normal phenomenon, which indicates that hemoglobin has decreased slightly. A pronounced change in the concentration of iron-containing protein is especially characteristic of women who have heavy periods or a long duration of menstruation (about 7 days). However, even in this case, a healthy body immediately makes up for the loss.
The only thing doctors recommend focusing on is the hemoglobin level after menstruation (whether it falls or, conversely, is above normal)
- The norm is considered to be a decrease to 110 g/l. If it is lower, this may indicate signs of anemia.
- In the absence of any pathologies, just a few days after menstruation, this figure increases to the usual figures for a woman - 120–140 g/l.
- Detection of hemoglobin concentrations above normal (about 150 g/l) is not uncommon among female smokers. It has been proven that tobacco tar activates this kind of protective reaction of red blood cells to avoid oxygen starvation.
To maintain the balance of blood cells, it is recommended to eat more iron-containing foods during menstrual periods. As a rule, 3-4 days after the start of menstruation, hemoglobin returns to normal. If a blood test is done after two weeks, but your hemoglobin levels are still low, you should consult a doctor. The manifestation of problems associated with abnormal blood conditions is evidenced by symptoms during menstruation such as a feeling of weakness, dizziness, nausea and difficulty in the gastrointestinal tract. The nature of the bloody discharge can also indicate a disorder: heavy and prolonged bleeding or, conversely, scanty and dark discharge - a signal that you urgently need to visit a gynecologist.
How dangerous is anemia for a woman from a gynecological point of view?
Anemia, if the start of treatment is delayed or the therapy is incorrectly selected, can seriously affect the functioning of the entire body. With this disease, the number of not only red blood cells in the blood decreases, but also leukocytes and platelets, which in turn inevitably leads to a decrease in immunity and even the development of immunodeficiency states. As a result, the woman begins to get sick often and for a long time.
Depression, low performance and chronic fatigue can provoke various neurological disorders. It becomes more difficult for such patients to concentrate, mental abilities decrease, and memory deteriorates. An advanced disease can negatively affect the functioning of the cardiovascular system; the load on the heart muscle increases significantly.
An important factor for women is the deterioration of appearance due to anemia. The disease affects the condition of the skin, hair, and nails. Dark circles under the eyes and pale skin become companions of iron deficiency anemia.
If gynecological diseases leading to anemia are not treated, a woman is at risk of developing infertility. Some changes in the uterus that provoke recurrent bleeding and, as a result, anemia, are irreversible if treatment is not started on time.
It is worth understanding that insufficient or excessive production of sex hormones in the female body can become a provocateur of diseases like a chain reaction. Therefore, in case of anemia, it is so important to undergo a full course of gynecological examination and make sure that women’s health is stable, and if any pathologies are detected, undergo a course of treatment in a timely manner and thereby improve overall well-being.
Low hemoglobin during menstruation
If the usual level of hemoglobin in a woman’s blood, even outside of menstruation, is very low, then she is probably familiar with painful sensations and extremely poor health on menstruation days. These representatives of the fairer sex, regardless of how much hemoglobin drops during menstruation, during menstruation regularly have to deal with:
- general weakness;
- nausea;
- dizziness;
- low labor productivity;
- other signs of poor health during menstruation.
As a rule, the menstrual cycle of these young ladies is longer than that of others, as a result of which menstruation days can drag on for a week or longer, not without pain and intense discharge. What is this connected with? It's simple. Low hemoglobin during menstruation and throughout the menstrual cycle indicates that the body does not have enough microelement such as iron, which means that fragility of blood vessels, in particular in the uterus, cannot be ruled out. If they are damaged, bleeding is observed for a long time, and additional blood loss only aggravates the situation: oxygen starvation - the risk of hormonal imbalance (so constant shifts in menstruation are also quite possible).
Does hemoglobin drop during menstruation if everything is in order with the body? If the situation is somewhat different, and outside of menstruation a woman has a normal hemoglobin concentration, and its decrease occurs only on critical days, this is absolutely normal. Doctors confirm this, calling this reaction a natural process. Moreover, on the eve of the planned menstruation, appetite often increases, so feel free to pamper your body with foods rich in:
- Iron. Products such as pork or chicken liver, beef or lamb meat, oysters, mussels and other seafood, as well as chicken yolk, lentils, peanuts, buckwheat and wheat bran are especially good in this regard.
- Vitamin B: Carrots, cauliflower, green vegetables, nuts, sardines, oatmeal and many other foods in your refrigerator are complete sources of B vitamins.
At the end of menstruation, low hemoglobin can remain stable for about a week, after which it quickly returns to normal without any treatment. All you need to do is ensure a healthy diet. The body should be monitored more closely if the level of iron-containing protein has decreased significantly - to 110 g / l or lower.
The relationship between hemoglobin levels and menstruation has long been proven scientifically. Firstly, the appearance of menstruation is caused by the fact that the uterus gets rid of the endometrium, as a result of which its renewed layer is formed. Secondly, each new menstrual cycle is accompanied by a shortage of new blood in the body, which must be replenished within seven or more days. In other words, low hemoglobin after menstruation or during menstruation is normal, although if even after two weeks nothing has changed or the protein concentration continues to decrease, you should be examined by a gynecologist.
High hemoglobin during menstruation
Excessive concentrations of iron-containing proteins in the body during or after menstruation affect only a small percentage of women and can be due to a variety of reasons. Symptoms in this case include:
- weak discharge during menstruation;
- sleep disturbance;
- frequent dizziness;
- pain in the heart area and more.
Such symptoms are the result of excessive oxygen content in the blood, which increases the load on many internal organs and, first of all, the heart.
The increased rhythm of its work causes pain and provokes disruptions in the menstrual cycle: menstrual periods may begin earlier than scheduled or on time, but with minimal discharge. It is very important that such signs do not recur many times, otherwise you subsequently risk complications in the form of serious diseases: in addition to increased blood pressure and a significant change in blood viscosity, vascular thrombosis may occur, cholesterol plaques may form, and even myocardial infarction may occur. Thus, if your hemoglobin level increases during or after your period, doctors may prescribe special medications to thin the blood: this allows you to resume menstruation and prevent complications.
There are often situations when women are looking for independent ways to quickly increase hemoglobin: the menstrual cycle for these young ladies is extremely difficult, since constant weakness does not allow them to work normally or do any other things. In some cases, representatives of the fairer sex even resort to medical help, although quite often it is enough to simply eat as many foods containing iron as possible between menstrual periods.
How can a woman understand that she has anemia: symptoms and signs of anemia
Symptoms of this disease can manifest themselves in various conditions, ranging from malfunctions of the cardiovascular system to distortion of tastes and smells. But first of all, a woman should be concerned about the most specific signs for this condition, which most often accompany anemia:
- decreased labor activity;
- causeless weakness;
- darkening of the eyes;
- fatigue and apathy;
- depression;
- changes in the menstrual cycle;
- prevalence of bad mood;
- cold fingers;
- tendency to eat chalk, clay, toothpaste, raw cereals, etc.
It is worth paying close attention to your appearance. Often women explain their external changes by other reasons and do not always think about the fact that a serious disease, such as anemia, can greatly affect their appearance. So, it is recommended to consult a good gynecologist if external signs of anemia appear:
- pale, flabby, dry skin, sometimes with a greenish tint;
- haggard appearance;
- hair and nails are brittle, dull;
- White stripes or dots may appear on the nails, the nail plates themselves become concave;
- Trophic wounds appear on the tongue, which manifests itself as pain when eating salty and spicy foods.
It is worth urgently undergoing an examination if the above symptoms are accompanied by loss of consciousness, pain in the heart, shortness of breath, urinary incontinence or numbness of the extremities. Such manifestations may indicate advanced anemia that requires immediate treatment.
Normal hemoglobin during menstruation
It is well known that the norm of hemoglobin outside menstruation can vary from 120 to 140 g/l. The only exceptions are athletes or those who like to lift weights in the fitness room: for them this figure can easily reach 160 g/l, and this is not a sign of pathology. A deviation can also be observed in those who smoke: in this case, the protein concentration increases to 150 g/l.
A natural phenomenon is considered to be similar to other days of the menstrual cycle or reduced hemoglobin during menstruation: the norm is about 110-130 g/l, depending on the age of the woman. In particular, we present to your attention the average hemoglobin indicators by age, which are called normal:
- maturing organism (11-15 years) - 110-130 g/l;
- young girls (15-18 years old) - 115-135 g/l;
- girls aged 18 years and older - 120-140 g/l.
With large blood loss or prolonged menstruation, this indicator can be at the level of 105-115 g/l, which is understandable from a physiological point of view.
Young mothers whose hemoglobin level drops to a minimum level deserve special attention: to 110 g/l during the first and third trimester, and also to 105 g/l during the second. It is believed that pregnancy is proceeding normally if this indicator does not exceed 120 g/l. This is due to the fact that carrying a baby is accompanied by a more active consumption of iron, which goes towards the formation of the placenta and the development of the embryo. Moreover, the volume of blood in a woman’s body during pregnancy increases by at least 50%, due to which the bone marrow performs its functions slowly and cannot provide the blood with hemoglobin in the usual amount.
Iron deficiency conditions in gynecological diseases and methods for their correction
Iron deficiency anemia (IDA) is a hematological syndrome characterized by impaired hemoglobin synthesis due to iron deficiency. Anemia is based on tissue hypoxia, which develops as a result of a decrease in the amount of hemoglobin due to blood loss, impaired formation of red blood cells, their destruction, or a combination of these reasons [1, 2].
Iron deficiency occurs in almost 1/3 of the world's inhabitants, and iron deficiency anemia accounts for 80–90% of all anemias. The prevalence of anemia varies depending on gender, age, climatic-geographical and environmental-industrial causes [1, 3, 4].
A corresponding deficiency develops when iron losses exceed iron intake of 2 mg/day, and is observed in various physiological conditions and diseases [5, 6].
Iron deficiency (hypochromic, microcytic) anemia usually occurs due to a decrease in iron resources in the body due to chronic blood loss or insufficient external iron supply.
The most vulnerable to the development of iron deficiency are women of reproductive age due to monthly physiological blood loss during menstruation, pregnant women due to their high need for microelements, children and adolescents due to the high needs of a growing body, elderly people suffering from chronic diseases and having poor nutrition.
Iron is an essential microelement that plays an important role in the functioning of cells in many body systems, the main of which is the participation of iron in the processes of tissue respiration. The total amount of iron in a woman’s body reaches 2–3 g, and its concentration is 40–50 mg per kg of body weight.
There are two types of iron: heme and non-heme. Heme iron is part of hemoglobin, is found only in meat products, is easily absorbed, and its absorption is practically not affected by the composition of food.
Non-heme iron is found in free ionic form - ferrous or ferric iron. The absorption of non-heme iron (found primarily in vegetables), which accounts for up to 90% of the iron in the total diet, depends on a number of factors. The main part of iron is included in hemoglobin and myoglobin - 70%; iron depot - 18% (intracellular accumulation in the form of ferritin and hemosiderin); functioning iron - 12% (myoglobin and iron-containing enzymes); transported iron - 0.1% (iron bound to transferrin) [7–9].
The most important iron-containing compounds include: hemoproteins, the structural component of which is heme (hemoglobin, myoglobin, cytochromes, catalase, peroxidase), non-heme enzymes (succinate dehydrogenase, acetyl-CoA dehydrogenase, xanthine oxidase), ferritin, hemosiderin, transferrin.
In the mucous membrane of the small intestine, only divalent non-heme iron is absorbed from food. In order for iron to contact proteins and enter the cell, ferric iron is reduced to divalent iron in the presence of an acidic environment; in most cases, ascorbic acid plays the main role in this process [10–13]. Then, to enter the blood plasma and bind to transferrin, iron is again oxidized to trivalent. In the transferrin-bound state, iron is delivered to tissues through endocytosis, where it is either utilized by the cell or deposited in ferritin. Ferritin stores iron in an easily accessible and non-toxic form. Ferritin level is the “gold” standard indicator of the amount of stored iron in the body. Each microgram of ferritin corresponds to 8 mg of deposited iron and for women is normally 15–150 mg/ml [2, 14–16]. The concentration of serum iron is subject to significant daily fluctuations and averages 6.6–26 µmol/l in women. Therefore, its definition is not of paramount importance [2].
Hemoglobin is an oxygen transport protein containing heme iron. The hemes are combined into a protoporphyrin framework, in the center of which there is one divalent iron atom. One hemoglobin molecule can carry a maximum of 4 oxygen molecules. Thus, the number of red blood cells and hemoglobin plays an important role in oxygen transport [2].
During iron deficiency, successive stages are distinguished: latent iron deficiency, in which iron losses exceed iron intake without changes in hemoglobin concentration, and iron deficiency anemia itself, which, depending on the severity, is divided into compensated, subcompensated and decompensated forms [3].
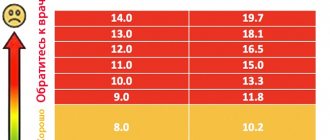
Hemoglobin concentration is expressed in grams per liter. The normal hemoglobin level in women is considered to be 115-145 g/l (MCHC, Mean Corpuscular Hemoglobin Concentration - the average concentration of hemoglobin in a cell is 320-360 g/l); anemia is indicated when hemoglobin decreases below 110 g/l. The severity of anemia is judged by the level of hemoglobin. According to the severity of anemia, there is a mild degree - 90-109 g/l, a moderate degree - 70-89 g/l and a severe degree - less than 70 g/l [3, 14, 15].
In addition, iron deficiency anemia is characterized by a decrease in hematocrit, hypochromia (MCH, Mean Corpuscular Hemoglobin - the average absolute content of hemoglobin in one erythrocyte), microcytosis (MCV, Mean Corpuscular Volume - the average volume of an erythrocyte), hyposiderosis (a decrease in the amount of serum iron, an increase in total iron-binding ability of blood serum, decrease in ferritin level in blood serum and in hemolysate) [3, 5]. The number of red blood cells, hematocrit and hemoglobin constitute the measured values, and MCV, MCH, MCHC are derivatives of these values [2].
The clinical picture of anemia is caused by oxygen starvation of tissues, progressive hemic hypoxia with the subsequent development of secondary metabolic disorders. Clinical symptoms appear as the severity of the disease increases: general weakness, dizziness, headache, palpitations, shortness of breath, fainting, decreased performance, insomnia. Symptoms characteristic of IDA include changes in the skin, nails, hair, muscle weakness, and distortion of the sense of taste. The skin becomes dry and cracks appear on it. Due to impaired carotene metabolism, iron deficiency causes yellowness of the skin. The shape of the nails changes, they flatten, become concave and brittle. Hair becomes thinner, breaks and falls out profusely, and gray hair appears. With IDA, symptoms of damage to the cardiovascular system are also possible: palpitations, shortness of breath, chest pain and sometimes swelling in the legs [6, 14].
The main compensatory mechanisms are circulatory and ventilatory adaptation, including an increase in cardiac output, vasodilation, a decrease in vascular resistance, an increase in tissue perfusion, blood redistribution, an increase in minute volume of respiration, and an increase in erythropoietin activity. Acute, severe and uncompensated anemia can lead to circulatory collapse and shock [2].
The main cause of the development of iron deficiency anemia in women is blood loss of various etiologies. Iron deficiency is 6 times more common in women than in men. A significant amount of blood is lost during menstruation, pregnancy, and childbirth. With heavy menstruation, iron loss of 50–250 mg of iron is possible [2]. Most often, hyperpolymenorrhea is associated with the presence of uterine fibroids, adenomyosis, hyperplastic processes of the endometrium, and dysfunctional uterine bleeding. Metrorrhagia with uterine fibroids is most often associated with submucosal localization of nodes, in which the menstrual surface increases, the permeability of blood vessels supplying the fibroids increases, and the contractility of the uterus decreases. With fibroids, the regeneration of the bleeding surface of the uterus slows down after desquamation of the endometrium. With adenomyosis, the uterine myometrium is affected, which leads to prolonged heavy menstruation and secondary iron deficiency anemia.
Menstrual irregularities occur in women at different ages. Various reasons can lead to the development of hypermenstrual syndrome - severe emotional shocks, malnutrition, vitamin deficiencies, obesity, occupational hazards, infectious and septic diseases, immaturity of hypothalamic structures in puberty and involutive changes in premenopause. In a significant proportion of cases of menometrorrhagia in women, they are accompanied by anemia of varying severity, which contributes to the development of trophic disorders in various organs and tissues. Prevention and treatment of anemia in women with menstrual irregularities and organic gynecological diseases are the most important factors in restoring their health [1, 4, 17].
Regardless of the cause of menometrorrhagia (fibroids, endometriosis, ovarian dysfunction) and the need to influence the corresponding factor, long-term therapy with iron preparations for oral administration is required. The dose, dosage regimen and specific drug are selected individually, taking into account the iron content in the drug, its tolerability, etc.
When choosing a specific drug and the optimal dosage regimen, it is necessary to keep in mind that an adequate increase in hemoglobin levels in the presence of IDA can be ensured by the intake of 30 to 100 mg of ferrous iron into the body [18]. Dietary measures alone cannot compensate for iron deficiency and achieve a therapeutic effect.
Antianemic therapy should be carried out with oral medications and should not be stopped after hemoglobin normalization. Indications for parenteral administration are quite limited: intestinal pathology with malabsorption, intolerance to oral drugs, social reasons (use in patients with personality changes, the mentally ill). According to many studies, parenteral forms do not have advantages over oral ones, and a large number of serious side effects are noted [4, 10, 19]. Blood transfusions for IDA should be carried out only for health reasons.
Modern oral ferrous preparations are salts of ferrous iron (ferric ions are not absorbed in the digestive tract) or compounds consisting of a hydroxide-polymaltose complex of ferric iron (the absorption mechanism differs from that of ionic preparations) [20].
Ferric sulfate salt has the highest bioavailability, therefore ferrous sulfate is mainly contained in ferrous preparations [19, 21]. Ferrous sulfate is the most studied, proven form, which has proven itself with long-term use, therefore it is most often included in preparations for oral administration. It has the highest degree of absorption of all iron preparations.
In the process of absorption of divalent iron in the intestine, ascorbic acid is of great importance, which helps maintain iron in divalent form, so its presence in the preparation is very important [22]. In hematopoiesis, folic acid plays a significant role, enhancing nucleic acid metabolism. For normal folic acid metabolism, cyanocobalamin is necessary, which promotes the formation of its active form. Deficiency of these substances, which often occurs in anemia associated with blood loss, leads to disruption of DNA synthesis in hematopoietic cells, while the inclusion of these components in the drug increases the active absorption of iron in the intestine and its further utilization. The presence of ascorbic and folic acids, as well as cyanocobalamin in the drug significantly increases the rate of hemoglobin synthesis and increases the effectiveness of therapy for iron deficiency conditions and iron deficiency anemia [14, 23, 24].
The listed components that increase the bioavailability of iron are part of the complex antianemic drug Ferro-Folgamma® [24], which was developed and produced in accordance with the recommendations of the World Health Organization (1998).
1 capsule contains 112.6 mg of ferrous sulfate (elemental iron 37 mg), which is the optimal dose for therapy and reduces the incidence of side effects.
Absorption of iron from salt preparations (Fe2+) occurs in the form of passive diffusion according to a concentration gradient, does not depend on pH and motor activity of the gastrointestinal tract (GIT), which ensures rapid saturation.
Ascorbic acid improves the absorption of iron in the intestine, prevents its transition from divalent to trivalent form, accelerates the transport of iron and its inclusion in heme, and also participates in the process of releasing iron from the depot.
Ascorbic acid is necessary for the formation and preservation of the reduced form of folic acid - tetrahydrofolic acid.
In turn, folic acid is an essential factor for the synthesis of DNA and RNA, protein metabolism and the formation of red blood cells, and also acts as an additional stimulator of erythropoiesis and hematopoiesis [21, 23, 25].
Cyanocobolamine is necessary for the formation of hemoglobin, red blood cells, metabolism of proteins, fats, carbohydrates, and energy production.
Ferro-Folgamma® is highly effective, providing an average increase in hemoglobin of 2.5 g/l/day (the highest rate of increase in hemoglobin among ferrous sulfate preparations). When using the drug Ferro-Folgamma®, a weakening of the clinical symptoms of posthemorrhagic anemia is observed during the first 10 days of use [6].
Ferro-Folgamma® is prescribed 1 capsule 3 times a day after meals for 3–4 weeks for mild forms of anemia, for moderate forms — 1 capsule 3 times a day for 8–12 weeks, and for severe forms of anemia — 2 capsules 3 times a day for 16 weeks or more. During pregnancy, it is prescribed to prevent folic acid and iron deficiency, 1 capsule 3 times a day in the II and III trimesters, in the postpartum period during breastfeeding.
After cessation of treatment with Ferro-Folgamma®, the positive effect and stabilization of blood serum parameters (hemoglobin level, red blood cells, serum iron, total iron-binding capacity of blood serum) are guaranteed to persist for at least one month [4].
The active components of Ferro-Folgamma® are in a special neutral shell, which ensures their absorption in the upper part of the small intestine, which eliminates irritating effects on the stomach. The components are dissolved in rapeseed oil, which improves the absorption of iron and at the same time reduces the irritating effect of iron on the gastric mucosa, promoting good tolerability of the drug in the digestive tract [1, 13]. Due to the absence of an aggressive effect on the gastrointestinal mucosa, Ferro-Folgamma® can be successfully used to correct anemic syndrome, with a deficiency of vitamin B12 and folic acid against the background of impaired absorption in the gastrointestinal tract (atrophy of the gastric and duodenal mucosa).
In addition, Ferro-Folgamma® is effectively used for combined iron-folate-B12-deficiency anemia caused by chronic blood loss, chronic alcoholism, infections, taking anticonvulsants and oral contraceptives, anemia during pregnancy and breastfeeding.
The effectiveness of Ferro-Folgamma® for the treatment and prevention of iron deficiency anemia with good tolerability and favorable pharmacoeconomic characteristics (cost/iron dose/efficacy) was proven in several Russian studies that included a wide range of patients, including pregnant women and women with gynecological diseases [4, 18, 19]. Indications for the use of the drug Ferro-Folgamma® are anemia caused by a combined deficiency of iron, folic acid and vitamin B12, occurring against the background of chronic blood loss (menorrhagia and metrorrhagia, etc.), as well as with chronic alcoholism, infectious diseases, taking anticonvulsants and oral contraceptives. The drug is approved for the prevention and treatment of iron and folic acid deficiency in the second and third trimesters of pregnancy, in the postpartum period and during lactation.
Thus, anti-anemic therapy using the drug Ferro-Folgamma® with optimal iron content is highly effective with a rapid increase in hemoglobin (complete clinical and hematological remission in 93% of patients after 3 weeks of therapy). There is good tolerability - the absence of side effects in 95% of patients, allergic reactions and negative effects on the body of women, as well as the stability of the results achieved and the maintenance of a positive effect for a month after treatment, which makes it possible to recommend the drug Ferro-Folgamma® to a wide range of patients.
Literature
- Transcript of the scientific symposium “Iron deficiency conditions in obstetrics and gynecology.” III Russian Forum “Mother and Child”. M., 2001, 29.
- Hook R., Breiman K. Anemia during pregnancy and the postpartum period. M., 2007, 74.
- Gorodetsky V.V., Godulyan O.V. Iron deficiency conditions and iron deficiency anemia: diagnosis and treatment. Guidelines. M.: Medpraktika-M, 2005; 28.
- Konovodova E. N., Dokueva R. S.-E., Yakunina N. A. Iron deficiency conditions in obstetric and gynecological practice // Breast Cancer. 2011; 20: 1228–1231.
- Dolgov V.V., Lugovskaya S.A., Morozova V.T., Pochtar M.E. Laboratory diagnosis of anemia. M., 2001. P. 84.
- Kozlovskaya L.V. Hypochromic anemia: differential diagnosis and treatment // New Med. magazine 1996; 56:8–12.
- Shekhtman M. M. Guide to extragenital pathology in pregnant women. M., 2005, 816, 373–399.
- Johnson-Wimbley TD, Graham DY Diagnosis and management of iron deficiency anemia in the 21st century // Therap. Adv. Gastroenterol. 2011; 4 (3): 177–184.
- UNICEF/UNU/WHO. Iron Deficiency Anemia: Assessment, Prevention, and Control. A Guide for Program Managers. Geneva: WHO/NHD, 2001.
- Arkadyeva G.V. Diagnosis and treatment of iron deficiency conditions. Educational and methodological manual. M.: 1999: 22–25.
- Burlev V. A., Gasparov A. S. et al. Epocrine in the treatment of iron deficiency anemia in patients with uterine fibroids after hysterectomy // Problems of reproduction. 2003; 6:59–64.
- Kasabulatov N.M. Iron deficiency anemia in pregnant women // Breast cancer. 2003; 11, 1: 18–20.
- Lebedev V. A., Pashkov V. M. Principles of treatment of iron deficiency anemia in gynecological patients // Difficult patient. 2013, 11, 11: 3–7.
- Dvoretsky L.I., Zaspa E.A. Iron deficiency anemia in the practice of an obstetrician-gynecologist // Breastfeeding. 2008; 29.
- Kazyukova T.V., Samsygina G.A., Kalashnikova G.V. et al. New possibilities of ferrotherapy for iron deficiency anemia // Klin. pharmacology and therapy. 2000; No. 9 (2): 88–91.
- Pasricha SR, Flecknoe-Brown SC, Allen KJ et al. Diagnosis and management of iron deficiency anemia: a clinical update // Med. J. Aust. 2010; 193(9):525–532.
- Fernandez-Gaxiola AC, De-Regil LM Intermittent iron supplementation for reducing anemia and its associated impairments in menstruating women // Cochrane Database Syst. Rev. 2011. 12. CD009218.
- Burlev V.A., Konovodova E.N., Ordzhonikidze N.V., Serov V.N., Elohina T.B., Ilyasova N.A. Treatment of latent iron deficiency and iron deficiency anemia in pregnant women // Russian Bulletin of Obstetrics- gynecologist. 2006. No. 1. P. 64–68.
- Vertkin A.L., Godulyan O.V., Gorodetsky V.V., Skotnikov A.S. Iron deficiency anemia and the choice of drug for its correction // Russian Medical Journal. 2010. No. 5.
- Gratsianskaya A.N. Iron deficiency anemia: Ferro-Folgamma // Breast cancer. 2013; No. 29.
- Arvas A., Gur E. Are ferric compounds useful in the treatment of iron deficiency anemia? // Turk J Pediatr. 2000. Vol. 42(4). R. 352–354.
- Teucher B., Olivares M., Cori H. Enhancers of iron absorption: ascorbic acid and other organic acids // Int J Vitam Nutr Res. 2004. Vol. 74(6). R. 403–419.
- Konovodova E. N., Burlev V. A. Ferro-Folgamma + Erythropoietin - new possibilities for the treatment of anemia in patients with uterine fibroids // Farmateka. 2004. No. 15 (92). pp. 70–73.
- Ferro-Folgamma. Therapy with iron, folic acid, vitamin B12 and ascorbic acid. Scientific review. Werwag Pharma. M., 2001.
- Ghinea MM Treatment of iron deficiency anemia with Ferro-Folgamma // Rom J Intern Med. 2004. Vol. 42(1). R. 225–230.
A. Z. Khashukoeva1, Doctor of Medical Sciences, Professor S. A. Khlynova, Candidate of Medical Sciences M. V. Burdenko, Candidate of Medical Sciences M. R. Narimanova O. V. Kozlova, Candidate of Medical Sciences, Associate Professor
GBOU VPO RNIMU im. N. I. Pirogova Ministry of Health of the Russian Federation, Moscow
1 Contact information
Abstract. The role of Ferrum in the human organism has been analyzed, mechanisms of its digestion from food, clinical presentations of hypoferric conditions and women's hypoferric anemia, as well as approaches to therapy and prophylaxis of hypoferric anemia with modern oral preparations.