Doctors Cost
Price list Doctors clinic
Anemia is a whole category of syndromes characterized by a decrease in hemoglobin concentration and the number of red blood cells. This condition is diagnosed only by the results of laboratory tests; it is impossible to determine the disease by eye. Symptoms of anemia in adults can vary greatly. Therefore, the direction of treatment depends on the general state of health, the causes of the disease, age and gender, and concomitant pathologies.
Anemia - what is it and how dangerous is it?
This disease is also called anemia. This is a clinical-hematological syndrome that can occur as a consequence of one or another pathology. Hemoglobin protein is synthesized in the bone marrow with the participation of iron and is a component of erythrocytes - red blood cells. It delivers oxygen to the tissues and also helps to utilize carbon dioxide, delivering it to the lungs.
Such an important function easily explains the dangerous consequences of anemia. Firstly, even in conditions of a lack of iron in the diet, the body will fight anemia with all its might: first there will not be enough iron in the tissues and organs, and only lastly in the blood. This means that anemia often accompanies serious bone marrow diseases, tumors, and severe hematological diseases. It is important to pay attention to anemia as early as possible for this reason.
Secondly, a decrease in hemoglobin levels can lead to the following consequences:
- weakening of protective forces and increased susceptibility to aggressive environmental factors;
- decreased physical endurance and tolerance to intellectual stress;
- high risks of developing heart disease;
- high risks of developing purulent-septic processes.
Pregnant women deserve special attention. Anemia during pregnancy can lead to a high probability of spontaneous abortion, fetal malnutrition and intrauterine growth retardation, the appearance of hypoxia, and discoordination of labor. Physiological blood loss during childbirth or during a cesarean section will not cause complications in a healthy woman, but in an expectant mother with anemia it can also cause serious consequences.
Iron metabolism
It is known that iron is an important trace element, which is used mainly as a component of heme in erythrocytes for oxygen transport, and is present in smaller quantities in muscles in the form of heme-myoglobin and in the liver in the form of ferritin [10]. Its sufficient level is necessary to maintain physiological homeostasis [11]. However, excess iron levels can lead to cell death through the formation of free radicals and lipid peroxidation of biological membranes, toxic damage to proteins and nucleic acids. It is important that both iron deficiency and overload can have catastrophic consequences for the body, therefore the content of this microelement is strictly regulated [7, 9, 12–14].
The body of a healthy person contains about 3–5 g of iron, most of which, 2100 mg, is found in blood cells and bone marrow. Approximately 2.5 g of this iron is present in hemoglobin for oxygen transport, and another 2 g is stored as ferritin, mainly in the bone marrow, liver and spleen [9]. In the bone marrow, iron is used to form hemoglobin, liver iron is the main reserve of the microelement, and reticuloendothelial cells of the spleen remove old red blood cells. Finally, relatively small amounts of iron (approximately 400 mg) are present in cellular proteins such as myoglobin and cytochromes, and approximately 3–4 mg is bound to transferrin in the circulation [10, 15]. Almost all metabolically active iron is bound to proteins, and free iron ions can be present in extremely low concentrations.
Under natural conditions, no more than 0.05% (<2.5 mg) of the total amount of iron is lost daily due to exfoliating epithelium of the skin and gastrointestinal tract (GIT), as a result of sweating [12, 13, 16, 17]. The processes of absorption, recycling and storage of iron reserves are regulated by a special hormone - hepcidin, which is produced by liver cells. Under physiological conditions, hepcidin production is controlled by a complex interaction of signals, primarily the level of iron in the blood and the degree of oxygenation of liver tissue. Under pathological conditions, its production is regulated by proinflammatory cytokines, of which interleukin-6 plays a major role [7, 12, 13, 18].
Iron deficiency is detected in people of all age and social groups, but more often in women of reproductive age, young children and the elderly [5, 6]. The main reasons for the development of iron deficiency include decreased food intake, decreased absorption and blood loss. In developed, resource-rich countries, adult diets are almost always adequate, and the most common cause of iron deficiency is blood loss [2, 6].
Symptoms of anemia
Symptoms of anemia and treatment options may vary in patients of different age groups, gender, and general health. The most characteristic signs are the following:
- pallor of the skin (from white to yellowish) and mucous membranes;
- hair loss (not patchy baldness, but uniform hair loss);
- brittle nails, changes in the structure of the nail plate, suddenly appearing white spots on the nails;
- change in taste sensations, burning sensation on the tongue;
- cracks in the corners of the mouth;
- menstrual cycle disorders in women;
- decreased physical activity, resistance to physical activity;
- muscle weakness;
- increased drowsiness;
- rapid mood changes, irritability;
- dizziness, periodic headaches, less often fainting;
- ringing in the ears, darkening or spots in the eyes;
- unusual gastronomic preferences, for example, the desire to taste paints, soil, chalk, etc.;
- pain behind the sternum, usually in the heart area.
In each specific case, not all of the listed symptoms may be observed. Sometimes anemia is discovered by chance, during the diagnosis of general health, when the patient came to the doctor for another reason. Thus, frequent respiratory diseases are a common consequence of anemia, and consulting a doctor allows you to identify the true causes of constant ailments.
Differences between anemia in adults and children
According to WHO, about 2 billion people in the world suffer from anemia. The majority are children of different ages. Almost half of them are preschoolers, and a little more than a quarter are young school-age patients. And in adults, the disease occurs quite often. This syndrome is dangerous for both children and adults, and in adults the treatment period is somewhat longer.
Anemia in children may be associated with a specific cause: periods of rapid growth. The mechanisms of hematopoiesis are still imperfect, and the growth spurt requires an increased amount of nutrients. This may be associated with a temporary decrease in hemoglobin levels in the blood. However, this is still not a variant of the norm, but a syndrome that deserves close attention from a doctor. Anemia can lead to decreased defenses, poor weight gain, loss of appetite, weakness, and tearfulness. Timely methods of diagnosing and treating anemia will allow you to correct the condition and prevent complications.
The most dangerous complication of iron deficiency anemia (IDA) in adults is hypoxic coma. With high blood loss, it can cause death. Therefore, it is important to consult a doctor in time.
Complications of IDA
Complications arise with prolonged anemia without treatment and reduce the patient’s quality of life: decreased immunity, increased heart rate, which leads to heart failure; in pregnant women, the risk of premature birth and fetal growth retardation increases; in children, iron deficiency causes retarded growth and development; a rare and severe complication is hypoxic coma; hypoxia due to iron deficiency complicates the course of existing cardiopulmonary diseases (coronary artery disease, bronchial asthma, chronic cerebral ischemia, etc.) until the development of emergency conditions, such as acute or repeated myocardial infarction and acute cerebrovascular accident (stroke).
Why does anemia occur?
Anemia can be caused by many factors. There is often a combination of causes that quickly lead to blood disorders. The most common factors for the development of anemia:
- diet features. This is the most insidious reason. The lack of food rich in iron and B vitamins may not be taken seriously by a person. This is observed with a meager diet in women trying to lose extra pounds, the need to follow a certain table for gastrointestinal diseases, etc.;
- dysfunction of the digestive system. Even a complete diet does not guarantee the absence of anemia if iron cannot be absorbed in full due to gastrointestinal diseases. Iron absorption occurs in the stomach and upper small intestine. Diseases of these organs can lead to disruption of the process and the development of IDA;
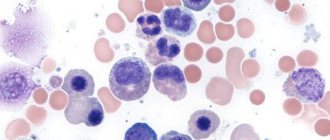
- diseases leading to disruption of red blood cell production in the bone marrow. Such diseases include pathologies of the kidneys and endocrine system, protein depletion, chronic infections, cancerous tumors;
- hemolysis. This is a condition in which red blood cells are destroyed prematurely. Normally, physiological hemolysis occurs no earlier than after 120 days—that’s how long the red blood cell “lives.” In pathological conditions, the lifespan of red blood cells decreases, causing anemia. This may be due to long-term drug therapy, infectious diseases, rheumatism, systemic diseases (scleroderma, etc.), kidney diseases, etc.;
- chronic blood loss. Blood loss is a common cause of anemia. These include heavy menstruation in women or a short (21 days or less) menstrual cycle, frequent nosebleeds or bleeding gums, gastrointestinal bleeding, non-healing wounds in people with diabetes, previous surgeries, childbirth, etc.
Anemia is always the result of an underlying disorder, so it is important to get accurate information about the causes. It is not recommended to engage in self-diagnosis and self-medication. Taking iron supplements can correct the condition, but will not get rid of the underlying disease, so it will not be fully effective and there is a high probability of relapse.
The approach to treating anemia depends on what causes the disease. Thus, secondary causes of the development of the syndrome include:
- refusal of protein foods, fasting due to life circumstances or beliefs. If a person is forced or prefers to give up food of animal origin and does not find a replacement for it in terms of iron content, deficiency and associated anemia develop;
- pregnancy. Hormonal changes, an increased need for vitamins and microelements can cause deficiency, including iron; anemia in pregnant women develops quite often. It is important to regularly visit an obstetrician-gynecologist and get tested on time so as not to miss possible violations;
- blood donation. Although blood donation is carried out taking into account safe blood loss, the risks of developing anemia increase. You should consult your doctor if you are acting as a donor;
- professional sports or increased physical activity. This is due to the fact that muscles require increased amounts of iron. The peculiarity of this cause is that anemia occurs in an erased form, because usually an athlete leads an active and healthy lifestyle. It is important to pay attention to fatigue, intolerance to previously habitual stress, and shortness of breath.
Classification of anemia
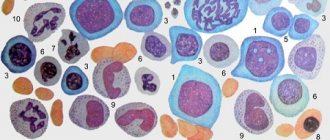
Anemia is classified according to the color index, which shows the level of saturation of the red blood cell with hemoglobin. The following types of syndrome are distinguished:
- hypochromic (iron deficiency, thalassemia, anemia associated with a lack of vitamin B6, etc.);
- normochromic (hemolytic, posthemorrhagic, i.e. resulting from blood loss/surgery, aplastic, etc.);
- hyperchromic (vitamin B12 deficiency, folate deficiency, etc.).
We see that anemia is not always synonymous with iron deficiency. Deficiency of B vitamins can also cause the development of the syndrome, and quite often it is associated with diet or absorption of nutrients in the intestines. And in this regard, independent diagnosis is impossible: only a doctor can determine the type of anemia, identify the causes and correctly correct the condition.
Treatment also depends on the severity of the anemia. It is determined by the severity of the decrease in hemoglobin levels. There are three degrees of severity:
- light. Hemoglobin level from 90 g/l;
- average. Hemoglobin level 70–90 g/l;
- heavy. Hemoglobin level is less than 70 g/l.
Features and diagnostic methods
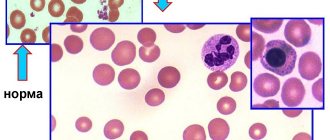
Diagnosis of anemia includes not only determining the fact of a decrease in hemoglobin levels. The doctor must understand the causes, assess the general state of health, and exclude severe pathologies that occur in a latent form, if they were not detected earlier. For this purpose, laboratory tests may be involved: a detailed clinical blood test is required. It will help assess the size, structural and other characteristics of blood cells.
The content of hemoglobin, erythrocytes, platelets, leukocytes, and several calculated erythrocyte indices are assessed. These indicators allow you to obtain data on the size, hemoglobin saturation, and uniformity of red blood cells. Determination of reticulocytes (young red blood cells) helps to understand the nature of anemia, as well as assess the reactivity of the hematopoietic system to the pathological condition. This is also important for monitoring treatment - the doctor can evaluate the response to the course of therapy.
Determination of erythrocyte parameters includes assessment of the following indicators:
- red blood cell count;
- hemoglobin concentration;
- average erythrocyte volume;
- hematocrit;
- width of distribution of red blood cells by volume;
- normoblasts.
The average volume and diameter of red blood cells are also assessed. An increase in these parameters may indicate a vitamin B12 deficiency. A decrease indicates a lack of iron.
Reticulocytosis or quantitative indicators of immature red blood cells may indicate certain features of bone marrow activity. In aplastic anemia associated with bone marrow suppression, the indicator may drop to zero. Reticulocytosis increases with blood loss and hemolytic anemia.
The doctor will also pay attention to those blood parameters that are not directly related to red blood cells. For example, an increase in platelet levels may be a consequence of IDA due to chronic blood loss. If leukocytes and platelets are reduced, we can talk about aplastic anemia. Detection of blast cells requires special attention; there is a high probability of acute leukemia.
Although laboratory diagnosis is critical, it is important to resort to other research methods. An examination is mandatory - the doctor evaluates the color of the skin and mucous membranes. Palpation helps to suspect possible disorders of internal organs and tumors. A thorough survey allows you to identify lifestyle features, probable causes, and the duration of symptoms.
If you have symptoms of anemia, it is important to consult a general practitioner or hematologist. He will order the necessary tests and make suggestions as to the reasons. To clarify them, it is sometimes necessary to resort to additional diagnostic tools:
- fibrogastroduodenoscopy. Assessing the condition of the mucous membranes of the esophagus and stomach will help in identifying gastric bleeding;
- Ultrasound of the liver and kidneys;
- examination of the pelvic organs in women;
- CT or MRI if indicated;
- colonoscopy;
- X-ray of the lungs, etc.
A complete list of diagnostic methods is not required: a specialist will find out the possible causes and refer you to certain studies according to indications. If necessary, he can refer you to another doctor. So, if the cause of anemia is heavy and prolonged menstruation or a short cycle, an examination by a gynecologist will be required. Detection of gum problems (bleeding) and symptoms of periodontal disease will require a visit to a periodontist. Frequent nosebleeds are a reason to consult an otolaryngologist, assess blood pressure parameters, etc.
Treatment of anemia
Clinical recommendations for the treatment of anemia depend on many factors: gender, age and condition of the patient, type and severity of the syndrome. There are several general principles that apply in medical practice. These include the following:
- Mandatory diet correction for B12 deficiency and iron deficiency anemia. This complements the main course of treatment - taking medications that will compensate for the lack of substances;
- timely correction of deficiency of vitamins and microelements in pregnant women;
- mandatory consultation with a specialist when identifying specific causes: chronic bleeding, features of the functioning of the reproductive system in women, etc.;
- examination by a specialist in cases where anemia has caused complications in organs and systems. For example, consultation with a cardiologist for angina pectoris, low blood pressure, etc.
An integrated approach allows you to cope with the cause of the syndrome, rather than mask the symptom, and also eliminate or correct the consequences of the disease.
Cost of consultation for anemia?
| Name of service | Price, rub.) |
| Initial appointment with a cardiologist | 2000 rub. |
| Repeated appointment with a cardiologist | 1500 rub. |
| Primary appointment with a general practitioner | 2000 rub. |
| Repeated appointment with a general practitioner | 1500 rub. |
| Prescription of treatment (drawing up an individual treatment regimen) | 1500 - 3000 rub. |
All our services and prices
The main objectives of the treatment of anemia:
- eliminating the cause. Identification and elimination of the source of chronic blood loss, normalization of iron absorption in the intestines, reduction of blood loss during menstruation, etc.;
- replenishing the lack of important substances;
- prevention of the development of dystrophic changes in internal organs, restoration of their normal function.
It is important to remember that it is impossible to eliminate anemia with diet alone. This is explained by the fact that the absorption of iron from food is no more than 2.5 mg/day. From drugs, it is absorbed 20 times more. However, following a diet is very important as an addition to a course of drug therapy. Patients are recommended foods containing large amounts of digestible protein and iron.
Meat contains heme iron, which is absorbed by 30%. Also, liver, eggs and fish contain iron, which is absorbed by 10–15%. The microelement is also found in products of plant origin; absorption of Fe from legumes, spinach, soybeans, dill, and bread is up to 3–5%. It is advisable to include apples, pomegranates and pomegranate juice, beets, and buckwheat in your diet. But in terms of their overall benefits, the absorption of iron ions from them is limited, as demonstrated by numerous studies. That is why it is important to understand that eating apples will not help cure anemia; this is nothing more than a myth.
People who eat meat get more iron than those who are vegetarian. Strict vegetarianism can cause anemia because vegetables and grains contain substances that interfere with the absorption of iron. If you follow a normal, balanced diet, they do not entail serious consequences.
It is important to understand that a balanced diet helps cover the daily requirement, but will not eliminate iron deficiency. The basis of correction is drug therapy.
Blood transfusions (transfusions) are performed according to vital indications. They are usually carried out when hemoglobin drops below 50−40 g/l.
If the situation is not so severe, the doctor prescribes medication. IDA is corrected with oral medications; the course of treatment in adults is quite long. Interim monitoring is mandatory - detailed blood tests are performed. The principles of treatment in this case are as follows:
- prescribing iron supplements with a dose of divalent or trivalent iron sufficient for a person;
- supplementing the course of treatment with substances that enhance absorption. Succinic and ascorbic acid are used;
- refusal of antacids, oxalates and other drugs that reduce iron absorption whenever possible or recommendations for taking them at different times;
- therapy for at least 6–8 weeks until normalization and for at least another 4 weeks after improvement.
Let’s take a closer look at the recommendations about avoiding medications and foods that interfere with the absorption of iron. This can be prevented by phosphoric acid, calcium, tannin, phytin, and salts. Therefore, you should not drink tea, coffee, or Coca-Cola at the same time as taking iron.
For women suffering from long and heavy menstruation, not associated with diseases of the endocrine and reproductive systems, it is important to maintain monthly short courses of treatment: take average therapeutic doses of Fe for 3-5 days.
Clinical guidelines for the treatment of anemia dictate regular monitoring. The criterion for the effectiveness of therapy is an increase in reticulocytes at least three times 7-10 days after the start of treatment.
All iron preparations are classified into two groups: ionic (salt or polysaccharide compounds of ferrous iron) and non-ionic, consisting of a ferric iron complex.
Ferrous sulfate is included in mono- and polycomponent products and is well absorbed, and also has a relatively smaller list of side effects. Chloride compounds are absorbed less well and can also cause undesirable consequences: metallic taste in the mouth, dyspepsia, darkening of tooth enamel, etc. Modern treatment standards call for the use of ferrous or trivalent iron preparations.
Sometimes iron supplements are indicated to be administered parenterally. This is relevant for cases where there is a malabsorption in the intestine and other features. The main indications for drip infusion are the following:
- impaired intestinal absorption - malabsorption, previous surgery, etc.;
- intolerance to oral medications;
- the need for quick saturation. For example, in case of emergency surgery;
- treatment with erythropoietin: with it, the need for iron sharply increases, since it is actively consumed by red blood cells.
Important: parenteral administration requires no more than 100 mg/day. Otherwise, there is a risk of complications.
Treatment regimens for anemia associated with vitamin deficiency include additional intake of vitamin B12, folic acid and certain microelements.
Treatment of anemia associated with diseases of the hematopoietic organs and bone marrow tumors is developed individually and requires special attention to the cause.
Reasons for development
Thus, we can distinguish 4 main reasons for the development of IDA:
- insufficient intake of iron into the body from food;
- increasing the body's need for iron;
- violation of its absorption;
- disruption of iron transport throughout the body.
Insufficient intake of iron into the body
Food is the main source of iron for the human body. And an unbalanced diet is one of the most common causes of iron deficiency anemia in both children and adults.
In most cases this is due to:
- prolonged fasting;
- vegetarian or vegan diet;
- consumption of monotonous foods with insufficient amounts of heme and non-heme iron;
- anorexia.
For infants, especially during the first six months of life, the only source of iron is mother's milk. Provided that a nursing woman does not have IDA, the child receives it in the required amount. At the same time, transferring a baby to artificial feeding or early introduction of complementary foods often becomes the reason for the development of iron deficiency anemia.
Nan-O-Fer (Switzerland)
Nan-O-Fer (Switzerland) – capsules for oral use, created taking into account the peculiarities of iron absorption in the body. It is Nanofer that today is one of the priority drugs for the treatment of IDA, since it contains liposomal iron in the form of pyrophosphate, and in order to improve the quality of its absorption, vitamins B12, B6 and folic acid are added to the drug.
Eslotin
Check availability
If a nursing mother has a severe form of iron deficiency anemia, this can lead to congenital iron deficiency in the child. This can also occur in premature babies, as well as those born from multiple pregnancies. In such situations, they speak of congenital iron deficiency, and its symptoms appear from the first weeks of the child’s life.
Increasing the body's need for iron
An increased need for iron is usually characteristic of women during pregnancy and breastfeeding. This is due to:
- an increase in blood volume and the number of red blood cells, which requires about 500 mg of iron;
- the need to form the placenta (200 mg);
- ensuring proper development of fetal tissues and organs (300 mg);
- loss of blood during and after childbirth (50-150 mg);
- covering the newborn's needs for this macronutrient (400-500 mg).
During pregnancy and lactation, a woman’s need for iron almost doubles, and with multiple pregnancies it increases even more.
In general, during pregnancy and breastfeeding 1 child, the female body loses about 1 g of iron. Considering the fact that a maximum of 2.5 mg of iron can be absorbed per day, iron deficiency anemia in pregnant women is an almost inevitable condition. But it is within the power of a woman to ensure that it proceeds to the mildest extent through proper preparation for pregnancy, correction of the diet and the use of iron supplements if necessary.
Also, an increase in the body's need for iron occurs during blood loss, which is also most typical for women. Every month, during menstrual bleeding, the female body loses iron. But such losses are physiological and, with proper nutrition, do not lead to the development of IDA. Unfortunately, the lifestyle and diet of most women is not capable of creating sufficient amounts of iron reserves in the body and covering its monthly losses.
But besides menstrual bleeding, other situations accompanied by increased blood loss can lead to iron deficiency anemia in people of any gender and age. But single losses of even a large volume of blood, for example, during severe injuries or operations that violate the integrity of soft tissues, usually do not provoke IDA, since the iron reserves in the body are sufficient to replace them.
Iron deficiency anemia usually develops against the background of chronic and prolonged bleeding, typical of:
- peptic ulcer of the stomach and duodenum;
- hemorrhoids;
- intestinal diverticula;
- Crohn's disease;
- endometriosis;
- uterine fibroids;
- hematuric form of chronic glomerulonephritis;
- frequent nosebleeds;
- systemic vasculitis, systemic lupus erythematosus;
- intestinal polyposis;
- malignant tumors in the terminal stage.
IDA can also occur in donors who donate large volumes of blood more than 4 times a year.
Other reasons for the increased need for this macronutrient are:
- heavy physical labor, active sports;
- period of puberty and active growth;
- parasitic infestations.
Iron malabsorption
Iron absorption occurs through the mucous membrane of the duodenum and the initial parts of the small intestine. This is only possible if their mucous membrane is in normal condition. But there are many diseases that can lead to changes in it, and therefore to disturbances in the absorption of iron from food. These include:
- enteritis is a disease accompanied by inflammation of the intestinal mucosa;
- celiac disease is a hereditary pathology in which the body is not able to absorb gluten, which leads to impaired absorption of all nutrients in the intestines in its presence;
- atrophic and autoimmune gastritis – gastrointestinal pathologies in which destruction of cells of the gastric mucosa is observed;
- resection of the stomach and/or small intestine - surgical interventions performed in the presence of compelling indications, but capable of disrupting the production of hydrochloric acid, which is necessary for the transformation of ferrous iron into ferric iron;
- Crohn's disease is an autoimmune disease of the gastrointestinal tract, accompanied by inflammation of the mucous membranes of the intestines, and sometimes the stomach;
- Helicobacter pylori infection is the main cause of the development of gastritis and peptic ulcers of the stomach and duodenum with impaired formation of hydrochloric acid;
- cystic fibrosis is a hereditary pathology in which the functioning of most glands of the body is disrupted;
- oncological diseases of the stomach and duodenum.
Alcoholism also contributes to damage to the mucous membranes of the gastrointestinal tract, which leads to impaired iron absorption. In addition, alcohol inhibits the activity of red bone marrow, which can aggravate the course of iron deficiency anemia.
Also, the use of a number of medications can provoke disturbances in the absorption of iron in the intestines. This is typical for the use of antacids that reduce the acidity of gastric juice, iron-binding drugs, as well as NSAIDs that are often used by people without prescription and supervision by a doctor (Paracetamol, Ibuprofen, Nurofen, Nise, Diclofenac, Aspirin, etc.). The latter drugs have anti-inflammatory and analgesic properties, but at the same time they negatively affect the condition of the mucous membranes of the gastrointestinal tract and thin the blood.
In such situations, IDA will occur even if there is sufficient intake of heme and non-heme iron in food.
Transportation disruption
The main carrier of iron throughout the body is the protein transferrin. But in a number of situations there is a violation of its synthesis in the body. This is typical for:
- congenital disorders of transferrin production, in which case signs of iron deficiency anemia will be observed from the first months of the child’s life;
- liver pathologies, in particular cirrhosis and hepatitis;
- tuberculosis;
- severe infectious diseases.
Features of prevention
Prevention of anemia should be carried out in case of hidden signs of iron deficiency or the presence of risk factors for the development of the syndrome. Thus, if there are grounds for the rapid development of anemia, it is important to examine the level of hemoglobin and serum iron annually. The following patients are at risk:
- blood donors, especially females;
- pregnant women, especially those with frequent pregnancies;
- women with long (more than 5 days), heavy menstrual bleeding, short cycle (21–25 days);
- children from multiple pregnancies, premature babies;
- children during growth spurts;
- people with dietary restrictions;
- people suffering from chronic bleeding. For example, with hemorrhoids, etc.;
- patients taking non-steroidal anti-inflammatory drugs;
- professional athletes and people engaged in active physical labor.
Functions of iron in the body
The main studied processes occurring with the participation of iron include:
- blood cell formation;
- synthesis of hemoglobin and myoglobin;
- supplying body tissues with oxygen and evacuating carbon dioxide;
- synthesis of ATP (energy carrier molecules) from blood glucose;
- synthesis of cytochromes (P450) and enzymes (catalases) - natural antioxidants involved in the processing of drugs, xenobiotics and the removal of hydrogen peroxide;
- DNA synthesis;
- participation in the regeneration of cells and tissues;
- synthesis of hormones and neurotransmitters;
- regulation of thyroid function;
- regulation of immune system function;
- participation in the processes of physical and psychomotor development.