Anemia can cause a huge number of problems, from fatigue and hair loss to heart failure and even cancer in the long term. According to WHO estimates, more than one and a half billion people worldwide suffer from various types of anemia, which is a quarter of the entire world population. Moreover, pathologies often occur in preschool children - 50%, and least often in men - 12%.
In most cases, people do not even pay attention to the main signs of anemia (constant fatigue, dry skin, pallor), considering them an insufficient reason to see a doctor. Of course, such symptoms do not always indicate a disease; it cannot be diagnosed only by the presence of these symptoms. Moreover, you should not start taking iron-containing medications on your own - this can lead to serious complications. At the same time, for a full diagnosis of anemia, it is not enough to simply donate blood for hemoglobin. For example, in people who smoke, the level of hemoglobin and red blood cells is usually normal: carbon monoxide, which is contained in cigarettes, when combined with hemoglobin, forms a substance called carboxyhemoglobin, which is not capable of carrying oxygen. Therefore, to compensate for oxygen starvation, the hemoglobin level increases. It turns out that a comprehensive study is needed, reflecting the true state of the hematopoietic system and the health of the body as a whole. In addition, it is important to know what exactly causes anemia. In older people, for example, it often occurs against the background of a tumor process in the gastrointestinal tract. There is a type of anemia associated with poor absorption of vitamin B12, and to identify it, the level of vitamin B12 in the blood serum should be determined and the morphology of red blood cells should be assessed. To assess the state of the hematopoietic system and diagnose the true causes of anemia, DILA laboratory diagnostic experts have developed a comprehensive screening program 175 “Determine the cause of anemia.” It will allow you to exclude or confirm the presence and nature of anemia, establish its causes and severity.
Who is the examination recommended for?
- for preventive purposes: people with increased physical activity and athletes, children during periods of active growth and puberty, blood donors, people following a vegetarian diet, children and adults with diagnosed parasitic diseases;
- women at the planning stage and during pregnancy;
- for men, women and children in the presence of complaints that are accompanied by characteristic signs of anemia, after severe blood loss, with previously diagnosed anemia to monitor treatment;
- children with congenital iron deficiency.
The program can be used for the primary diagnosis of anemia and differential diagnosis of anemia, examination of patients with high risks of developing the disease and assessment of the effectiveness of treatment.
About the disease
What is this? Anemia (anemia) is a decrease in hemoglobin content and/or a decrease in the number of red blood cells per unit volume of blood, leading to a decrease in the supply of oxygen to tissues.
What caused it? The causes of anemia are varied and may be closely related to the following factors:
- Somatic diseases - liver and kidney diseases, autoimmune, infectious and inflammatory processes.
- Acute and chronic blood loss. Acute is considered blood loss with a blood volume of more than 500-700 ml (in adults), which occurs within a short period of time. It can be visible (bleeding from a wound, bloody vomiting, uterine and nasal bleeding) and initially hidden (bleeding into the intestines, into the abdominal cavity and/or pleura, extensive hematomas). Chronic blood loss develops against the background of minor but prolonged blood loss (heavy and prolonged menstruation, stomach ulcers, cancer, hemorrhoids, hemodialysis procedures). Over time, even minor losses deplete the body's iron stores when the amount of iron the body loses exceeds its intake from food. As a result of iron deficiency, hemoglobin synthesis is impaired
- Poor nutrition, lack of vitamins and microelements. Anemia develops against a background of deficiency of iron, vitamin B12 and folic acid. This may be due to both a lack of substances necessary for the body in the diet (for example, with strict diets or vegetarians), and with a decrease in iron absorption as a result of various diseases of the duodenum and the initial parts of the small intestine (enteritis, tumors, conditions after operations on the small intestine). intestines). In conditions that cause a decrease in the level of blood proteins that carry iron (nephrotic syndrome, impaired protein-synthetic function of the liver, malabsorption syndrome, nutritional deficiency), a decrease in the amount of iron and, as a consequence, anemia may also be observed.
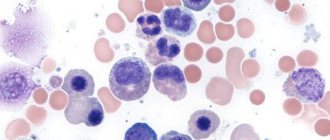
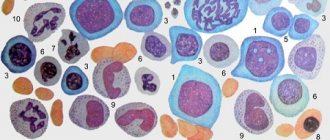
- Hematopoietic disorder. Anemia occurs when there is insufficient formation of red blood cells in the bone marrow (for example, when the bone marrow is depleted or damaged by toxic substances, ionizing radiation), against the background of premature and excessive destruction of red blood cells in the bloodstream (for example, during hemolysis). Anemia can also occur with the formation of secondary foci (metastases) of tumor cells in the bone marrow, disruption of the production of the non-protein part of hemoglobin (heme) and the accumulation of its toxic products, as well as disruption of the regulation of red blood cell synthesis (decreased production of the hormone that stimulates the growth and reproduction of red blood cells - erythropoietin ).
Depending on the causes, anemia is classified as iron deficiency, caused by blood loss or insufficient iron intake or absorption; B12 deficiency and folate deficiency, caused by insufficient intake or absorption of cyanocobalamin and folic acid, respectively; aplastic, caused by a violation of the formation of red blood cells in the bone marrow; and hemolytic, in which the red blood cells in the body are destroyed too quickly. The most common form of anemia is iron deficiency - it is diagnosed in 80-90% of patients who have a reduced number of red blood cells and/or hemoglobin in the blood. Iron deficiency conditions develop gradually. Initially, a negative iron balance is created, in which the body's needs for it and its losses exceed the amount it receives from food. This may be due to blood loss, pregnancy, breastfeeding, growth spurts during puberty, impaired absorption of micronutrients in the gastrointestinal tract, or insufficient consumption of foods containing iron, as with vegetarianism.
Normally, iron is absorbed in the small intestine, but in some chronic gastrointestinal diseases, malabsorption syndrome occurs - impaired absorption of vitamins, microelements and other beneficial substances from food. In the blood, iron is transported by the protein transferrin to places where it is consumed or accumulated. In iron deficiency conditions, the amount of free transferrin in the blood increases, and the level of serum iron decreases. The production of hemoglobin in the bone marrow is not so active, as a result of which iron deficiency anemia develops with all the clinical manifestations of anemia.
Main causes of iron deficiency
In a number of cases, there are signs of iron deficiency in the body, ultimately leading to anemia. The most common causes of low iron levels include the following:
- reduced dietary intake;
- pathology of element absorption in the intestine;
- presence of chronic blood loss;
- increased iron requirements during pregnancy;
- excess polyphenols in food (for example, when drinking green tea or coffee);
- large blood losses due to injuries.
The group at increased risk of developing iron deficiency includes premature babies and children whose diet is deficient in iron, teenage girls, and those at the beginning of menstruation. A special category of people with anemia includes pregnant women, whose need for iron increases many times over. Blood donors may also notice signs of iron deficiency.
Low iron levels are common among vegetarians due to inadequate dietary intake of the element. In people with diseases of the digestive system, as well as with the development of chronic infectious diseases, anemia develops due to impaired absorption of iron by the digestive system.
It should be borne in mind that anemia is not always a harmless and easily corrected condition. Quite serious chronic diseases are often hidden under the mask of a lack of iron in the blood . Anemia is often one of the symptoms of cardiovascular diseases, chronic diseases of the urinary system, a manifestation of malabsorption syndrome (or impaired intestinal absorption function). Anemia in women can occur with heavy menstrual bleeding. Other dangerous pathologies accompanied by iron deficiency in the blood are cancer and chronic inflammatory processes in the intestines.
Symptoms and complications
The severity of anemia depends on the severity of the disease and the speed of its development. The lower the hemoglobin level and the faster the anemia develops, the more pronounced the clinical picture.
There are general (nonspecific) signs of anemia and manifestations characteristic of a particular type of disease. Nonspecific signs include:
- pale skin;
- weakness and increased fatigue;
- drowsiness;
- frequent dizziness and fainting;
- noise in ears;
- “flies” before the eyes;
- shortness of breath and rapid heartbeat, rapid pulse.
The absence of these symptoms does not exclude the presence of anemia, since with mild and moderate forms of the disease, as well as its slow development, the clinical picture may be blurred.
With iron deficiency anemia, dryness and disruption of the integrity of the skin, brittle nails and hair, the appearance of ulcerations and cracks in the corners of the mouth, and muscle weakness are observed. There may be a burning sensation of the tongue, a distortion of taste in the form of an indomitable desire to eat chalk, toothpaste, earth, raw cereals, raw meat, as well as an addiction to certain odors (acetone, gasoline). In addition, with iron deficiency, damage to the gastrointestinal tract is often observed.
A lack of vitamin B12 can also be manifested by problems with the gastrointestinal tract (in particular atrophic gastritis) and neurological symptoms - these include paresthesia, sensory disturbances, and numbness of the extremities. Extremely severe anemia is sometimes accompanied by mental disorders and hallucinations.
Clinical manifestations of folic acid deficiency are very similar to those of vitamin B12 deficiency, but there are no neurological symptoms and inflammation of the tongue is rarely observed.
Hemolytic anemia is characterized by yellowness of the skin and mucous membranes, an increase in the size of the spleen, and a tendency to form stones in the bile ducts. With massive hemolysis of red blood cells (hemolytic crisis), in addition to jaundice, anemia and deterioration of the general condition, nausea, vomiting, disturbances of consciousness, convulsions are possible, and acute renal and/or cardiovascular failure may develop.
Aplastic anemia , which occurs against the background of suppressed proliferation of bone marrow cells, is characterized by bleeding (nasal, gastrointestinal tract) and hemorrhages (mainly in the legs, thighs and abdomen, and hematomas are formed at injection sites). Bronchitis and pneumonia are often diagnosed.
Like symptoms, complications of anemia can be general and specific. Common ones include:
- decreased blood pressure;
- deterioration of immunity and increased incidence of infectious diseases;
- during pregnancy – chronic fetal hypoxia, intrauterine growth retardation;
- decreased intellectual and physical development in children.
Specific complications develop with a certain type of anemia. For example, hemolytic anemia is accompanied by an increased risk of developing cholelithiasis, hemosiderosis of internal organs (excessive deposition of hemosiderin, a pigment that is formed during the enzymatic breakdown of hemoglobin), hemolytic crises, and an increase in the size of the liver and spleen.
Acute massive blood loss can lead to the development of multiple organ failure (cardiovascular, renal, respiratory), DIC syndrome (hemostasis disorder).
With vitamin B12 deficiency, complications often affect the spinal cord.
With anemia associated with impaired production or utilization of porphyrins (impaired hematopoiesis), diabetes mellitus, adrenal insufficiency, liver cirrhosis, and circulatory problems may develop.
Symptoms of iron deficiency
The classic clinical signs of iron deficiency are:
The patient complains of fatigue and fatigue even from the usual load. The main reason is the insufficient supply of oxygen to the cells and tissues of the body. Weakness and lack of endurance are also due to the fact that iron is involved in the production of energy in the form of ATP molecules. In the absence of sufficient oxygen, muscle tissue switches to anaerobic mechanisms for producing ATP, which is less efficient and more taxing on the body. Other common symptoms of anemia include mood swings and irritability . The mechanism of this process is as follows: a lack of iron in the body disrupts the production of the neurotransmitter dopamine and thyroid hormones, which leads to hypothyroidism. Hence the feeling of anxiety, stress, irritability and mood swings.- The next symptom of iron deficiency is decreased concentration . As you know, oxygen is one of the factors that ensures the activity and high performance of the brain. Its deficiency in anemia is the cause of impairment of the subtle cognitive functions of the brain. Many patients with low iron levels in the body experience attacks of dizziness. Frequent dizziness is also the result of a lack of oxygen in red blood cells. The same series of symptoms of anemia include unexplained frequent headaches. Lack of iron leads not only to a decrease in hemoglobin content, but also disrupts the formation of another iron-containing protein - myoglobin. This leads to soreness and tension in the muscles of the face, neck and shoulders, which explains frequent headaches in iron deficiency.
A number of patients with anemia complain of sleep disturbances . Ferritin, the main protein that stores iron, is one of the most important regulators of sleep. Insomnia in iron deficiency occurs when iron reserves are depleted at the earliest stages of the pathological process, since ferritin is the first to disappear.- Visible changes in anemia in men and women occur in the skin and nails : the surface of the lips looks dry and cracked, the nails become brittle and longitudinally striated. Ferritin is an essential component necessary for the normal processes of tissue regeneration and renewal, especially the skin and its appendages (hair, nails). Depletion of ferritin stores leads to deterioration of cellular repair processes in these tissues. The skin and mucous membranes of patients with anemia are usually pale, this is especially noticeable when hemoglobin drops below 90 g/l. First of all, those areas where the blood flow is closest to the surface of the skin or mucous membrane turn pale: lips, conjunctiva, palms, nail beds.
- , restless legs syndrome or Willis-Ekbom disease may occur A deficiency of the element in the body leads to an imbalance between the synthesis of dopamine and the metabolism of thyroid hormones. To make such a diagnosis, the presence of 4 main signs is necessary: the need to move the legs to overcome unpleasant sensations in the limbs;
- unpleasant sensations in the legs arise and intensify at rest;
- unpleasant sensations partially or completely disappear in an active state (running, walking);
- the need to move the legs and discomfort intensify in the evening and often cause insomnia.
Diagnosis of anemia
When the first signs of the disease appear, it is important to consult a doctor to make an accurate diagnosis. An important role in identifying the causes of anemia is played by information obtained during a patient interview - age, the presence of occupational factors, the nature of the diet, the presence of concomitant diseases, and medication use. No less important are the examination data - the color and condition of the skin, the size of the lymph nodes, liver and spleen, signs of damage to the nervous system.
The first stage of diagnosing anemia usually includes the following studies:
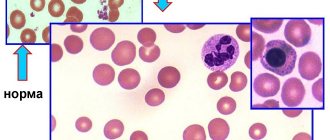
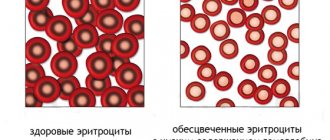
- General detailed blood test. In anemia, it shows small pale colored red blood cells, decreased MHC (mean hemoglobin content in a red blood cell), MCV (mean red blood cell volume), MCHC (mean hemoglobin concentration in a red blood cell), decreased hemoglobin concentration and hematocrit. A complete blood count allows your doctor to evaluate the size, shape, and maturity of your blood cells.
- Ferritin. This biomarker is the most specific and sensitive parameter of the presence of iron reserves in the body, the main participant in iron metabolism and the donor of iron for cells that are deficient in it. Ferritin concentrations increase in iron deficiency anemia, but may increase in liver disease and inflammation.
- Folic acid (vitamin B9). It promotes the combination of globin and heme in hemoglobin and myoglobin and is an indicator for the differential diagnosis of anemia, in particular for identifying or excluding folate deficiency anemia.
- Iron is a key marker for diagnosing iron deficiency anemia. When there is a shortage of iron in the body, serum iron is consumed very quickly; when there is an excess, transferrin is completely saturated with iron. The main form of long-term storage of this element is its complex with the protein ferritin. Iron concentration increases with hemolytic, pernicious and aplastic anemia, and decreases with iron deficiency.
- Vitamin B12 (cyanocobalamin). Its deficiency can lead to the development of macrocytic (megaloblastic) anemia.
The screening program 175 “Determine the cause of anemia” includes a complete blood count and all the specified markers. A comprehensive determination of all these indicators allows the doctor to identify the exact cause of anemia and differentiate it from other dangerous diseases.
Laboratory tests for the primary and differential diagnosis of anemia are important and can be recommended both to establish the cause of nonspecific symptoms and as a screening test, especially in groups at high risk of developing anemia. The risk group includes pregnant and lactating women, children, people with chronic diseases and diseases of the gastrointestinal tract, vegetarians, and people experiencing chronic stress.
Diagnosis of iron deficiency
Currently, several laboratory tests have been developed to diagnose iron deficiency. The main ones include determining the following blood parameters:
- the amount of serum iron;
- indicator of total iron-binding capacity of serum (TIBC);
- transferrin iron saturation percentage;
- ferritin amount;
- amount of hemoglobin.
It is important to understand that it is a big mistake to prescribe iron supplements solely based on the results of determining low ferritin. In the presence of a MTHFR mutation that disrupts the processing and absorption of iron, folic acid, and vitamin B12, ferritin is always low and serum iron is high, which does not allow prescribing iron supplements to such patients.
The goals of laboratory tests for iron deficiency anemia are:
- identification of disturbances in iron metabolism;
- determination of the nature of anemia;
- assessing the risk of developing iron overload in the body.
Preparation for laboratory tests for anemia is simple and fairly standard. It is necessary to donate blood in the morning, strictly on an empty stomach (with an 8-hour break after eating). The day before testing, you must stop taking iron supplements and/or multivitamins. If radioisotope diagnostics were carried out the day before, the study of iron metabolism should begin no earlier than 4-5 days after its completion. It is also important to consider that some medications may interfere with test results. For example, estrogen or oral contraceptives can increase TBI, while corticosteroids and testosterone, on the contrary, lower TBI.
The place of iron supplements in the correction of anemia in a cardiac patient
In cases of detection of true “comorbid” IDA, not associated with existing cardiac pathology (tumors of the stomach and intestines, bleeding hemorrhoids, menorrhagia in women, malabsorption syndrome, gastroesophageal reflux disease, nutritional deficiency, etc.), treatment should be aimed at eliminating this cause (if possible) or correction of existing disorders (erosive-ulcerative and tumor lesions of the gastrointestinal tract, uterine fibroids, enteritis, etc.). When a correctable cause of IDA is identified, treatment (medical, surgical) of the underlying disease and pathogenetic therapy with iron supplements are necessary. In the presence of an irremovable or difficult to eliminate cause (pregnancy, nosebleeds due to hereditary hemorrhagic telangiectasia, menorrhagia, etc.), pathogenetic therapy of the pancreas remains the only way to correct Fe deficiency.
2.1. Pancreas with anemia in patients with coronary artery disease
In one of the studies devoted to the problem of the combination of coronary heart disease with anemia, it was shown that in patients with coronary heart disease in combination with mild anemia (Hb - 130–110 g/l) and latent Fe deficiency when correcting Hb, serum Fe, and total iron-binding capacity serum during the use of the drug Sorbifer Durules (iron sulfate + ASA), the frequency, duration and intensity of angina attacks decreased, the need for nitroglycerin decreased, exercise tolerance increased, the severity of comorbid clinical manifestations decreased: edema, shortness of breath, palpitations, heart rate [15].
2.2. Pancreas with anemia in patients with CHF
Treatment of pancreatic anemia in CHF is of great interest among researchers, since it is relatively inexpensive and there is evidence of its effectiveness, although many unresolved issues remain [58]. Noteworthy are the results of a study demonstrating the effectiveness of intravenous administration of pancreas to 16 patients with CHF without concomitant EPO therapy, against the background of which a significant increase in the average Hb level was achieved from 112 to 126 g/l, improvement in exercise tolerance according to the 6-minute walk test and quality life in general [59]. In another study, during treatment with iron salts (Ferro-Folgamma) and iron-containing complexes (Venofer), a decrease in the severity of clinical signs of heart failure and a transition of patients to a more favorable FC were noted [60].
Three randomized placebo-controlled studies were carried out on the use of pancreatic acid in patients with CHF and anemia. In one of them, 40 patients were randomized to receive intravenous pancreatitis or placebo [61]. After 6 months, Hb values during the use of pancreatic acid increased on average from 103 to 118 g/l and remained stable in the placebo group. Along with this, during treatment of the pancreas, positive dynamics in the concentration of natriuretic peptide, C-reactive protein, LVEF and 6-minute walk test were noted. Another study included 35 patients with CHF who received intravenous prostate cancer or placebo for 16 weeks [62]. There was a decrease in heart failure FC according to NYHA, an improvement in the general condition of patients, according to their self-assessment, without improvement in exercise tolerance, according to the treadmill test. Another larger randomized placebo-controlled study of the effectiveness of pancreas among patients with CHF included 429 patients with CHF with anemia [63]. It was shown that against the background of intravenous administration of the iron-polymaltose complex, along with an increase in Hb concentration, a significant or moderate improvement in the condition was noted, according to patient self-assessment (50 and 28%), a decrease in the FC of CHF according to NYHA (47 and 30%), and an improvement in test scores 6- minute walk and quality of life compared with patients receiving placebo. Since not all patients had improvement accompanied by an increase in Hb levels, it was suggested that the effect of RV in patients with CHF is not only associated with an increase in Hb levels, but may also be due to an improvement in the function and performance of muscles, including the heart. This assumption is supported by the results of experimental studies, which showed that muscle performance improved in rats receiving pancreatic acid [64, 65].
In the study by I.R. Kim et al. while taking oral pancreatic acid in combination with standard therapy for patients with a combination of CHF and IDA, positive dynamics were also noted in the form of not only an increase in Hb concentration from 97.1 ± 3.7 to 106.7 ± 3.9 g/l, but also increasing exercise tolerance (distance traveled in 6 minutes increased from 284.8 ± 26.1 to 420.3 ± 31.4 meters) and improving the clinical status of patients. Changes in central hemodynamics were also noted in the form of an increase in EF from 37.1 ± 3.6 to 49.04 ± 4.2%, p < 0.05, and stroke volume from 43.7 ± 5.6 to 66.3 ± 6.2 ml [66].
In our study, against the background of treatment for the correction of anemia (RV, vitamin B12) in patients with CHF with severe anemia (Hb less than 70 g/l), in contrast to patients with initially less severe anemia, an improvement in exercise tolerance and a reduction in the proportion of patients with high FC of CHF according to NYHA, despite a decrease in initial indicators of EF, stroke, and end-systolic volumes [43].
Regarding the problem of managing patients with CHF with anemia, in particular the tactics of using pancreatic glands, a number of questions remain [67], which boil down to the following: • Is it always necessary to use parenteral pancreatic glands or do pancreatic glands for oral administration have the same effect? • Is there a difference in the response to pancreatic therapy in patients with IDA and ACD? • Does LV function improve after RV treatment? • Do pancreas have a multilateral, not only “hematological” effect on patients with severe CHF? • Is it necessary to use pancreas more widely for intravenous administration in patients with ACD? • How long can parenteral pancreatic fluids be used in patients with ACD, and are there concerns about Fe deposition in the liver or heart tissue with long-term administration of pancreatic acid? To answer these questions, further research in this direction is necessary.
2.3. Pancreas when using EPO in patients with CHF with anemia
There are a number of reports on the successful use of EPO drugs in patients with CHF and anemia. In a randomized placebo-controlled study, D. Mancini et al. [68], in which 26 patients with NYHA class III–IV CHF and Ht < 35%, along with EPO, received oral pancreatitis (325 mg) and 1 mg/day of folic acid, the Hb level increased from 110 ± 0.6 to 140 ± 1.2 g/l (p < 0.0001), and maximum oxygen consumption increased from 11 ± 0.8 to 12.7 ± 2.8 ml/min/kg (p < 0.05).
There were no significant differences in indicators in the control group. Another study [69] of patients with CHF and anemia who received recombinant human EPO (50 IU/kg 2 times a week intravenously) in combination with parenteral administration of pancreas demonstrated not only a significant increase in Hb level, exercise tolerance, according to 6-minute walk test and EF, but also significantly better survival over the 3-year follow-up period (16 out of 29 people compared to 7 out of 26, p < 0.05, HR = 1.27).
A decrease in the FC of CHF, a decrease in the need for intravenous diuretics, a decrease in hospitalization and stabilization of renal function in combination with a significant increase in EF during therapy with EPO drugs in combination with parenteral administration of the pancreas were also noted in the study by D. Silverberg et al. [70].
Most studies have administered intravenous PGs, which are considered by many to be superior to oral PGs. However, the effectiveness of PZ for oral administration is largely determined by the bioavailability of a particular drug. Thus, in one of the studies, it was not possible to note significant differences in the dynamics of the increase in Hb levels in patients with IDA treated with oral Fe salt preparations (Sorbifer Durules) or intravenous iron-containing complexes (Ferrum Lek) [71]. Taking into account these data, oral supplements should take a wider place in various clinical situations requiring correction of Fe deficiency, including in the treatment of EPO in patients with CHF with anemia.
2.4. Pancreas with anemia while taking antiplatelet agents
The problem of prescribing pancreatic cancer to patients receiving antiplatelet agents and anticoagulants has two clinical aspects. On the one hand, one of the complications of antiplatelet therapy in patients with coronary artery disease is bleeding with the development of iron deficiency anemia, which requires timely diagnosis and prescription of prostate cancer. However, only about half (48.4%) of hospitalized patients with coronary artery disease with the presence of IDA receive pancreatic cancer and a significantly smaller number (24%) of patients in the cardiac intensive care unit. As for patients with mild IDA, only 6.5% of patients receive pancreatic cancer [12].
On the other hand, existing anemia, especially with a significant decrease in Hb (Ht) levels, is considered, along with other signs (diabetes mellitus, heart failure, creatinine level, blood pressure, etc.) to be one of the predictors of bleeding during treatment with antiplatelet agents (CRUSADE scale) . This, for obvious reasons, limits doctors in the use of anticoagulants and antiplatelet agents that are vital for patients with coronary artery disease.
Indeed, the frequency of prescription of anticoagulants to patients with ACS with and without ST segment elevation in the presence of mild hypochromic anemia is 97.1 and 93.1%, while for moderate anemia and severe IDA – 39.9 and 4.3% respectively [12].
Thus, the presence of anemia in people with cardiovascular pathology poses a serious problem both from the point of view of deciphering the pathogenetic connection with the underlying disease and in the management of this category of patients. Regardless of whether anemia is a true comorbidity or turns out to be pathogenetically associated with cardiac pathology, in each specific situation timely diagnosis of anemia, verification of the pathogenetic variant and the reasons for its development, and adequate correction with the help of antianemic, mainly iron-containing, drugs are necessary.
When should you pay attention to your health?
Any healthy person should undergo a minimum preventive examination once a year, which includes a general blood test.
If the hemoglobin level is below 120 g/l, you should consult a physician.
Anemia with a hemoglobin level above 100 g/l is considered mild and does not pose a serious danger to the body at the time of detection, but still requires correction. If the hemoglobin level is 70-80 g/l and below, it is necessary to take urgent measures, because This condition poses serious threats to health, and sometimes life!
For the reasons for the development of anemia, the leading position is occupied by iron deficiency anemia - every 12th person in the world suffers from iron deficiency anemia, and among all anemias, iron deficiency anemia reaches 80% in frequency.
What is associated with the development of iron deficiency anemia? The reasons may be an elementary deficiency of iron in food, impaired absorption of iron in the gastrointestinal tract (for example, with gastritis with low acidity) and chronic bleeding.