Hyperchromic anemia
– a group of blood diseases with a color index above 1.15, characterized by impaired hematopoietic function.
Hyperchromic macrocytic anemia includes the following diseases:
— B12-deficiency anemia;
— Folate deficiency anemia;
— Myeloplastic syndrome.
- Symptoms of folate deficiency anemia
- Symptoms of myelodysplastic syndrome
Macrocytic anemia
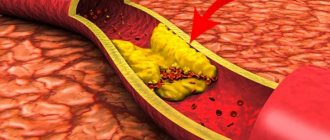
Anemia is a pathological syndrome characterized by a decrease in the level of hemoglobin in the blood, causing dysfunction of the hematopoietic system and oxygen transport, and the development of hypoxia.
Macrocytic anemia is characterized by an abnormal increase in red blood cells (macrocytosis) to a volume of ≥ 100 fL/cell (femtoliters per cell) when the norm is 80–100 fL. Due to the increase in size of red blood cells, their concentration in the blood decreases, which leads to a decrease in hemoglobin content. As a result, the blood does not receive the required amount of oxygen.
The degree of saturation of red blood cells with hemoglobin is determined by the color index of blood cells. Normally it is 0.86–1.1. Based on deviations from the coefficient, pathology is divided into 2 types:
- Macrocytic hypochromic anemia - color index below 0.86. It is divided into thalassemia and iron deficiency anemia.
- Hyperchromic macrocytic anemia – color index more than 1.1. It is divided into myelodysplastic syndrome, folate deficiency and vitamin B12 deficiency anemia.
Normochromic anemia is also distinguished, in which CP is within normal limits, but there are other pathological processes in the body, for example, bleeding, bone marrow disease, extramarrow tumor, etc. This category includes posthemorrhagic and hemolytic anemia.
The role of the CPU color index
If pallor or hypochromia of red blood cells occurs, then they become very pale, and the amount of light color in the center of the red blood cells, and the width of this zone, is significantly increased.
The color index, or a measure of the saturation of red blood cells with hemoglobin, helps to quantify the degree of hypochromia of red blood cells. If the blood color index is less than 0.8, then this morphological diagnosis can be made with confidence. In case if:
- the blood is “healthy” and does not contain hypochromic red blood cells, then the color index value will be above 0.85 and below 1.05. This is an acceptable hemoglobin content that is capable of normal gas exchange;
- the color index is less than 0.8, and there is a normal amount of red blood cells - this means that each of them or almost all of them has less hemoglobin than necessary and there is the presence of hypochromia;
- Sometimes the opposite picture occurs - hyperchromia, when the color index is higher than 1.1.
When the color index is very high and exceeds the norm, amounting to 1.4 or more, then we can talk about a deficiency of cyanocobalamin (vitamin B12). Such hyperchromic anemia is an indicator of vitamin deficiency and is called pernicious.
Causes of macrocytic anemia
The disease usually develops due to a deficiency of vitamin B12 (cyanocobalamin) or B9 (folic acid).
A deficiency of these compounds often occurs with an unbalanced diet. Vegetarianism is a risk factor, since cyanocobalamin is found mainly in products of animal origin.
In some people, vitamins enter the body, but are not absorbed. Possible causes of this pathology:
- autoimmune disorders;
- inflammatory diseases of the small and large intestines;
- intestinal malabsorption;
- malignant formations;
- excessive alcohol consumption;
- addiction.
Acute and chronic macrocytic anemia is possible against the background of the following diseases:
- hypothyroidism;
- metabolic disorders;
- diseases of the liver (for example, cirrhosis) and spleen;
- leukemia;
- rare metabolic disorders;
- acquired sideroblastic anemia.
The risk group includes people with a hereditary predisposition, alcoholism, smokers, pregnant women and patients taking medications that disrupt DNA synthesis (antitumor drugs and immunosuppressants).
Due to their origin, macrocytosis is conventionally divided into two large groups:
- Megaloblastic - occurs with vitamin deficiency.
- Non-megaloblastic - develops against the background of various diseases and clinical conditions that are not fully understood. Usually these are disorders associated with an increase in the area of the red blood cell membrane, which is characteristic of chronic pathologies of the liver and spleen.
Mechanisms of hematopoietic damage
Vitamin B12 and folates (folic acid salts) perform an important function in the synthesis of cell DNA: they are essential enzymes, without which the biochemical process stops. It is impossible to accumulate a sufficient amount in the liver. The body needs constant replenishment of the necessary components.
Pathology develops gradually when all reserves are exhausted. During the process of hematopoiesis, the division of erythroblast cells is disrupted. They turn into megaloblasts. A similar type of erythrocyte germ was present in humans in the embryonic state.
Symptoms
At the initial stage of the disease there are no symptoms. They develop gradually as normal red blood cells decrease in the blood. Regardless of the form, the main manifestations of the pathology are the same:
- general weakness;
- fast fatiguability;
- frequent headaches;
- dizziness;
- sleep disorders;
- noise in ears;
- flashing “flies” before the eyes;
- cardiopalmus;
- shortness of breath, especially during physical activity;
- loss of appetite;
- pale skin;
- decreased concentration;
- depression;
- fainting.
With B12 deficiency, the following disorders are often observed: memory loss, tingling or numbness in the hands, muscle weakness, gait instability, paresthesia, difficulty walking.
With megaloblastic anemia, glossitis, indigestion, and anorexia may occur.
B12-deficiency anemia of the elderly, or “old people always have cold feet”
Anemia caused by a lack of vitamin B12 has been known to medicine for a long time, and was previously considered incurable, leading to the death of the patient for several months. Today, the problem is not treatment, but the identification of pathology in the elderly, for whom it is typical. Indeed, for this category of patients, most of the symptoms of B12-deficiency anemia are “a common consequence of old age”, and therefore are not a reason for examination.
10 times more likely in older people
B12-deficiency anemia at a young age is a fairly rare phenomenon, mainly due to a complete rejection of “animal” products or impaired absorption of vitamin B12 and occurs in approximately 0.1% of the population.
In the elderly, the prevalence of this pathology is 10-20 times higher, and is already 1-2% under the age of 75, and about 4% among representatives of the older group.
Moreover, this B-12-induced anemia is a rather multifactorial disease, and among the main reasons for its development:
- lack of intrinsic factor Castle (produced by the stomach and necessary for the absorption of B12 from food),
- B12 deficiency in diet
- severe intestinal dysbiosis or helminthiasis.
Castle's intrinsic factor deficiency
It is not for nothing that this pathology ranks first among the causes of B12-deficiency anemia in the elderly, because the absorption of B12 in the intestines is possible only in combination with the “gastric” factor.
In other words, the absorption of vitamin B12 is severely impaired during atrophy (atrophic gastritis) or resection (removal of part of an organ) of the stomach. While atrophic gastritis occurs in the elderly with a frequency of 70-80%.
The causes of atrophic gastritis are also varied. But in the elderly, autoimmune aggression plays a significant role in this.
Antibodies to the parietal cells of the stomach or Castle factor itself are found in 90% of patients with atrophy of the gastric mucosa. However, today it is not clear whether they are an independent cause of such gastritis, or whether they develop against the background of an existing disorder.
Heredity
Many clinicians pay attention to the “continuity” of the risk of B12 deficiency among close relatives. After all, 20-30% of patients with anemia and atrophic gastritis in the family already had (or have) similar diseases.
In addition, among patients without a family predisposition, the average age of onset of B12 anemia is 66 years, and with a family history - 51 years.
B12 deficiency in diet
It's no secret that older people often develop a penchant for plant-based foods. While the consumption of meat and dairy products, as well as eggs, is greatly reduced or stopped altogether. But these foods are an essential source of vitamin B12, which also explains the frequency of B12 anemia in vegetarians.
Intestinal dysbiosis or “worms”
Vitamin B12 deficiency can also be caused by “simple competition”, since bacteria and parasites are quite “voracious” in relation to it.
At the same time, the “accelerated” proliferation of bacteria is facilitated by the tendency of older people to constipation and the frequency of intestinal diverticulosis. And among helminthic infestations, the wide tapeworm is of greatest importance.
How to suspect B12 deficiency
Weakness, fatigue, rapid heartbeat and other “classic” (iron deficiency) signs of anemia are very weakly expressed with a lack of B12. And, in most cases, they are forced to see a doctor only when they reach a severe degree of severity (hemoglobin at a level of 60-40 g/l or less).
At the same time, among the complaints that provoke seeking help are symptoms of worsening concomitant diseases (angina pectoris, arrhythmia, ischemic heart disease and others), the decompensation of which is due to prolonged oxygen deprivation of tissues (hypoxia) and impaired blood flow.
Another, almost obligatory, sign of B12 deficiency anemia in the elderly is damage to peripheral nerves, or funicular myelosis.
True, signs of such neuropathy are revealed only after a thorough examination, because:
- weakness in limbs
- constant feeling of cold in the legs,
- numbness,
- tingling
- and sensory impairment
according to the elderly patients themselves, “the phenomenon is normal at this age,” and “old people’s feet always get cold.” This means that such symptoms “definitely” cannot be a reason for examination.
Survey
1. Clinical blood test
The “blood picture” with B12 deficiency is characterized by a decrease in red blood cells, hemoglobin, an increase in erythrocyte indices (MCV, MCH), as well as a lack of platelets and leukocytes.
Red blood cells, in this case, are characterized by irregular shape and/or size (macrocytosis). And the appearance of such deviations is due to the enormous importance of vitamin B12 for normal DNA synthesis.
With B12 deficiency, the most actively dividing cells obviously “suffer” more, and one of such systems is the hematopoietic one.
2. Blood test for vitamin B12
The appearance of characteristic abnormalities in the general blood test, it is necessary to clarify the cause of their occurrence. Because not all macrocytic anemias are of B12 deficiency.
3. Confirmed vitamin B12 deficiency obviously needs to determine the reasons on which the effectiveness of further treatment obviously depends:
- examination of the stomach complex “Gastrocomplex” (0.H84.201) to detect mucosal atrophy (laboratory “analog” of FGDS),
- blood test for antibodies to parietal cells of the stomach (0.A56.201) and Castle factor (9.0.A57.201);
Diagnostics
Due to the absence of specific clinical manifestations of the disease, the only way to establish a diagnosis is laboratory tests:
- a general analysis (smear) reveals a low level of hemoglobin, hypo-, normo- or hyperchromia;
- biochemical analysis allows you to determine the presence or absence of folic acid or cyanocobalamin deficiency;
- A peripheral blood smear reveals a high level of red blood cell distribution and macrocytic changes in red blood cells.
Since macrocytic anemia can be caused by various pathologies and diseases (in fact, it is their symptom), a comprehensive diagnosis is carried out to determine the exact cause - ultrasound, CT, MRI, X-ray, endoscopy, gastroscopy and a number of other studies. Quite often, anemia is discovered by chance when examining a patient for another reason.
Hyperchromic anemia in myelodysplastic syndrome
Myelodysplasia syndrome was isolated due to characteristic hyperchromic changes in the blood after chemotherapy and radiation exposure to the bone marrow in the treatment of tumors and leukemia.
In this case, a toxic effect occurs on the process of hematopoiesis in brain cells. Against the background of severe symptoms of the underlying disease, the patient develops:
- dyspnea;
- increased fatigue;
- severe dizziness and tachycardia at the slightest exertion.
The diagnosis is made based on a typical blood picture.
Treatment of macrocytic anemia
The therapeutic regimen is developed individually for each patient, depending on the severity of the condition and the cause of the pathology.
In mild forms caused by vitamin deficiency, a correction of the diet is sufficient. The diet should contain large amounts of animal protein, vitamins and iron. Patients are prescribed vitamin preparations to treat macrocytic anemia, such as B12 Ankermann (source of cyanocobalamin), Folacin (source of folic acid).
In moderate and severe forms, the patient is hospitalized and vitamins are administered parenterally.
If anemia is a consequence of any disease, appropriate therapy is required.
If the hemoglobin level decreases excessively, red blood cell transfusion is performed.
Prevention
Following the principles of a healthy diet, maintaining a good level of vitamins B9 and B12, and iron is the simplest and most important way to protect against hyperchromic anemia, especially for pregnant women. The diet used to treat it is also preventive in nature. Additionally worth:
- visit a gastroenterologist regularly;
- exercise;
- stop smoking;
- do not contact with pesticides;
- to walk outside;
- promptly treat infectious diseases and remove parasites;
- take vitamin and mineral complexes.
Complications
Low hemoglobin levels also mean lack of oxygen. Because of this, tachycardia develops and blood pressure rises. If treatment is not started, this can lead to degeneration of tissues and organs, circulatory disorders, myocardial dystrophy with an increase in heart size, and heart failure.
Vitamin B12 deficiency causes various neurological diseases.
If the pathology is caused by bone marrow pathologies, there is a risk of developing leukemia.
Blood picture
In peripheral blood it is found:
- a sharp decrease in the number of normal red blood cells;
- moderate leukopenia and thrombocytopenia;
- In the blood smear, various erythrocytes (megalocytes, megaloblasts) changed in structure, size and shape are visible; in them, an experienced laboratory technician finds typical nuclear Jolly bodies and rings (due to the parietal location of the nucleus).
The tongue is distinguished not only by its crimson hue, but also by its smoothness of the pattern and swelling
Stages of iron deficiency
Currently, there are several stages of iron deficiency:
1. Predisposition to the development of iron deficiency (vegetarianism, adolescence in combination with menstrual irregularities in girls, frequent childbirth, the presence of chronic diseases of the gastrointestinal tract or female reproductive system associated with blood loss).
2. Pre-latent iron deficiency. At this stage there are no laboratory criteria for iron deficiency, however, an increase in the absorption of 59Fe3+ in the gastrointestinal tract can be determined, which can exceed 50% (normally 10-15%).
3. Latent iron deficiency. It is characterized by the development of sideropenic syndrome, a decrease in iron reserves in the body according to laboratory tests.
4. WAITING. The diagnosis is established when the hemoglobin concentration decreases to less than 120 g/l in women and 130 g/l in men.
Health implications
In childhood, hyperchromic anemia is dangerous due to delayed mental and physical development. The child will be more susceptible to various diseases, his immunity will not be able to cope with infections. Such children get sick for a long time and seriously.
Anemia is dangerous for pregnant women who may experience premature labor. The fetus will suffer from a lack of nutrients, the child may be born with underweight and developmental abnormalities. Therefore, during pregnancy you need to regularly visit an obstetrician-gynecologist.
Other consequences of anemia include: cardiomyopathy, tachycardia, heart failure. Therefore, treatment of this disorder must be timely.
Author of the article:
Shutov Maxim Evgenievich |
Hematologist Education: Graduated from Kursk State Medical University in 2013 and received a diploma in General Medicine. After 2 years, he completed his residency in the specialty “Oncology”. In 2021, she completed postgraduate studies at the National Medical and Surgical Center named after N.I. Pirogov. Our authors
Epidemiology
IDA was first described by the German physician J. Lange in 1554, and drugs for its treatment were first used by T. Sydenham in the 17th century. Anemia that develops as a result of iron deficiency in the body is the most widespread in clinical practice. According to WHO, about 2.5 billion people on Earth have hidden iron deficiency and 1 billion people suffer from IDA.
In women it is observed 2–5 times more often than in men; children are in 2nd place in frequency of occurrence.
The influence of IDA on the increase in the incidence of maternal and child mortality has been reliably proven. IDA occurs in 12–13% of children aged 6 months and older. up to 2 years. In developing countries, this figure is much higher: in India and African countries it reaches 72–76%. In developed countries of Europe and North America, IDA is detected in 7.5–11% of all women of childbearing age, and 20–25% have hidden tissue iron deficiency. The frequency of IDA is significantly higher in the countries of Asia, Africa and Latin America, where it reaches epidemic levels and amounts to 45–60%. Of all anemias encountered in clinical practice, about 80% are iron deficiency. In the Russian Federation, there is no information on the frequency of IDA, however, according to our data, in Moscow its frequency is 30–35% among women of childbearing age, and hidden iron deficiency is up to 60%.