Causes of esophageal varicose veins
The disease develops against the background of increased pressure in the portal vein (also known as the portal vein), but other pathologies (hypertension, congenital anomalies, and so on) can contribute to its occurrence. Esophageal varicose veins, the causes of which lie in pathological changes in the portal vein, often begin to progress with previously diagnosed severe diseases of the liver or pancreas - cirrhosis, tumors, insufficiency. The disease often develops against the background of severe diseases of the thyroid gland, in which case we will be talking about pathological disorders of the vena cava.
According to statistics, esophageal varicose veins are more often diagnosed in men aged 50 years and older.
Liver cirrhosis (LC) is a diffuse process characterized by fibrosis and the formation of nodules that develop as a result of necrosis of hepatocytes [8]. Among the causes of the disease, the first place is occupied by alcoholic cirrhosis (about 40%), the second is viral diseases [1].
In addition to the clinical manifestations of the underlying disease, two leading syndromes are observed in cirrhosis: hepatic cell failure and portal hypertension. The severity of these syndromes determines the prognosis and treatment tactics [4, 6]. The main causes of death in patients with decompensated cirrhosis are bleeding from varicose veins of the esophagus and stomach, encephalopathy, infectious complications (spontaneous bacterial peritonitis) and hepatorenal syndrome. It must be emphasized that CP is a multidisciplinary problem. Treatment of manifestations and complications of cirrhosis is within the competence of doctors of several specialties - therapists, gastroenterologists, surgeons, resuscitators. The patient’s life depends on the consistency and continuity of their actions. Indeed, when bleeding occurs from the esophagus and stomach, not only surgical tactics are important, but also how quickly the patient is hospitalized in the intensive care unit and intensive care is started.
Bleeding from the esophagus and stomach is based on portal hypertension, which is understood as the syndrome of high pressure in the portal vein basin associated with impaired blood flow in the portal vessels, hepatic veins and inferior vena cava.
The circulatory system in the liver has its own characteristics. Blood enters the liver from the hepatic artery (͌30%) and portal vein (͌70%), the total blood flow is about 1500 ml/min. Under physiological conditions, almost all portal blood flows through the hepatic veins, but with cirrhosis this figure can decrease to 20%. The portal vein is connected by numerous anastomoses with the vena cava (portocaval anastomoses), which include anastomoses with the veins of the esophagus and veins of the stomach, rectum, periumbilical veins and veins of the anterior abdominal wall. Anastomoses play an important role in the development of collateral circulation in case of outflow disorders in the portal vein system.
The pathogenesis of portal hypertension is associated with an increase in hydromechanical resistance of the corresponding section of the vascular bed. Normally, the pressure in the portal vein is about 3-7 mm Hg; portal hypertension is diagnosed when the pressure exceeds 12 mm Hg. Increased resistance to portal blood flow leads to the formation of portosystemic collaterals. They divert part of the portal blood flow from the liver, which helps reduce portal hypertension, but not completely eliminate it.
The pressure in the portal system can be expressed by the following equation: P = Q R, from which it follows that the blood pressure in the portal system (P) is equal to the product of the volume of blood flow (Q) and the resistance (R), therefore an increase in pressure can occur both due to an increase blood flow volume and due to resistance. With a proportional decrease in one factor and an increase in another, the pressure does not change [7]. With cirrhosis, the pressure in the portal system increases due to both an increase in vascular resistance and an increase in the volume of portal blood due to dilation of the vessels of the internal organs against the background of hyperdynamic syndrome. The increase in vascular resistance is caused by two factors - the development of connective tissue and the restructuring of blood flow in the liver (mechanical factor) and the reversible contraction of smooth muscle fibers of the vascular wall under the influence of nervous and humoral regulation (dynamic factor).
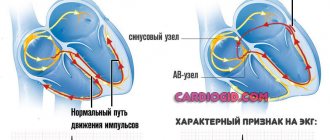
The existing classification of portal hypertension is based on data on the localization of the blockade of portal blood flow. In accordance with this, the following forms of portal hypertension are distinguished: suprahepatic, intrahepatic and subhepatic.
The suprahepatic form of portal hypertension is associated with blockade of hepatic outflow. It most often occurs with Budd-Chiari syndrome (hepatic vein thrombosis). The outcome of this condition is usually CPU.
The subhepatic form of portal hypertension is caused by blockade of the portal inflow. There are primary subhepatic portal hypertension, which occurs due to portal vein thrombosis, and secondary, which is a consequence of the involvement of portal vein vessels in the occlusive process due to neoplasms or inflammation of the pancreas. The development of portocaval and porto-portal anastomoses is typical for these processes.
The most common development is intrahepatic portal hypertension, which occurs during cirrhotic transformation of the liver. With cirrhosis, a significant restructuring of the cellular and vascular architecture of the liver occurs. Nodular regeneration of the liver disrupts the normal drainage function of the branches of the hepatic veins. In addition to the above, as a result of the replacement of the liver parenchyma with connective tissue, a reduction in the intrahepatic branches of the portal vein occurs, leading to an increase in pressure in the portal vein system and the active functioning of portocaval anastomoses. When the normal structure of the liver is disrupted, the sinusoidal network of the hepatic lobules also undergoes significant changes. In this case, anastomoses are formed between the branches of the portal vein, the hepatic artery and the branches of the hepatic veins, i.e. direct portohepatic shunts develop. Thus, collateral circulation in cirrhosis occurs not only through intrahepatic shunts, but also through extrahepatic portacaval anastomoses. A significant portion of the blood passes through the liver, bypassing the active parenchyma. The reduction in effective hepatic blood flow can reach 50%. Blood circulation bypassing the active liver parenchyma significantly impairs the metabolism of liver cells.
It is necessary to point out that the clinical manifestations of portal hypertension syndrome are varied, but most often recorded are varicose veins of the esophagus and stomach, ascites, hepatic encephalopathy and hepatorenal syndrome. For clinicians, a very important diagnostic criterion is the occurrence of signs of portal hypertension in the form of bleeding from the esophagus and stomach. As pressure increases, varicose veins gradually transform and vasculopathy develops. Against the background of a progressive deterioration in the conditions of blood outflow from the portal vein basin, portal hypertensive crises occur, which serve as a trigger for bleeding from the esophagus and stomach.
The risk of bleeding depends on the level of portal pressure, the threshold is 12 mmHg. is usually critical for the occurrence of bleeding; it is this indicator that is used in the treatment of portal hypertension. The probability of venous wall rupture correlates with its tension and is described by Laplace’s law, according to which wall tension (T) is defined as the gradient between intravascular (Pi) and extravascular (Re) pressure (Pi-Re) and the ratio of the vessel radius (r) to vascular wall thickness (w):
T=(Pi-Pe)·r/w.
Endoscopic assessment of the risk of bleeding depends on the presence of inflammatory changes in the mucous membrane of the esophagus and stomach, the size of the lesions of the veins and the presence of signs of high tension in their walls: cherry red spots and blood cysts (English - cherry red spots, varices on top of the varices) [1, 8].
At the time of diagnosis of cirrhosis, 50% of patients have varicose veins of the esophagus and stomach. The risk of developing varicose veins is higher in patients with alcoholic cirrhosis. In the first year, bleeding from varicose veins occurs in 12% of patients. The mortality rate for the first episode of bleeding is 20-25%. A second episode of bleeding develops in 60% of patients, and the probability of death is 20-35% [10, 12].
If bleeding occurs from the esophagus and stomach, intensive therapy is carried out aimed at correcting hemodynamic disturbances associated with hypovolemia [4]. In the intensive care unit, the central vein is catheterized, vital signs, hemoglobin, hourly diuresis, creatinine, urea, electrolytes, and coagulogram are monitored. The first stage of treatment is infusion therapy aimed at replenishing the volume of circulating blood, which includes transfusion of solutions of colloids and crystalloids, red blood cells, hemostatic therapy, the use of fresh frozen plasma and platelet mass in the presence of hemostasis disorders. A nasogastric tube is inserted to control bleeding and gastric lavage. All patients with suspected bleeding from the cervical vein undergo an emergency endoscopic examination of the esophagus and stomach.
It should be noted that bleeding from the esophagus and stomach during cirrhosis has an extremely adverse effect on the function of hepatocytes, since it causes a decrease in oxygen delivery to cells due to anemia. At the same time, the load on the liver increases due to increased intoxication due to the breakdown of blood in the intestines.
Many different methods have been proposed to stop bleeding from varicose veins of the esophagus and stomach, which are essentially based on two principles: 1) reducing pressure in the portal system with medication or using shunt operations, 2) obliterating varicose nodes and balloon tamponade. Based on this, methods of achieving hemostasis during bleeding from varices can be divided into 4 groups: pharmacological, endoscopic, balloon tamponade and surgical. At the same time, all methods of stopping bleeding are not able to influence the course of the underlying disease, since they affect the effect, not the cause. Stopping the bleeding only allows patients with cirrhosis to survive this episode. They often die later from other complications. Today, the only possible radical solution to the problem under consideration is liver transplantation.
For the purpose of nonspecific prevention of bleeding from the esophagus and stomach, patients with cirrhosis should stop taking aspirin and non-steroidal anti-inflammatory drugs. Routine use of H2 receptor blockers and proton pump inhibitors is recommended.
For primary prevention of bleeding from varicose veins in patients with portal hypertension, non-selective β-blockers (propranolol, nadolol, timolol) are used [5]. The mechanism of reduction in portal vein pressure when taking these drugs is associated with constriction of the vessels of the internal organs and, to a lesser extent, with a decrease in cardiac output. Indications for the use of β-blockers are the significant size of the varices and the presence of red spots on the nodes detected during endoscopic examination. During treatment, it is advisable to maintain portal vein pressure less than 12 mm Hg. A promising method for assessing therapy is to determine the intrahepatic venous pressure gradient, however, this method is invasive and cannot be widely used in medical institutions. Indirect confirmation of the effectiveness of β-blockers can be a decrease in heart rate at rest by 25% (but not less than 55 beats per minute without concomitant arterial hypertension). It has been established that non-selective β-blockers reduce the risk of bleeding from esophageal and gastric varices by approximately 45%; data on their effect on mortality are contradictory [2, 20].
For the primary prevention of bleeding in medium- and large-sized varices, endoscopic vein ligation has also been attempted. However, it has been shown that the effectiveness of β-blockers and ligation did not differ [18], so the administration of β-blockers has advantages due to the economic component and the complexity of the ligation technique.
When bleeding from the varicose vein occurs, vasoactive drugs are widely used, with the help of which they achieve a decrease in pressure in the portal vein and a decrease in the tension of the varicose vessel wall. According to the mechanism of portal pressure reduction, they can be divided into two groups. The first group includes vasodilators that affect the dynamic component of portal resistance (nitrates - isosorbitol 5-mononitrate). However, these drugs are rarely used as monotherapy (including due to the hypotensive effect); they are usually used in combination with vasoconstrictors. The second group includes vasoconstrictors, which reduce portal pressure due to splanchnic vasoconstriction and, accordingly, a decrease in portal blood flow.
Direct vasoconstrictors include vasopressin and its synthetic analogue terlipressin. These drugs act directly on the smooth muscle cells of blood vessels. The mechanism of action of indirect vasoconstrictors - somatostatin and its synthetic analogue octreotide - is explained by inhibition of the activity of endogenous vasodilators (in particular, glucagon).
Vasopressin was one of the first drugs used to reduce portal pressure and control bleeding from varicose veins. It causes spasm of the arterioles of the internal organs and a decrease in portal blood flow. However, the use of vasopressin was abandoned due to the large number of side effects inherent in the drug, and primarily due to the possibility of causing ischemic changes in the myocardium.
Currently, terlipressin (N-triglycyl-8-lysine-vasopressin), a synthetic analogue of the posterior pituitary hormone vasopressin, is widely used in clinical practice. Terlipressin differs from vasopressin by three additional glycine residues connected to the N-terminus of the molecule and by the substitution of lysine at the eighth position of arginine. The pharmacological effect of terlipressin is manifested by the vasoconstrictor effect of arterioles, venules and veins of the visceral organs, which leads to a decrease in portal blood flow and a decrease in portal pressure. Changing the chemical structure of vasopressin helped to increase the duration of action of the drug and reduce side effects. This allows it to be administered as a bolus rather than as a long-term intravenous infusion.
The effectiveness of terlipressin has been proven in numerous clinical studies. It was found that a single administration of the drug in a dose of both 1 mg and 2 mg leads to a decrease in pressure in the portal vein within 4 hours. In addition, after bleeding stopped, the administration of terlipressin 1 mg every 4 hours for 5 days significantly reduced the risk of recurrent bleeding. bleeding [14].
Based on a meta-analysis of 20 randomized studies on the effectiveness and safety of terlipressin in patients with bleeding from the esophagus and stomach, it was concluded that the use of the drug reduces overall mortality by 34% compared with placebo. Side effects are minimal and terlipressin is as well tolerated as octreotide and somatostatin [19].
When comparing terlipressin with somatostatin in patients with cirrhosis, the former drug was more effective. When terlipressin was prescribed, bleeding control was recorded in 91% of patients, and in the somatostatin group - in 81% [25]. In another study, standard doses of terlipressin were used to stop bleeding from varices in patients with cirrhosis. To achieve comparable results in the control group, increased doses of somatostatin were required [26].
In studies devoted to a comparative study of the effect of terlipressin and octreotide on the magnitude of portal hypertension, it was found that terlipressin significantly and lastingly reduced pressure in varicose veins. However, the effect of octreotide was short-lived; repeated administration of octreotide did not prolong or maintain its effects [15, 21].
Analysis of modern methods of stopping bleeding from varicose veins allowed J. Bosch et al. [11] conclude that terlipressin is the drug of choice, since it is the only drug that can improve survival in this pathological condition.
In modern clinical practice, endoscopic sclerotherapy is often used for emergency treatment of bleeding from the esophagus and stomach. It can be performed immediately during the first diagnostic endoscopy or delayed until the bleeding has stopped using conservative methods. During the procedure, a needle is passed through the endoscope channel, through which a sclerosing solution is injected either into the varicose nodes or in close proximity to them. This leads to the formation of scar tissue and vascular thrombosis. Usually the procedure is performed several times, achieving complete obliteration of all nodes present in the patient, which takes from several days to several weeks. The effectiveness of this method ranges from 70 to 90% [23]. However, endoscopic sclerotherapy to stop bleeding from the esophagus and stomach may be accompanied by a number of complications. A transient disorder of esophageal motility has been described. A more serious complication is persistent dysphagia associated with the formation of scar structures, the risk of which depends on the number of injections and the amount of sclerosant administered [22]. Also, after sclerotherapy, ulcers of the esophageal mucosa may occur, which can lead to both bleeding and necrosis of the wall, followed by perforation and the development of mediastinitis [9].
Recently, the technique of ligation of esophageal varices of the esophagus, proposed in 1986 by G. Stiegmann, has begun to be used. It was more effective in recurrent bleeding than sclerotherapy [24]. To implement this technique, an endoscope with a special ligating device is required. During the procedure, the varicose vein is aspirated into a ligation device and an elastic ring is placed on it. The method is simple to perform and has fewer complications than sclerotherapy.
Temporary control of bleeding can be achieved with balloon tamponade using a Sengstaken-Blakemore obturator probe or self-expanding esophageal stents. The use of balloon tamponade, according to modern data, is considered justified if it is necessary to transport a patient with bleeding or if it is impossible to use other treatment methods, in particular with massive bleeding, when sclerotherapy is difficult due to poor visibility. The total time that the Sengstaken-Blakemore probe is in the esophagus should not exceed 24 hours, since its further stay can lead to ulceration of the mucous membrane of the lower parts of the esophagus.
When choosing treatment tactics for patients with bleeding from the esophagus and stomach, preference is given to the use of terlipressin. In Europe, a standard management scheme for such patients has been developed [13]. In Russia, this opportunity appeared in 2012 with the registration of the drug remestipa (terlipressin). Conventional methods of intensive care, including infusion-transfusion therapy and constant monitoring of vital functions of the body, are supplemented with the administration of terlipressin. The drug is administered intravenously at a dose of 1 mg when a diagnosis of bleeding from the esophagus and stomach is established. Repeated doses are prescribed every 4 hours. On the 2nd day, nutritional support with liquid nutritional mixtures begins, followed by a transition to a salt-free diet. In parallel, to prevent infectious complications, 400 mg of norfloxacin is prescribed per os every 12 hours. Terlipressin therapy usually lasts 2-5 days. At the same time, ligation of the varicose veins is performed, although endoscopic sclerotherapy is allowed in the absence of technical capabilities [16]. Subsequently, the patient is discharged with recommendations to take β-blockers and subsequent planned courses of ligation of varicose veins.
If drug therapy and endoscopic arrest are ineffective and bleeding continues, surgical intervention is indicated. Often a good effect is achieved by gastrotomy with suturing of the esophagus and stomach. Performing surgical intervention does not exclude recurrent bleeding. In addition, with hepatocellular failure, there is a decrease in the synthesis of coagulation factors, which worsens the results of the operation, despite plasma transfusion.
Reduction of portal hypertension can be achieved by portocaval shunting. Currently, three main types of such operations are common: total, selective and partial bypass surgery [1, 17].
Total bypass surgery is performed by creating large-diameter vascular anastomoses with the portal, splenic or superior mesenteric vein. This completely eliminates portal hypertension and the threat of bleeding from the esophagus and stomach. A significant disadvantage of the operation is the occurrence of severe hepatic encephalopathy in the postoperative period.
Selective splenorenal shunting is based on the formation of a distal splenorenal anastomosis. The essence of the operation is selective bypass of the spleno-gastric region while maintaining reduced blood flow through the portal vein. As a result, the risk of developing possible bleeding due to portal hypertension is significantly reduced. The quality of life of patients after performing this operation is significantly higher than with total bypass surgery.
Partial portacaval shunting is carried out by applying a small diameter (8-10 mm) anastomosis side to side with any main vessel of the portal system. In this case, on the one hand, decompression of the portal system is ensured, sufficient to prevent bleeding from the esophagus and stomach, and on the other hand, reduced blood flow in the portal vein is maintained.
A relatively new method of stopping bleeding is transjugular intrahepatic portosystemic shunting. The method is based on the installation of a stent between the branches of the hepatic and portal veins, which leads to partial discharge of blood into the systemic circulation and a decrease in portal pressure [3]. The stent diameter is selected so that the portal pressure gradient is below 12 mm Hg. The disadvantages of the method include the development of complications in the form of stenosis and stent dislocation.
Recurrent bleeding from varicose veins and end-stage cirrhosis are indications for liver transplantation. However, previously performed portosystemic anastomoses complicate transplantation, especially if manipulations were performed at the porta hepatis.
Thus, bleeding from the esophagus and stomach is one of the most prognostically unfavorable complications of cirrhosis and portal hypertension. Methods to stop bleeding include drug vasoactive therapy (terlipressin), aimed at reducing portal pressure, and endoscopic intervention (sclerotherapy and ligation of the varices). If conservative therapy is ineffective, transjugular intrahepatic portosystemic shunting or open portacaval shunting is performed. Patients with cirrhosis and varicose vein bleeding are candidates for liver transplantation. The use of terlipressin to stop bleeding from the esophageal vein in patients with cirrhosis can reduce the number of recurrent bleeding, the number of blood transfusions and prepare patients for planned surgical interventions for portal hypertension.
Esophageal varicose veins: symptoms
Depending on the degree of development, the following signs are distinguished:
- First degree. The diameter of the veins is increased by no more than 3 mm, the formation of single nodes is possible. Diagnosis of the disease is possible only by the endoscopic method; there are no clinical signs.
- Second degree. A rather dangerous period of varicose veins of the esophagus - there are no symptoms (even the mucous membrane of the organ still remains unchanged), but at the same time the contour of the veins already becomes unclear, and X-ray diagnostics reveal thickenings on the veins (harbingers of nodules). Already at this stage, bleeding is possible, which in the absence of immediate medical attention often leads to death.
- The third and fourth degrees of varicose veins of the esophagus are characterized by severe symptoms - the patient is often bothered by heartburn, pain occurs in the sternum, shortness of breath is possible, not only during physical activity, but also at rest. Often the disease is diagnosed only in the later stages of its development, when the first bleeding appears; blood is released directly from the esophagus or found in the vomit.
Your health is in the hands of professionals!
Kreimer Vadim Dmitrievich
- Doctor of Medical Sciences, Head of the Clinic of Gastroenterology and Digestion, gastroenterologist, endoscopist.
- Professor of the European Association of Gastrointestinal Endoscopy.
- He is the author and co-author of more than 100 scientific works, including 3 monographs.
- For services in the field of medicine, he was awarded the Order of “LABORE ET SCIENTIA” (labor and knowledge) of the European Scientific and Industrial Consortium.
Pokrovsky Yuri Anatolievich
- PhD, gastroenterologist, endoscopist.
- A highly professional doctor, one of the few gastroenterologists in Russia who himself performs all examinations on his patients, including gastro- and colonoscopy.
- Dr. Pokrovsky is a certified oncologist and gastroenterologist, who has been dealing with the problems of gastrointestinal tumors for a long time.
Treatment
Treatment of varicose veins of the esophagus begins with finding out the true causes of the development of the disease. If a pathology of the liver, thyroid or pancreas is diagnosed, then it must be treated - the provoking factor must be eliminated or its influence must be weakened. Medications include vitamin complexes, antacids and astringents. If bleeding is diagnosed, there is always a risk of its reoccurrence. In this case, the following is prescribed:
- blood transfusion;
- hemostatic drugs;
- introduction of a special probe that can compress the vessels.
Varicose veins of the esophagus, bleeding in which occurs too often, require surgical treatment.
Surgery is also performed if there is no effect from therapeutic treatment. Can esophageal varicose veins be stopped in this case? The prognosis is more favorable - the survival rate of patients increases 3 times. After any treatment, you must follow the dietary recommendations of doctors, undergo regular examinations and avoid excessive physical activity.
You can find out more about what esophageal varicose veins are and which doctor you should contact on the pages of our website Dobrobut.com.
Diagnostics
The diagnosis can be suspected, but cannot be confirmed without esophagogastroduodenoscopy. This is practically the only way to establish a connection between bleeding and esophageal varices; gastric varices are often simultaneously detected.
An x-ray can reveal inflammation, tumors, spastic contraction with obstruction of patency
The procedure allows you to determine the degree of deformation of the veins, the stage of the disease, visually determine the condition of the vascular walls, and predict rupture. It is almost impossible to conduct research during bleeding.
Contrast radiography of the esophagus is routinely prescribed; before the image, the patient is given a barium mixture to drink. A series of radiographs are used to monitor the movement of the contrast and its spreading in the lumen of the esophagus.
Laboratory way:
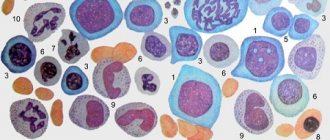
- it is necessary to determine the presence of anemia by the content of red blood cells, platelets, and color indicator;
- in case of acute bleeding, the hematocrit is calculated;
- be sure to do an analysis of clotting indicators;
- determine liver function by enzyme tests, protein, glucose, bilirubin levels; deviations in the results make it possible to suspect the influence of liver pathology on changes in the venous system of the esophagus;
- if there are signs of bleeding, the blood type and Rh factor are determined in case of a necessary blood transfusion.
Even minimal excretion of blood in the stool is confirmed by Gregersen's reaction to occult blood.
Prognosis for liver cirrhosis
Vascular disease of the gastrointestinal tract is characterized by high mortality. In cirrhosis it reaches 50%. Mortality does not depend on the nature of the bleeding, but on the severity of organ damage.
In 80% of cases, hemorrhage occurs on its own, so the likelihood of recovery is in those patients who have good liver condition. But 75% of patients are susceptible to relapse within the first two years.
To improve the condition of varicose veins, it is necessary to regularly undergo drug support and endoscopic treatment.
Although VRVP cannot be treated, the patient can live for decades if he maintains his condition with timely examinations, adjusts his diet and sleep and rest patterns. Be healthy!