Disseminated processes in the lungs mean a fairly large group of diseases and pathological conditions (more than 100 known to modern medicine), in which multiple inflammatory foci and (or) fibrotic changes are diagnosed in the respiratory organ, usually located chaotically and on both sides. Pathological changes can affect almost all pulmonary segments, or can be concentrated only in certain places, for example, around the bronchi, in the peripheral parts of the lungs, etc.
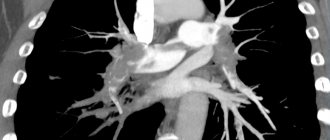
Primary disseminated lung diseases are identified based on the results of hardware medical examinations (CT, X-ray). On high-resolution cross-sectional computed tomography of the lungs (MSCT), foci of dissemination and fibrosis are best visualized. A radiologist can assess the volume of damaged lung tissue, identify fibrous cords (connective tissue adhesions and scars), accumulation of fluid and (or) pus in the alveolar vesicles, and concomitant pathologies of the respiratory tract, arteries, and lymphatic system.
In this article we will talk in more detail about pulmonary dissemination and the diseases in which this symptom is observed.
What is dissemination in the lungs?
Dissemination consists of multiple pathological foci (compressions) with a diameter of 1-10 mm. On CT scans they appear as light spots, while normally the lung tissue is visualized as an almost uniform dark color. The lesions can be completely different in size, shape (ellipsoid, with uneven edges) and morphology. Perifocal inflammation is often found around the lesions. They can merge and in this case resemble infiltrative processes in pneumonia. Dissemination also manifests itself in the form of focal micro lesions with blood and swelling.
During disseminating processes in the lungs, the respiratory organ partially (depending on the volume of damage) ceases to perform its main function - breathing and transporting oxygen to other organs, in particular to the heart and brain. With total disseminated lung damage, the patient may die.
Symptoms of pulmonary dissemination
Like most lung diseases, disseminated lung disease does not have specific symptoms that can be used to accurately diagnose it. With dissemination, patients may experience standard respiratory symptoms:
- Dyspnea;
- Cough;
- Difficulty breathing (it becomes more frequent, it becomes difficult to hold it);
- Unpleasant sensations in the chest;
- Cough;
- Loss of appetite;
- Temperature increase;
- Weakness (due to impaired respiratory function and lack of oxygen);
- Decrease in blood oxygen saturation;
- Change in blood pressure.
Causes of pulmonary dissemination
When dissemination is detected in the lungs, it is important to accurately determine the cause and identify the specifics of the pathological process. The causes of pathological processes, depending on the shape, density and nature of the distribution of lesions, can be:
- Tuberculosis;
- Pneumonia;
- Poisoning by toxic gases and drugs;
- Prolonged inhalation of industrial dust (pneumoconiosis);
- Hamman-Rich disease;
- Other types of alveolitis (including allergic);
- Goodpasture's syndrome;
- Idiopathic pulmonary fibrosis;
- Oncological diseases of the lungs or other organs (sarcoidosis, metastases, carcinomatosis, bronchoalveolar cancer);
- Acute respiratory distress syndrome;
- Vasculitis (including rheumatoid);
- Some diseases of other internal organs (heart, liver).
Note that the causative agents of infectious and inflammatory lung diseases that can cause disseminated lung damage include a large group of viruses, bacteria and fungi (mycobacterium tuberculosis, SARS-CoV-2, coccidioides immitis), etc. Sometimes it is possible to identify the exact cause of diffuse inflammatory foci and fibrosis is not possible. If the disease has symptoms similar to tuberculosis or pneumonia, or there is severe fibrosis, but even after medical examinations the cause remains unclear, then such pathological changes are called “idiopathic”, and treatment tactics are selected individually based on the data obtained and the patient’s medical history.
Therefore, disseminated lung diseases are considered quite difficult to diagnose. CT scan of the lungs is much more informative than conventional radiography, however, even this method, isolated from laboratory tests, does not provide enough information to prescribe therapy. If a pulmonologist or radiologist suspects a malignant process, a biopsy may be recommended for the patient.
Pulmonary sclerosis. Treatment and prevention
Doctors at the Yusupov Hospital prescribe small doses of glucocorticoids to patients suffering from pulmonary sclerosis for six months to a year. In the acute period of the disease, their daily dose is 20-30 mg; for maintenance therapy, 5-10 mg of prednisolone is recommended. For bronchitis, bronchiectasis and pneumonia, antibacterial and anti-inflammatory drugs are used. Among the antibiotics, macrolides (azithromycin) are the drugs of choice. To treat pneumosclerosis, doctors also prescribe cephalosporins of the second and third generation. Metronidazole is administered intravenously.
Complex therapy for pulmonary sclerosis includes the following medications:
- expectorants and sputum thinners;
- bronchodilators;
- cardiac glycosides (for circulatory failure);
- vitamins (retinol, α-tocopherol acetate and others).
Non-drug treatment methods are widely used: physiotherapy, oxygen therapy and exercise therapy. For pulmonary sclerosis at the Yusupov Hospital, patients are taught therapeutic and breathing exercises. Outside of exacerbation, sanatorium treatment is recommended. Rarely is there a need for surgery, in which surgeons remove the affected part of the lung. If necessary, this operation is performed in partner clinics.
Prevention of pneumosclerosis consists of timely treatment of colds, hardening, and an active lifestyle. Effective treatment of pneumosclerosis is possible after a comprehensive examination, which is carried out by doctors at the Yusupov Hospital, using modern diagnostic methods. If you have signs of pulmonary sclerosis, call and a consultant doctor will answer all your questions.
What diseases are characterized by the symptom of pulmonary dissemination?
Let's consider the most common diseases that can manifest as a disseminated pathological process in the lungs.
Tuberculosis
Mild tuberculosis is a fairly common, dangerous and serious disease. Its causative agent is bacteria - Koch bacilli, which are easily transmitted by contact and airborne droplets, can live for years in street dust and even in human lungs without causing any symptoms.
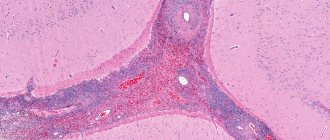
The disease manifests itself when the human immune system cannot independently restrain the active phase and growth of mycobacterium tuberculosis. Bacterial damage to the lungs in tuberculosis is usually visualized as multiple inflammatory foci - granulomas.
In the center of tuberculous granulomas there are foci of necrosis. Seals form around them - the pulmonary alveoli are filled with a liquid substrate, which contains the bacteria themselves, epithelial and plasma cells, dead lymphocytes, large Langhans cells, and macrophages.
In the initial stages, tuberculosis progresses almost asymptomatically; over time, the patient begins to notice weakness, deterioration in general health, cough and changes in breathing.
At the same time, something suspicious is rarely noted on auscultation. Sputum analysis does not show mycobacteria. Diagnosis of tuberculosis is possible based on the results of an X-ray examination and a tuberculin skin test.
Granulomatosis and diffusely located “ground glass” on CT are not a specific sign of tuberculosis. The former are also found in sarcoidosis, and the latter in pneumonia and other diseases.
To treat tuberculosis, the patient is prescribed a course of antibacterial therapy. It is important to prevent fibrosis (scarring of the lungs) as such changes can be irreversible.
Pneumoconiosis
Pneumoconiosis is a disseminated lung disease caused by inhalation of construction or industrial dust. Most often, pathological processes occur with a pronounced development of primary diffuse fibrosis, in which the pulmonary alveoli “stick together” as connective tissue grows in them.
Pneumoconiosis is also granulomatous in nature. CT scans clearly show multiple nodular densities of varying densities. Such compactions should be checked to determine whether the process is benign and whether there is an oncological threat.
Pneumoconiosis is a so-called “occupational” disease. Most often it affects:
- Electric welders;
- Builders and workers (the disease is caused by inhalation of dust from silicon dioxide, silicates, metals, carbons);
- Industrial workers (the disease is also caused by inhalation of dust from cotton, flax, grain, and some chemicals).
Silicosis is a common and severe lung disease, in which multiple diffuse fibrosis and nodular compactions are diagnosed. As a result, the patient's functional lung volume is significantly reduced. Occurs due to prolonged inhalation of dust with free silicon dioxide (contained in quartz sand and the surrounding air). Therefore, sandblasters, employees of relevant (abrasive blasting) enterprises, and residents of “sandy” regions are at risk.
Asbestosis is a chronic lung disease that also causes multiple pulmonary fibrosis. Occurs due to inhalation of asbestos dust or asbestos fibers. Employees of asbestos mining and asbestos processing enterprises are at risk.
Pneumonia and complications of pneumonia
Pneumonia is a group of inflammatory lung diseases. Against the background of this disease, the patient may experience more dangerous complications, which are also characterized by dissemination: acute respiratory syndrome (ARDS), interstitial lung disease, cobblestone symptom, honeycomb lung, pulmonary edema, fibrosis, etc.
In pneumonia with multiple diffusely located loci of damage, the vital capacity of the lungs is significantly reduced, since the inflammatory foci and infiltrates are large, the alveoli are filled with liquid exudate, not air.
Pneumonia with dissemination can be a consequence of pulmonary candidiasis, pneumoconiosis and other diseases. It is necessary to accurately establish the cause of pathological changes. Sometimes it is also necessary to exclude a malignant process (based on laboratory diagnostic results).
Sarcoidosis
Pulmonary sarcoidosis is an oncological disease. Its main features on CT are dissemination and mediastinal lymphadenopathy. Dissemination on scans is not as pronounced as with progressive tuberculosis, but there is a certain similarity. Diagnosis is complicated by pulmonary fibrosis. Along with disseminated damage to the respiratory organ, vasculitis, perivasculitis, and peribronchitis are present.
Multiple foci (from 2 mm to 1 cm) are often located along the bronchovascular bundles, interlobular fissures, costal pleura, and in the interlobular septa (perilymphatic type of dissemination). In sarcoidosis, granulomatosis is often (about 35% of cases) found not only in the lungs, but also in the bronchi. At the same time, their mucous membrane may not be changed - swelling, hyperemia, and areas of thickening of the epithelium indicate damage to the bronchi in sarcoidosis.
In the early stages, sarcoidosis develops asymptomatically; in later stages, the patient begins to be bothered by a nonproductive cough, breathing problems (for no obvious reason), discomfort and burning in the back, and heaviness in the chest.
Lung lesions in systemic connective tissue diseases
Systemic connective tissue diseases are a group of inflammatory autoimmune diseases of unknown etiology, characterized by multiple lesions of the connective tissue of various organs and systems. The process may involve all parts of the respiratory system. In some cases, lung pathology is associated directly with systemic damage to the connective tissue; in others, it is secondary. Often lesions of different types are combined in one patient, and this multiplicity of lung damage is a common feature of systemic diseases. At the same time, each disease has a unique pulmonary pathology. Systemic connective tissue diseases are progressive in nature and have a long, often severe course. Pulmonary manifestations can occur at any stage or precede the disease by several years. The leading symptoms are shortness of breath, cough and chest pain. The most common syndromes are pleural lesions and interstitial lung diseases. The dysfunction of the immune system characteristic of these diseases, as well as the use of glucocorticosteroids and cytostatic drugs in treatment, increase the body’s susceptibility to infection and contribute to the development of severe complications (pneumonia, sepsis and tuberculosis). Along with the usual pathogens of pneumonia, complications are often caused by opportunistic flora, Mycobacterium tuberculosis, viruses and fungi.
Systemic lupus erythematosus (SLE) is an autoimmune disease characterized by systemic damage to blood vessels of various sizes. SLE is characterized by the presence in the blood serum of high titers of antinuclear factors (ANF), antibodies to native DNA and Smith antigen (Sm-Ag), and low levels of complement.
Compared to other systemic diseases, lung damage in SLE is represented by the widest range of syndromes:
- pleurisy is often bilateral, often combined with pericarditis,
- acute lupus pneumonitis is observed in 1-4% of cases, combined with exudative pleurisy, accompanied by fever, shortness of breath, cough with sputum, hemoptysis (35-60% of cases),
- chronic interstitial pneumonitis,
- damage to interstitial lung tissue occurs in 3-8% of cases,
- alveolar hemorrhages,
- damage to the respiratory muscles (lung shrinkage syndrome),
- bronchiolitis obliterans,
- pulmonary vasculitis with pulmonary hypertension,
- thromboembolism of the branches of the pulmonary artery,
- infectious complications.
The clinical picture of lung damage is observed in 1-6% of cases of SLE; according to multislice computed tomography (MSCT), lung damage is already observed in 30%, and at autopsy - in 70% of cases, SLE is accompanied by lung damage.
The basis of treatment for systemic lupus erythematosus is glucocorticosteroid drugs and immunosuppressive agents. Without treatment, the prognosis is unfavorable; with adequate therapy, remission can be achieved.
Rheumatoid arthritis (RA) is a symmetrical chronic inflammation primarily of the joints of the hands and feet, accompanied by gradual destruction (destruction) of their structure. An immunological feature of RA is the production of autoantibodies of the IgM class to one’s own immunoglobulins (rheumatoid factors), which are found in the blood serum in moderate or high titers. Along with joint damage, 20-30% of patients develop extra-articular manifestations, which include rheumatoid nodules and rheumatoid vasculitis. The most typical manifestations of vasculitis are digital (digital) arteritis, skin ulcers, peripheral neuropathy and vasculitis of internal organs (lungs, heart, kidneys). The risk of death with the development of extra-articular manifestations increases 5 times. Rheumatoid arthritis is characterized by bronchiectasis and bronchiolitis, as well as damage to the pleura, pulmonary vessels (vasculitis, pulmonary hypertension), alveolar hemorrhages, and the development of interstitial lung diseases (ILD). Pleurisy is the most common lung lesion in RA; it is asymptomatic, with a small amount of effusion, and is observed in approximately 25% of patients. In a third of patients, pleurisy is associated with ILD, the course of which in rheumatoid arthritis can be very slow (10 years or more) or fulminant (fulminant, instantaneous). Rheumatoid nodules (RU) are rarely found in the lungs (in 1-2%). In 10-15% of patients, a dangerous complication develops - secondary amyloidosis, including involvement of the lungs. A more frequent development of lymphomas, myeloma and leukemia has been proven against the background of rheumatoid arthritis.
Systemic scleroderma (progressive systemic sclerosis) is a group of diseases in the early stages of which microcirculatory disorders and inflammation prevail, gradually leading to generalized fibrosis (sclerosis). Typical autoimmune disorders in systemic scleroderma are the formation of anticentromere antibodies and antibodies to the topoisomerase 1 antigen (Scl-70). The disease is characterized by a variety of appearances, the most striking of which is thickening of the skin. The diffuse form of scleroderma is characterized by acute development and rapid progression of generalized fibrosis of the skin and internal organs (heart, lungs, kidneys). A relatively benign limited form debuts with Raynaud's phenomenon (syndrome), skin changes are limited in nature, progress slowly and are accompanied by vascular ischemic disorders. Lung damage with scleroderma occurs more often than with other systemic diseases, in men more often than in women. Lung pathology with multislice computed tomography (MSCT) in patients with systemic scleroderma is observed in 80-90%. The most common diseases are interstitial lung disease (ILD) and pulmonary hypertension (PH). The cause of PH in 12-15% may also be fibrous lesions of the left parts of the heart (valve, myocardium). Pulmonary hypertension is more often associated with a limited form of the disease and is detected in patients with a long history of ILD with a diffuse form. Infectious complications (pneumonia, abscess formation) occur less frequently than with other systemic diseases. The risk of developing lung cancer against the background of systemic scleroderma increases 3-5 times.
Idiopathic inflammatory myopathies are a group of diseases whose clinical manifestations are based on inflammation of striated muscles (polymyositis, dermatomyositis, juvenile dermatomyositis, etc.). Immunological markers are myositis-specific antibodies directed to cytoplasmic proteins and ribonucleic acids. The most common antibodies are antibodies to tRNA aminoacyl synthetases (Jo-1, etc.).
Muscle damage is manifested by symmetrical weakness of the proximal (located closer to the body) muscle groups of the upper and lower extremities and muscles involved in neck flexion, which is manifested by difficulty in rising from a low chair; when boarding a vehicle; when washing and combing your hair. Characteristic damage to the muscles of the pharynx, larynx and upper third of the esophagus (dysphonia, dysphagia). Intraorgan manifestations are varied, the most common being damage to the respiratory system. Typical for myopathies is damage to the intercostal muscles and diaphragm, which leads to difficulty breathing and shortness of breath. Pneumonia complicates the course of polymyositis and dermatomyositis in 30-50% of patients. The leading role in its development is played by aspiration of food associated with damage to the muscles of the pharynx and the upper third of the esophagus (aspiration syndrome). The most severe lung disease is interstitial disease (ILD), the symptoms of which precede symptoms of muscle damage in 10% of cases.