Fatty degenerations are associated with excessive accumulation of lipids (neutral fats, triglycerides, phospholipids, cholesterol) in the cytoplasm of parenchymal cells, or with their appearance in those cells where they are not normally found, or with the appearance of abnormal composition lipids in the cytoplasm of cells. A person's need for fat is 80-100 g per day.
The main functions of lipids in the body:
- structural - lipids form the basis of cell membranes;
- regulating;
- providing energy, since lipids are one of the main sources of energy.
Depending on the clinical manifestations, the following are distinguished:
- lipidoses;
- obesity;
- exhaustion.
The most common causes of acquired lipidosis are hypoxia and various intoxications. Therefore, fatty degenerations are a component of diseases accompanied by oxygen starvation. - coronary heart disease, hypertension, heart defects, chronic lung diseases (bronchiectasis, tuberculosis, emphysema). leading to the development of pulmonary heart failure. In addition, fatty degeneration is caused by various infections and intoxications, which are accompanied by both hypoxia and blockade of enzymes that catalyze lipid metabolism in cells by toxins. Lipidoses can sometimes be associated with a lack of vitamins and certain amino acids.
In pathology, fatty degenerations of the myocardium, liver and kidneys are of greatest importance.
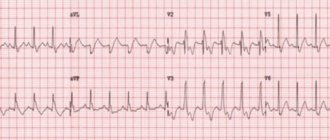
Rice. 3. Fatty degeneration of the myocardium. a — cardiomyocytes with fatty inclusions; b - venules; c — cardiomyocytes free from fatty inclusions.
Fatty degeneration of the myocardium develops by decomposition of fat-protein complexes of membranes of intracellular structures, as well as as a result of infiltration of cardiomyocytes with lipids. Regardless of the mechanism of dystrophy, small inclusions of fat first appear in myocardial cells (pulverized obesity), then they merge into droplets (small-droplet obesity), which gradually fill the entire sarcoplasm and can lead to cell death (Fig. 3).
for a sharp decrease in heart function and the development of heart failure.
Fatty liver, or fatty hepatosis
Rice. 4. Fatty degeneration of the myocardium (“tiger heart”). Yellow-white stripes are visible under the endocardium, corresponding to areas of lipid incorporation in cardiomyocytes.
At the same time, with many intoxications and infections, a mechanism of decomposition of the membranes of intracellular structures with the disintegration of their fat-protein complexes is possible. Finally, fatty hepatosis develops as a result of the transformation of proteins and carbohydrates into lipids, which is observed, for example, with chronic alcohol intoxication. In any case, in the cytoplasm of hepatocytes, mainly in the periphery of the hepatic lobules, dust-like obesity first develops, which transforms into small-droplet obesity, and then into large-droplet obesity. In this case, the nucleus and intracellular structures are pushed to the periphery of the cells, which often die. In these cases, the fatty inclusions of dead hepatocytes merge, forming fatty cysts. Macroscopic changes in the liver depend on the severity of dystrophy. In severe cases, for example with alcoholism, the liver is enlarged in size, flabby, and on a section it is ocher in color - “goose liver”. With less pronounced fatty degeneration, the liver is also enlarged in size and has a yellowish-gray color when cut. With fatty hepatosis, liver function is preserved for a long time, but as the underlying disease and fatty degeneration progresses, it decreases, sometimes quite significantly.
Fatty kidney degeneration develops by infiltration of the tubular epithelium during hyperlipidemia, observed, in particular, with nephrotic syndrome. In this situation, lipids end up in the primary urine (hyperlipiduria) and are intensively reabsorbed by tubular epithelial cells, but in such large quantities that these cells are not able to metabolize the lipids that have entered them - small droplet obesity of the tubular epithelium develops. Usually it is combined with their hyaline-droplet dystrophy. In this case, the kidneys are little changed externally, but in severe cases of the main pathological process, they acquire a grayish-yellow color, and when cut, their pyramids can take on a yellow color.
The outcome of parenchymal fatty degeneration depends on the degree of its severity - dust-like and small-droplet obesity is reversible when the cause that caused it is eliminated, large-droplet obesity can result in cell death.
Thyrotoxicosis
Thyroid hormones (triiodothyronine, thyroxine) stimulate metabolism; their excess leads to an increase in the need for oxygen and energy. The heart muscle is especially sensitive to this and begins to suffer first: myocardial dystrophy develops, as a result - specific cardiomyopathy (“thyrotoxic heart”). Thyroid hormones also have a “stimulating” effect on the heart: they increase heart rate and cardiac output.
The following symptoms may develop:
- feeling of palpitations, rapid pulse even at rest, severe fatigue;
- increased blood pressure, especially systolic (“upper” pressure), usually stable, without crises;
- there is often a significant spread between the values of systolic and diastolic pressure;
- when listening to heart sounds, the doctor can identify characteristic noises, and ultrasound examination of the heart often reveals prolapse (sagging, protrusion) of the mitral valve;
- most often there is a so-called sinus tachycardia;
- if the patient initially had a cardiac pathology, against the background of thyrotoxicosis it worsens: attacks of angina pectoris, atrial fibrillation, resistant to drug therapy (in the elderly this is sometimes the only symptom of thyrotoxicosis).
Over time, the walls of the heart thicken, its cavities expand, the heart muscle is partially replaced by connective tissue, fibrosis forms, and the contractility of the heart is impaired, which can lead to heart failure and atrial fibrillation.
Treatment:
- medicinal – thyreostatics, beta blockers, cardiac glycosides, diuretics, antiplatelet agents, etc.;
- radioiodine therapy;
- Surgical intervention is resorted to in severe cases, with low effectiveness of conservative treatment - the so-called subtotal resection of the thyroid gland is performed - i.e. removing most of it. Hypothyroidism
With decreased thyroid function, heart rate, cardiac output, and blood pressure, on the contrary, decrease. The lipid composition of the blood changes, there is an increased cholesterol content, widespread atherosclerosis, especially of the heart vessels. A specific cardiomyopathy is formed - “hypothyroid” or “myxedematous heart”.
The following symptoms may appear:
- rare weak pulse;
- pain in the heart area;
- systolic pressure is usually low, while diastolic pressure may remain normal;
- sometimes it is possible to develop concomitant hypertension;
- general swelling;
- weakness, lethargy, sleep apnea;
- X-ray examination reveals an increase in the size of the heart.
The most common type of arrhythmia in hypothyroidism is sinus bradycardia.
The contractile function of the heart suffers, and there is a risk of developing heart failure. Mucous fluid accumulates in the muscle wall and in the heart sac, mucinous edema develops, which also impedes the blood supply to the heart, all this can lead to the appearance of foci of ischemia and an increased risk of heart attack.
Treatment:
- The main treatment is thyroid hormone replacement therapy;
- With concomitant arterial hypertension - antihypertensive drugs, diuretics;
- There are also surgical innovative methods - for example, transplantation of donor thyroid cells.
CONGENITAL PARENCYMATOUS LIPIDOSES
Congenital parenchymal lipidoses are hereditary enzymopathies, inherited in an autosomal recessive manner, and are characterized by the accumulation of lipids in cells that damage cell structures and are often accompanied by the death of the cells themselves. The most common lipid thesaurismoses are:
- Gaucher disease is caused by a lack of the enzyme beta-glucocerebrosidase. As a result, glucocerebrosides accumulate in the liver, spleen, bone marrow, brain, endocrine glands and lymph nodes, which leads to the death of cells in these organs and to progressive dementia, increased weight of the liver, spleen and wasting (cachexia).
- Niemann-Pick disease develops in the absence of the enzyme sphingomyelinase, which breaks down sphingomyelin, which is part of many tissues, but especially nervous tissue. In sick children, it accumulates in the cells of most organs and at the same time there is an increase in the mass of the liver and spleen (hepato- and splenomegaly), a lag in mental development, neurological symptoms, hypotension, and exhaustion appear. Children die at the age of 2-3 years.
CARBOHYDRATE DYSTROPHIES
Carbohydrate dystrophies are associated with the accumulation of protein-polysaccharide complexes (glycogen, glycoproteins) in cells, or with the formation of these substances in those cells where they are not normally present, or with a change in their chemical composition.
Carbohydrates are an essential and most significant component of food. A person consumes 400-600 g of various carbohydrates per day. They are a necessary element of metabolism, an important component of the structure of cells and intercellular substances, and one of the main sources of energy to ensure the vital functions of the body.
ACQUIRED CARBOHYDRATE DYSTROPHIES
Hypoglycemia is a condition characterized by a decrease in blood glucose below 65 mg%, or 3.58 mmol/l. Normally, fasting blood glucose levels range from 65-110 mg%, or 3.58-6.05 mmol/l.
The causes of hypoglucemia are liver diseases - chronic hepatitis, cirrhosis of the liver, fatty degeneration, as well as prolonged fasting.
Disease results:
- impaired transport of glucose from the blood to hepatocytes, a decrease in the level of formation of glycogenesis in them and, in connection with this, the absence of stored glycogen;
- inhibition of the process of glycogen formation and glucose transport from hepatocytes to the blood.
Consequences of hypoglycemia
- Hypoglycemic syndrome is a persistent decrease in blood glucose levels below normal (up to 60-50 mg%, or 3.3-2.5 mmol/l), leading to disruption of the body's vital functions.
- Hypoglycemic coma is a condition characterized by: - a drop in blood glucose concentration below 40-30 mg%, or 2.0-1.5 mmol/l);
- — loss of consciousness;
- - life-threatening disorders of body functions.
Hyperglycemia is a condition characterized by an increase
blood glucose levels are higher than normal (more than 120 mg%, or 6.05 mmol/l on an empty stomach).
Causes of hyperglycemia:
- pathology of the endocrine system, accompanied by an excess of hormones that stimulate the flow of carbohydrates into the blood (glucagon, glucocorticoids, catecholamines, thyroid hormones, growth hormone) or a lack of insulin or a decrease in its effectiveness;
- neuro- and psychogenic disorders, for example reactive psychoses, stress reactions and similar conditions, characterized by activation of the endocrine system;
- overeating, especially long-term excessive consumption of confectionery products;
- liver diseases in which hepatocytes lose the ability to transform glucose into glycogen.
Consequences
- Hyperglycemic syndrome is a condition accompanied by a significant increase in blood glucose levels above normal (up to 190-210 mg%, 10.5-11.5 mmol/l or more), leading to disorders of the body's vital functions.
- Hyperglycemic coma , characterized by loss of consciousness, decreased or loss of reflexes, respiratory and circulatory disorders, often ending in the death of the patient.
Most often, hyperglycemia is observed in diabetes mellitus, which develops as a result of absolute or relative insulin deficiency (see Chapter 19).
Myocardial dystrophy
Myocardial dystrophy is a non-inflammatory damage to the heart muscle caused by metabolic disorders in the body.
The causes of the disease can be the following factors:
- Avitaminosis;
- Violation of carbohydrate, protein, fat metabolism (with liver failure, uremia, diabetes, etc.);
- Endocrine system disorders (thyrotoxicosis, hypothyroidism, dysfunction of the pituitary gland);
- Disorders of electrolyte metabolism (when the content of potassium and calcium in the body is higher or lower than normal);
- Systemic neuromuscular disorders (myasthenia gravis, myopathy);
- Oxygen starvation (with pulmonary and heart failure);
- Intoxication (poisoning of the body with dangerous substances, including alcohol intoxication, drug overdose, as well as in the case of kidney and liver failure, etc.).
- Infections (acute and chronic);
- Neurogenic effects (stress, sympathicotomy).
- Anemia;
- Physical overexertion.
Myocardial dystrophy does not have clear symptoms, since it is a concomitant diagnosis, and the patient’s well-being is largely determined by the course of the underlying disease. The patient's complaints boil down to unpleasant sensations, dull pain in the heart area, shortness of breath, palpitations, and fatigue. With this disease, the ability of the heart muscle to contract is impaired, which causes mild and, much less frequently, moderate forms of heart failure. Cardiologists distinguish three stages of development of myocardial dystrophy:
- Neurofunctional (when there is no deviation from the norm yet, but metabolic tension already exists);
- Metabolic-structural or organic changes (there are already signs of changes in the myocardium);
- Stage of heart failure (pronounced changes in the structure and functions of the heart muscle).
It is believed that myocardial dystrophy is reversible. Treatment of this disease is aimed at influencing metabolic processes, conduction disorders, and heart failure.
Thus, medications that affect electrolyte metabolism are widely used. These are mainly potassium salts, magnesium and phosphorylated vitamins B and B6.
A popular remedy is anabolic hormones, which have shown their effectiveness in disorders of protein metabolism and nutrition of the heart muscle. This group of drugs includes methandrostenolone, pyridine (orotatkaly) and purine (riboxin, inosid) mononucleotides, ATP and AMP.
An important role in the treatment of myocardial dystrophy is played by systematic visits to sanatoriums specializing in the treatment of cardiovascular diseases. Mineral waters, rich in potassium, calcium and magnesium and other essential substances, will replenish the biochemical imbalance in the body and restore electrolyte metabolism.