Behçet's disease - symptoms and treatment
The main symptom of Behçet's disease is painful mouth ulcers . Most often, ulcers appear on the mucous membrane of the lips, gums, cheeks and tongue. As a rule, they are small (less than 1 cm in diameter), have a multiple nature (from 3 to 10 at a time), are prone to recurrence and heal within 1-3 weeks. This symptom occurs in almost 100% of patients.
painful sores in the genital area is also typical . In women, the labia are more often affected, in men - the scrotum. After healing, small scars may remain. Approximately 5% of men develop epididymitis (non-infectious inflammation of the epididymis), which can lead to infertility.
Skin lesions can be varied and include nodules, acne-like rashes (resembling acne vulgaris), pyoderma (pustular rashes), etc.
Increased skin sensitivity (pathergy) is typical The diagnostic test for pathergy is based on this feature: superficial damage to the skin with the tip of a needle leads to the formation of a focus of redness and inflammation.
Eye damage is most common in young men. It manifests itself as an accumulation of inflammatory cells in the anterior chamber of the eye (hypopyon), or occurs in the form of chronic recurrent panuveitis (inflammation of all parts of the choroid and damage to the vitreous body). It is also possible to damage the anterior parts of the eye (anterior uveitis or iridocyclitis), the posterior parts (posterior uveitis or chorioretinitis). Pseudotumor of the orbit is rare.
In approximately half of the patients, joint damage in the form of non-deforming arthropathy with predominant involvement of the knee, ankle, wrist and elbow joints. Inflammatory fluid may accumulate in the joints (exudative synovitis develops). As a result, the patient experiences pain and stiffness in the joint.
Sometimes heart damage in the form of myocarditis, pericarditis, and inflammation of the coronary arteries. Signs of cardiac involvement may include chest pain, shortness of breath during exercise (less often at rest), and interruptions in cardiac function.
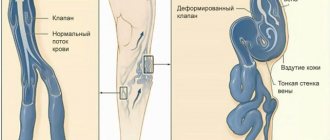
One of the main manifestations of Behçet's disease is damage to the veins . About a quarter of patients develop thrombophlebitis. But the movement of blood clots from the affected vessels and their entry, for example, into the lungs (which can lead to the death of the patient) practically does not occur with this disease. This is due to the fact that the thrombus is attached throughout the entire venous wall and does not have a movable “tail”. Thrombosis of the cava, hepatic and portal veins is life-threatening.
Damage to the arteries is accompanied by thinning and bulging of the wall - the formation of aneurysms. Rupture of aneurysms can be fatal to the patient.
Severe damage to the central nervous system It is possible to develop non-infectious meningitis (symptoms: headache, stiff neck), encephalitis (its manifestations are fever, impaired consciousness, convulsions), damage to the medulla oblongata. In women, benign angiopathy (vascular damage) of the central nervous system is possible, manifested by severe headaches.
Mental manifestations include anxiety and depressive disorders, memory and attention disorders.
The main manifestations of damage to the gastrointestinal tract : ulceration of the mucous membrane of the ileum and cecum. Patients may experience abdominal pain, accumulation of gases, and both constipation and diarrhea may occur. Among residents of the Far East, the incidence of gastrointestinal tract damage is higher than in Mediterranean countries. This may be due to a higher frequency of detection of the HLA-B51 antigen in them.
Kidney damage in the form of glomerulonephritis (autoimmune inflammation of the glomerular apparatus of the kidneys) is rare. But when amyloidosis occurs (the formation and deposition of a specific amyloid protein complex as a result of autoimmune inflammation) with high proteinuria (the release of large amounts of protein in the urine), severe renal failure quickly develops.
Lung involvement is very rare, manifests as hemoptysis due to rupture of vascular aneurysms, and can be fatal [1][2][3][4][5][6][7].
Behçet's syndrome
Clinical picture Behcet's syndrome is, in a nosological sense, a purely clinical concept. Not only relatively specific, but even any characteristic histomorphological, immunological or biochemical signs of this disease do not exist. At the same time, the clinical picture, if fully expressed, makes the diagnosis of the disease indisputable. It should be borne in mind that specific symptoms of Behcet's syndrome may not appear simultaneously. Months and even years may pass between the appearance of the first signs of the disease and the addition of new clinical manifestations. By this time, the first signs may undergo a complete reverse development. Therefore, at any given period, a patient with Behçet's syndrome may have only one or several characteristic signs of the disease, not to mention the possibility of remission without any pathological symptoms. This circumstance gives particular importance to anamnestic data for the correct recognition of the disease.
The most characteristic clinical manifestations of Behcet's syndrome are described below .
Aphthous (ulcerative) stomatitis. Shallow painful ulcers on the oral mucosa are usually the first symptom of the disease and occur in almost all patients. These ulcers (diameter from 2 to 10 mm) are located in the form of single elements or clusters. They are localized on the mucous membrane of the cheeks, gums, tongue, lips, sometimes in the pharyngeal region, less often in the larynx and on the nasal mucosa. In the central part they have a yellowish necrotic base, surrounded by a red ring, externally and histologically no different from ulcers with banal aphthous stomatitis. The ulcers last for several days to several weeks (usually 3 to 30 days) and heal without scarring.
Ulcers of the genital organs. Multiple or single recurrent painful genital ulcers look very similar to oral ulcers. They occur in approximately 80% of patients with Behçet's syndrome and are localized in women on the labia, vulva and vaginal mucosa, and in men on the scrotum and rarely on the penis. Both women and men can have perineal skin lesions. Ulcers of the vaginal mucosa are often painless and in such cases they are discovered either in connection with complaints of discharge or during a gynecological examination for other reasons. In most patients, recurrence of genital ulcers is observed less frequently than oral ulcers; The course and healing time do not differ.
Rarely, ulcers of the bladder mucosa or symptoms of cystitis without signs of ulceration are observed.
Eye damage. The most serious and common eye injury is uveitis, occurring in 2/3 of patients. As a rule, it is bilateral and very rarely occurs at the very beginning of the disease. On average, about six years pass between the first manifestations of the disease (usually ulcerative lesions of the oral mucosa and genital organs) and the onset of uveitis. A patient with Behçet's syndrome or suspected of having this disease should be consulted by an ophthalmologist to examine the anterior chamber of the eye by biomicroscopy and the posterior segment by biomicroscopic and indirect ophthalmoscopy. Fundus photographs following intravenous fluoroscein administration often reveal diffuse disc and retinal staining, indicating significantly increased vascular permeability.
Precipitates in the cornea and cellular infiltrates in the vitreous definitely indicate uveitis activity.
It is now obvious that the main cause of blindness in Behçet's syndrome is posterior uveitis involving the vitreous body and retina. Blindness can also be caused by anterior uveitis with the development of hypopyon (i.e., accumulation of pus in the anterior chamber of the eye). However, hypopyon is currently rare in patients with Behçet's syndrome, which is associated with local or systemic use of corticosteroids.
Other ocular pathologies associated with this disease include conjunctivitis , corneal ulceration, and less commonly observed optic neuritis, chorioretinitis, retinal vasculitis, and fundus arterial or venous thrombosis. Eye damage in some cases is completely reversible, but some patients develop persistent severe changes, in particular, in addition to partial or complete loss of vision, glaucoma and cataracts may occur.
Joint damage. Arthritis develops in approximately 50% of patients with Behçet's syndrome at any time during the course of the disease. They are usually combined with other manifestations of the disease, quite often with erythema nodosum. As a rule, there is a symmetrical polyarthritis affecting large joints (usually the knee, ankle, elbow). Less common is monoarthritis of a large joint or involvement of small joints in the process. Usually the joints are affected by the type of acute, often recurrent synovitis with complete reverse development. When analyzing synovial fluid, from 5,000 to 20,000 leukocytes per 1 mm3 are detected, with a predominance of neutrophils. The chronic course of arthritis is very rare (in this case, the synovial fluid may contain only a few mononuclear leukocytes), and even minimal signs of joint destruction are an exception (including with frequent recurrence of arthritis over many years). Arthralgias without objective signs of joint inflammation are very common, but have no diagnostic value.
In isolated patients who are carriers of HLA-B27, the development of sacroiliitis and spondyloarthritis has been described.
Skin changes are characteristic of approximately 70% of patients with Behçet's syndrome and are considered as diverse manifestations of cutaneous vasculitis. These include erythematous papules, pustules, blisters and elements such as erythema nodosum. The latter may be no different from “ordinary” erythema nodosum, but in some cases they show some features. Thus, the nodes are sometimes located in clusters, localized on the arms, and in some patients they even ulcerate. In some patients, elements of necrosis and suppuration of the skin are expressed, reaching significant distribution - the so-called gangrenous pyoderma.
Almost pathognomonic for Behçet's syndrome, although it does not occur in all patients, is the formation of a small pustule or nodule (sometimes with a pink halo) one day after any injection at the site of needle insertion. This feature can also be used for diagnostic purposes - after the administration of an isotonic sodium chloride solution or even an injection with a dry needle, a sterile pustule sometimes appears.
Vascular damage. In addition to the manifestations of cutaneous vasculitis discussed above, thrombophlebitis of the superficial or deep veins often develops. More often it is localized on the legs and sometimes causes pulmonary embolism. Thrombosis of the superior or inferior vena cava is very rarely observed. Sometimes phlebitis develops immediately after venipuncture.
Involvement of arteries in the pathological process is rare and is manifested by thrombosis and the formation of aneurysms. These changes were found in the aorta, ulnar, femoral and popliteal arteries, and fundus vessels. Thrombosis of branches of the pulmonary artery has also been described. Thrombosis of the arteries of the legs can lead to gangrene of the feet.
Neurological pathology. Involvement of the nervous system in the process is not uncommon - in severe forms of the disease in almost 1/4 of patients. The main neurological pathology in Behcet's syndrome is meningoencephalitis, which usually does not occur in the early stages of the disease and is manifested by fever, severe headache, and stiff neck. The cerebrospinal fluid is sterile and characterized by lymphocytosis and a normal content of gamma globulins. Meningoencephalitis, which can occur with exacerbations and remissions, makes the prognosis of the disease much more serious. Less common are other variants of damage to the nervous system - brainstem and spinal disorders, corticospinal conduction disorders, reversible increase in intracranial pressure with papilledema, transient pathology of the cranial nerves. Peripheral neuropathies are rare. In some patients, hemiparesis, tetraplegia, and “benign” increased intracranial pressure have been described. Psychosis is very rare.
Damage to the digestive tract. A number of patients with Behcet's syndrome are characterized by diarrhea, nausea, symptoms of proctitis, and perianal ulcers. Sometimes intestinal lesions are indistinguishable from ulcerative colitis and Crohn's disease. Some authors emphasize the pathogenetic similarity of these diseases and indicate that with primary Crohn's disease all the signs of Behçet's syndrome can occur. In some patients with a combination of signs of Behçet's syndrome and Crohn's disease, resection of the affected part of the colon also led to a noticeable reduction in the symptoms of Behçet's syndrome. Duodenal ulcers were found in isolated patients. Gastrointestinal manifestations are especially common in the Japanese (50% of all patients).
Other manifestations of the disease. Among the rarer symptoms of Behçet's syndrome, one should point out the possibility of involvement of the lungs with their diffuse infiltration, hemoptysis and pleurisy (almost exclusively in the Turkish population). Heart damage is also known (especially in severe generalized forms of the disease): myocarditis, pericarditis, endocarditis with the formation of moderately severe valve defects. A small proportion of patients have epididymitis and amenorrhea. Rarities include reports of pancreatitis, cryoproteinemia, and mild nephritis. There are isolated descriptions of hypercoagulability syndrome accompanied by reduced fibrinolysis.
An uncommon complication of Behçet's syndrome is systemic secondary amyloidosis, especially among people in the Middle East.
Some authors have drawn attention to the presumably non-random combinations of Behcet's syndrome with lymphoblastic lymphoma and with concomitant infection (in particular, subungual), which may indirectly indicate immune disorders inherent in the disease.
Flow. The course of Behcet's syndrome is highly variable. During different periods of the disease, the number of clinical symptoms and their severity are different. The disease is characterized by relapses and periods of subsidence of activity. With almost every exacerbation, there is an increase in body temperature and aphthous stomatitis, very often in combination with skin changes. Remissions last from several weeks to several years, which largely determines the overall severity of the disease and the patient’s ability to work.
In some patients, Behcet's syndrome is mild and does not significantly affect their lives. On the other hand, in some cases the disease is very severe, with high fever, obvious intoxication, polysystemic lesions and the absence of complete remissions. The causes of death are meningoencephalitis and vascular lesions of the central nervous system (most often), arterial thrombosis of various locations, embolism due to thrombophlebitis, perforation of ulcers of the digestive tract. The development of such signs significantly worsens the prognosis of the disease.
Severe uveitis that does not affect life expectancy may nevertheless indicate a dire prognosis due to the threat of vision loss.
1.General information
Behcet's syndrome is a rare and not yet sufficiently studied disease, which is classified as a group of systemic vasculitis (vascular inflammation). Small and medium-sized arteries are predominantly affected, which, in turn, causes the development of a specific clinical picture (see below).
A number of etiopathogenetic, classification, diagnostic and other issues regarding Behçet's syndrome remain controversial, despite the gradual accumulation of statistical data and research results. Thus, assessments of the influence of the gender factor are contradictory (some sources report a predominance of people of one gender or another among the sick, other authors deny such trends), while a certain regional dependence cannot be explained (indigenous residents of the Mediterranean, Near and Far East get sick hundreds of times more often than residents of, say, North America), opinions differ regarding trigger and etiopathogenetic mechanisms, criteria for differential diagnosis, approaches to treatment, etc.
A must read! Help with treatment and hospitalization!
3. Symptoms and diagnosis
The clinical picture of Behcet's syndrome is nonspecific, very polymorphic and very variable both in severity and types of course. Previously, a typical triad was considered to be a combination of ulcerative stomatitis, ulcerative inflammation of the genitals and inflammation of the ocular structures (uveitis, iridocyclitis, conjunctivitis). However, today a wide range of symptoms have been identified that are equally or even more characteristic of Behcet's syndrome, namely:
- joint inflammation (arthritis);
- skin lesions characteristic of vasculitis in general (papules, pustules, erythema, etc.);
- thrombophlebitis;
- damage to the central nervous system;
- pathology of the gastrointestinal tract;
- reproductive system disorders;
- in rare cases - pulmonary, cardiac, renal pathology, oncological processes.
All of these symptoms and complications are non-pathognomonic (i.e., they may indicate any of a variety of other diseases); in addition, they may not appear all at once, but sequentially, one after another, in certain combinations - sometimes over many years. And yet, based on the recognizable combination of the following manifestations, the nature of the clinical picture and the transformation of the symptom complex, Behcet's syndrome can (and therefore should) be diagnosed at least at the level of the dominant assumption.
The situation is further complicated by the fact that with Behcet's syndrome there are not only clinical, but also laboratory indicators that (or certain combinations of which) would become a decisive and unambiguous confirmation of the diagnosis.
About our clinic Chistye Prudy metro station Medintercom page!
Behçet's disease
What is Behçet's disease (BD)?
This is a systemic vasculitis, which affects vessels of any type and caliber.
The cause of BD is unknown; the most discussed hypothesis is genetic predisposition. This hypothesis is supported by: geographical prevalence, familial aggregation, association with the HLA-B51 antigen.
It is diagnosed more often in men aged 20-40 years.
There are no specific laboratory markers for BD; HLA-B51 testing is recommended.
Symptoms
The diagnosis is made only on the basis of clinical symptoms:
- recurrent aphthous stomatitis;
- ulcers on the genitals;
- eye pathology (posterior uveitis, retinal vasculitis);
- skin lesions (erythema nodosum, pseudofolliculitis, acne-like rash);
- positive pathergy test (skin rashes that appear after 24-48 hours at the site of an injection with a sterile needle);
- organ pathology: damage to blood vessels, the central nervous system and the gastrointestinal tract.
Diagnostics
Clinical modern methods are used to assess the manifestations of the disease: the diagnosis is established on the basis of generally accepted criteria for the disease, determining activity and severity indices.
Treatment
Standard treatment methods are used based on international and domestic clinical recommendations, including the complex use of immunosuppressive and vascular drugs registered in Russia, as well as innovative therapy within the framework permitted by a special commission and ethical committee.
The Institute’s experience in treating this pathology
In 1958, the Institute of Rheumatism was organized, where a department of “borderline forms” was opened; from that time on, the study of Systemic scleroderma (SSc) and Systemic lupus erythematosus (SLE) began. In 1981, two laboratories were created from this department: systemic rheumatological diseases and the laboratory of microcirculation and inflammation, which, maintaining continuity, are still engaged in the study and treatment of severe systemic rheumatological diseases and, subsequently, comorbid conditions in patients with rheumatic diseases (RD) : since 1985, the study of antiphospholipid syndrome, since 1990, the problems of pregnancy with RD, since 2004, cardiovascular problems, since 2006, mental disorders and psychological characteristics in our patients, since 2012, the study of metabolic syndrome, and since 2014 endocrine diseases in RA (diabetes and autoimmune thyroid diseases).
Make an appointment with a specialist:
- by phone, +7
- by filling out the feedback form
- receive ]in absentia[/anchor]
Publications in the media
Behçet's disease (Behçet's syndrome, Touraine's major aphthosis) is a systemic chronic disease of unknown etiology with a relapsing course, manifested by a characteristic triad: recurrent aphthous stomatitis, ulcerative changes in the mucous membrane and skin of the genital organs, eye damage in the form of uveitis or iridocyclitis. Additionally, damage to other organs is possible - arthritis, thrombophlebitis, colitis, and neurological symptoms often occur. Statistical data. The disease is common in Japan and Mediterranean countries (including Turkey). Prevalence in the USA is 1:100,000, in Russia - 3:100,000, in Japan - 670:100,000. The predominant age is 30–40 years. The predominant gender is male (2:1).
Genetic aspects. Several cases of familial disease have been described. The disease is listed in the McKusick Catalog of Inherited Diseases (109650). In Japan and Mediterranean countries, the disease is associated with HLA B5 and HLA DR5 Ag.
Risk factors • Consumption of large quantities of walnuts • Belonging to indigenous ethnic groups of the Mediterranean, Japan, Middle East.
Pathomorphology • Mononuclear perivascular infiltration • Swelling of endothelial cells • Partial obliteration of the vascular lumen • Mononuclear infiltration of the synovial membrane • Neutrophilic dermatitis, consistent with the picture of Sweet's syndrome • There may be no morphological changes.
Clinical picture • Oral mucosa: aphthous stomatitis (99%). Ulcers - shallow, painful, last from several days to several weeks, heal without a scar • Genital organs •• men - painful ulcers on the skin of the penis and scrotum •• women - ulcers on the mucous membrane of the vulva and vagina, often painful • Eye lesions: iritis, iridocyclitis, chorioretinitis, hypopyon (accumulation of pus in the anterior chamber of the eye), retinal hemorrhages, disc edema, optic nerve atrophy • Skin manifestations - papulovesicular rash, changes like erythema nodosum, vasculitis, pyoderma. Possible patchy hair loss. The formation of a purulent pustule at the injection site of any drug is very specific • Joint damage •• Morning stiffness occurs in 30% of patients •• Symmetrical polyarthritis of large joints of the lower extremities without signs of destruction • Thrombophlebitis: superficial veins, less often - pulmonary veins, cerebral veins • Neurological symptoms : damage to cranial nerves; symptoms reminiscent of multiple sclerosis, pyramidal insufficiency. In the cerebrospinal fluid - lymphocytosis, normal content of g-globulins • Gastrointestinal tract damage: aphthous-ulcerative changes in the gastrointestinal mucosa, often clinically indistinguishable from those with ulcerative colitis or Crohn's disease • Lung damage: thrombosis or PE, less often - pulmonary infiltrates, pleurisy • Rarely Myopathy or myositis, gangrene, epididymitis, glomerulonephritis, and schizoaffective disorders occur.
Laboratory data • Increased ESR (not always) • Detection of immune complexes, cryoglobulins in the blood serum • Hypergammaglobulinemia • Complement levels are normal or elevated • Abs to mucosal cells • RF absent • ANATs absent • Abs to cytoplasmic Ag of neutrophils • Demyelinating Abs in nerve damage systems • Antiphospholipid antibodies • The degree of decrease in the level of antithrombin III in the blood plasma correlates with the activity of the process • An increase in fibrinolytic activity of plasma occurs during exacerbation of the disease • In the synovial fluid there are 5000–20,000 leukocytes per 1 μl, neutrophils predominate.
Arteriography to detect aneurysms or thrombosis.
Diagnostic tactics. In Russia, Behcet's disease should be assumed after excluding other causes of ulceration of the mucous membranes.
International Diagnostic Criteria (1990) • Major criterion - recurrent oral ulceration, at least 3 times within 12 months • Minor criteria •• Recurrent genital ulceration •• Eye involvement (anterior uveitis, posterior uveitis, vitreous opacities) •• Skin lesion (resembling erythema nodosum or pseudofolliculitis; acne-like nodules in a postpubertal patient not receiving GC) •• Positive pathergy test: erythematous papule with a diameter of more than 2 mm after pricking with a sterile needle under the skin to a depth of 5 mm (assessed after 48 hours) .
To make a diagnosis, 1 major and 2 minor criteria are needed. Note: the criteria can be applied only in the absence of other pathology that could determine their presence.
TREATMENT
General tactics. It is based on immunosuppressive therapy (local for changes in the mucous membranes, systemic for the treatment of extramucosal manifestations). No specific regimen or diet was suggested.
Drug treatment
• For systemic reactions (fever, eye damage, central nervous system) •• Prednisolone 1 mg/kg/day or pulse therapy with methylprednisolone 1 g IV daily for 3 days. For posterior uveitis, if there is no improvement after hormone therapy, cyclosporine 5 mg/kg/day with a gradual increase in dose to 10 mg/kg/day until a therapeutic effect develops (therapeutic concentrations of cyclosporine in blood plasma are 50–200 ng/ml) •• Cytostatic agents (primarily for meningoencephalitis or eye damage) ••• Chlorambucil 0.1–0.2 mg/kg long-term (up to 2 years) ••• Azathioprine 2–3 mg/kg/day ••• Cyclophosphamide 50–100 mg/day in the morning. The patient should be warned about the need to drink at least 8-10 glasses of water during the day and if hematuria occurs, consult a doctor. Medicines should be taken orally due to the ease of formation of post-injection suppurations.
• For thrombophlebitis - acetylsalicylic acid 320 mg/day.
• In case of resistance to treatment, the use of intravenous immunoglobulin at 0.2–2 g/kg/day is recommended for 4–5 days.
Complications • Blindness • Central and peripheral paresis and paralysis • Pulmonary embolism (rare) • Vascular aneurysms • Amyloidosis.
Course and prognosis. The life expectancy of patients with damage to the nervous system is shorter than in the general population. Other manifestations (except for vascular accidents and the development of complications) do not affect life expectancy.
ICD-10 • M35.2 Behcet's disease.
Applications • MAGIC syndrome - a variant of Behçet's syndrome (English M outh A nd G enital Ulcers and Interstitial Chondritis oral ulcers, interstitial chondritis) • Mollare meningitis. More often it occurs in the form of recurrent forms of aseptic meningitis: fever, headache, malaise, meningeal signs, monocytes and endothelial-like cells in the cerebrospinal fluid.
References
- Behçet's disease (BD). Clinical recommendations. 2021
- Shenavandeh S, Jahanshahi KA, Aflaki E, Tavassoli A. Frequency of HLA-B5, HLA-B51 and HLA-B27 in patients with idiopathic uveitis and Behçet's disease: a case-control study. Reumatologia. 2018;56(2):67-72. doi: 10.5114/reum.2018.75516. Epub 2021 May 9. PMID: 29853720; PMCID: PMC5974627.
- Sakly K, Lahmar R, Nefzi F, Hammami S, Harzallah O, Sakly N, Sakly W, Hassine M, Mahjoub S, Ghedira I, Feki S. Phenotypic abnormalities of peripheral blood mononuclear cells in patients with Behçet's disease and association with HLA- B51 expression. Immunol Invest. 2014;43(5):463-78. doi: 10.3109/08820139.2014.886260. Epub 2014 Mar 24. PMID: 24661088.
- Shadmanfar S, Shahram F, Nadji A, Akhlaghi M, Faezi ST, Sadeghi-Abdollahi B, Faridar A, Madanchi N, Davatchi F. The relationship between plasma homocysteine level and HLA-B51 in patients with Behcet's disease: a case-control study . Int J Rheum Dis. 2014 May;17(4):466-70. doi:10.1111/1756-185X.12271. Epub 2014 Jan 16. PMID: 24428874.
2. Reasons
The immediate causes and patterns of development of Behcet's syndrome are one of the most pressing issues. Since the first clinical descriptions and studies (30-40s of the twentieth century), many assumptions and hypotheses have been put forward, the most well-reasoned of which were hereditary, infectious, and autoimmune. However, for example, the viral or bacterial (streptococcal) hypothesis about the nature of this disease is today considered refuted and untenable, although some authors continue to insist on it. Much uncertainty remains regarding the mechanisms of inheritance, triggering factors of immune and biochemical disorders, etc.
Reliable provoking factors include long-term (many years and daily) alcohol consumption, the presence of chronic infectious and inflammatory foci, etc.
The genetic factor is clearly visible in some cases and absent in others.
Visit our Rheumatology page