Drug treatment
Indication for starting medication is blood pressure level:[1]
- in women with chronic uncomplicated hypertension - systolic blood pressure ≥ 150 and/or diastolic blood pressure ≥ 95;
- in all other cases (gestational hypertension, preeclampsia, target organ damage, associated clinical conditions) - systolic blood pressure ≥ 140 and/or diastolic blood pressure ≥ 90 mm Hg.
Important aspects of drug therapy:[1][2][5][8]
- The choice of drug depends on the duration of pregnancy - there are significant restrictions on taking medications in the first trimester, and after childbirth - on the presence or absence of lactation.
- Treatment begins with minimal doses of one drug (usually methyldopa), if necessary, the dose is increased, then another drug is added.
- It is necessary to maintain target blood pressure for 24 hours, so blood pressure should be periodically monitored even when feeling well, in order to adjust therapy in time.
- Hypertension in itself is not a contraindication for vaginal delivery, but drug therapy during labor must be continued.
Antihypertensive therapy for hypertension in pregnant women: methyldopa and β-blockers
Antihypertensive therapy is indicated for increased blood pressure (equal to or higher than 140 and 90 mm Hg) and consists of taking oral medications. Methyldopa 1000 to 3000 mg per day is preferable. If there is a threat of preeclampsia, nifedipine up to 40 mg per day is used, as well as β-blockers (labetalol is most often prescribed, and metoprolol succinate preparations are classified as reserves).
List of prohibited drugs
When planning, during pregnancy and lactation, it is prohibited to take RAAS blockers (renin-angiotensin-aldosterone system) - ACE inhibitors, sartans, direct renin inhibitors.
List of allowed funds
- methyldopa;
- selective β-blockers;
- nifedipine.
Algorithm for providing medical care during the development of an attack of eclampsia
Treatment of gestational arterial hypertension and preeclampsia is carried out in an obstetric hospital, where intravenous administration of magnesium is used to relieve convulsive syndrome, 1% nitroglycerin and other drugs that are prescribed in accordance with the patient’s condition and specific tests.
Treatment of acute severe hypertension in pregnant women
If there is a sharp increase in blood pressure, pregnant women can be given a 10 mg nifedipine tablet (in the absence of tachycardia). In stationary conditions, intravenous, very slow administration of nitroglycerin and magnesium is added.
Evaluation of treatment effectiveness
Blood pressure should not be reduced too quickly. It is necessary to reduce the initial high pressure by no more than 25%.
Rehabilitation
In the postpartum period, blood pressure increases, reaching a maximum on the fifth day, at which time an increase in medication doses may be necessary.
During lactation, depending on the severity of hypertension, three options are possible:
- lactation without taking medications (uncomplicated hypertension with blood pressure < 150/95);
- lactation with low doses of medications (uncomplicated hypertension with blood pressure ≥ 150/95);
- refusal of lactation for the sake of full treatment of hypertension (complicated hypertension).
In the case of eclampsia, treatment and recovery are carried out in the intensive care unit with artificial ventilation of the lungs.
Delivery for preeclampsia and eclampsia
With moderate preeclampsia, hospitalization in an obstetric hospital is indicated, careful monitoring of the condition of the pregnant woman and the fetus, but prolongation of pregnancy is possible. In severe preeclampsia, after the woman’s condition has stabilized, immediate delivery is necessary.
Alternative therapy
The effectiveness and safety of alternative medicine have not been proven by scientific methods, so their use during pregnancy can be dangerous for the health of the woman and child.
Prevention of eclampsia
To detect preeclampsia and prevent eclampsia, patients should be screened for proteinuria (protein in the urine).
Prevention of long-term consequences
For arterial hypertension that persists more than 45 days after birth, the woman should be observed by a general practitioner or cardiologist with a choice of medications depending on whether lactation continues. If breastfeeding is stopped, the first-line drugs are RAAS inhibitors (primarily ACE inhibitors).
Forecast. Prevention
The prognosis depends on the level of blood pressure and the presence of complications. Timely initiation of adequate treatment for hypertension contributes to a favorable prognosis.
The best prevention of hypertension is a healthy lifestyle and diet, as well as the elimination of existing risk factors (obesity, inactivity, smoking, chronic stress).[6] In case of existing hypertension, in order to prevent complications, the following recommendations are added to these recommendations:
- women with hypertension before pregnancy need to undergo a full examination before planning pregnancy with treatment adjustment if necessary;[1][5]
- women with hypertension during pregnancy need careful monitoring of their condition and strict adherence to medical prescriptions.[1][2][5]
For the addition and verification of the material, we thank Elena Karchenova , a cardiologist, therapist, and scientific editor of the ProBolesni portal.
Hypertension during pregnancy
The initial link in the development of essential hypertension is a violation of the dynamic balance between the pressor and depressor systems of corticovisceral regulation, which maintain the normal tone of the vascular walls. An increase in the activity of the pressor sympathetic-adrenal and renin-angiotensin-aldosterone systems has a vasoconstrictor effect, which causes compensatory activation of the depressor system - increased secretion of vasodilator prostaglandins and components of the kallikrein-kinin protein complex. As a result of depletion of depressant agents, blood pressure lability increases with a tendency to its persistent increase.
Primary disturbances at the cortical level, realized through secondary neuroendocrine mechanisms, lead to the occurrence of vasomotor disorders - tonic contraction of the arteries, which is manifested by an increase in pressure and causes tissue ischemia. At the same time, under the influence of the sympathoadrenal system, cardiac output increases. To improve blood supply to organs, the volume of circulating blood increases compensatoryly, which is accompanied by a further increase in blood pressure. At the level of arterioles, peripheral vascular resistance increases, the ratio between electrolytes in their walls is disrupted, and smooth muscle fibers become more sensitive to humoral pressor agents.
Through the swollen, thickened, and then sclerotic wall of blood vessels, nutrients and oxygen penetrate worse into the parenchyma of internal organs, as a result of which various multiple organ disorders develop. To overcome high peripheral resistance, the heart hypertrophies, which leads to a further increase in systolic pressure. Subsequent depletion of myocardial resources contributes to cardiodilation and the development of heart failure. With symptomatic hypertension, the triggering moments of the disease may be different, but subsequently the same mechanisms of pathogenesis are activated.
Additional pathogenetic factors of hypertension during gestation in hereditarily predisposed women may be insufficient synthesis of 17-hydroxyprogesterone by placental tissue, high vascular sensitivity to the action of angiotensins, increased production of renin, angiotensin II, vasopressin against the background of functional renal ischemia, endothelial dysfunction. A certain role is played by overstrain of corticovisceral regulatory systems due to hormonal changes in the body and emotional experiences caused by pregnancy.
Frequently asked questions about blood pressure control during pregnancy
- What is preeclampsia?
- What are the symptoms of preeclampsia?
- At what stage of pregnancy does preeclampsia usually occur?
- Who is most at risk for preeclampsia?
- If my blood pressure is high, does it mean I have preeclampsia?
- Why is blood pressure control so important during pregnancy?
- What level of blood pressure during pregnancy is considered normal and what is considered high?
- What blood pressure levels before and after pregnancy are considered normal?
- How dangerous is preeclampsia for my baby and for me?
- How is preeclampsia treated?
- Can preeclampsia be prevented?
- Are there long-term effects of preeclampsia?
- Useful links on preeclampsia..
What is preeclampsia? Preeclampsia is a problem that some women face during pregnancy.
It occurs in the second half of pregnancy. The signs of this disease are as follows: high blood pressure, persistent swelling of the lower extremities and the presence of protein in the urine. What are the symptoms of preeclampsia? A woman with mild preeclampsia may feel very well. Therefore, it is necessary to undergo prenatal checkup for early detection of this condition. Symptoms of severe preeclampsia, which develops in the last weeks of pregnancy, include high blood pressure, headaches, blurred vision, intolerance to bright light, nausea, vomiting and excessive swelling of the feet and hands.
At what stage of pregnancy does preeclampsia usually occur? Preeclampsia can occur at any time during pregnancy, during labor, and during the six weeks postpartum period, but it most often occurs in the last trimester and resolves within 48 hours of delivery. Preeclampsia can develop gradually or appear suddenly, although signs and symptoms may already be present but go undetected for several months.
Who is most at risk for preeclampsia? Preeclampsia is much more likely to develop during the first pregnancy and in women whose mothers or sisters also suffered from preeclampsia. The risk of preeclampsia is higher in multiple pregnancies, during teenage pregnancies, and in women over 40 years of age. Other risk categories include women who had high blood pressure or kidney disease before pregnancy and women with a body mass index above 35. The cause of preeclampsia is unknown.
If my blood pressure is high, does it mean I have preeclampsia? Not necessary. If you have high blood pressure, you should see a doctor because this condition may indicate preeclampsia. In addition to high blood pressure, women with preeclampsia experience increased swelling and protein in the urine. Many women have high blood pressure during pregnancy, however, in the absence of swelling and protein in the urine, we are not talking about preeclampsia. If you have high blood pressure, then it is very important for you to monitor your blood pressure levels on a daily basis.
Why is blood pressure control so important during pregnancy? Preeclampsia manifests itself as high blood pressure. Therefore, it is necessary to measure blood pressure at least 2 times a day - morning and evening. It is necessary to measure in a sitting position, after rest and in a calm environment.
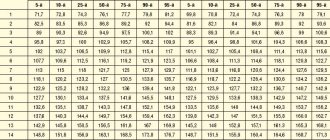
What level of blood pressure during pregnancy is considered normal and what is considered high? To answer this question, use the following table, which shows data on blood pressure values during pregnancy (in mmHg):
| Range | Systolic | Diastolic | What is recommended to do |
| Normal blood pressure | less than 140 | less than 90 | Self-control |
| Hypertension | higher than 140 | higher than 90 | Consult a doctor |
| Severe hypertension | higher than 180 | higher than 100 | Urgent medical attention required! |
Reference: Prof. A.H. Shennan, St. Thomas Hospital, London
What blood pressure levels before and after pregnancy are considered normal? Table of classification of blood pressure levels (in mmHg). Data from the World Health Organization (WHO).
| Range | Systolic | Diastolic | What is recommended to do |
| Pressure is low | < 100 | < 60 | Consult your doctor |
| Optimal pressure | 100 — 120 | 60 — 80 | Self-control |
| Normal blood pressure | 120 — 130 | 80 — 85 | Self-control |
| Slightly elevated blood pressure | 130 — 140 | 85 — 90 | Consult your doctor |
| High pressure | 140 — 160 | 90 — 100 | Consult a doctor |
| Pressure is excessively high | 160 — 180 | 100 — 110 | Consult a doctor |
| The pressure is dangerously high | > 180 | > 110 | Urgent medical attention required! |
How dangerous is preeclampsia for my baby and for me? Preeclampsia prevents the placenta from receiving the amount of blood it needs. If the placenta does not receive enough blood, the fetus suffers from air and nutritional deficiencies, which results in low birth weight and other problems for the baby. Most women with preeclampsia give birth to healthy babies. A small number develop a condition called eclampsia, which is very dangerous for mother and baby. Thanks to well-established antenatal care services, preeclampsia is detected at an early stage, when most problems can be eliminated.
How is preeclampsia treated? The only treatment is the birth of a child. If preeclampsia is diagnosed, mother and baby are closely monitored. It is mandatory to monitor the pressure level, at which measurements are taken 2 times a day. It is necessary to analyze the level of protein in the urine and monitor weight changes. There are now medications and various treatments available that prolong pregnancy and increase the baby's chances of survival.
Can preeclampsia be prevented? Preeclampsia is not a disease that can be prevented by lifestyle changes, such as diet, quitting smoking, quitting alcohol, exercise, getting enough rest, not worrying, etc. There is evidence that calcium supplements reduce the risk of preeclampsia, especially in women living in areas where calcium is deficient in foods. Calcium helps blood vessels relax and thus prevent hypertension.
Are there long-term effects of preeclampsia? For most women, childbirth reverses the effects of preeclampsia. Women who have preeclampsia during pregnancy may later develop high blood pressure. But this may also be a consequence of genetic predisposition, and not preeclampsia itself. In infants, the effects occur if they experienced severe lack of nutrition and oxygen in the womb or had problems as a result of prematurity. There are no health problems associated with preeclampsia in children born to mothers with preeclampsia.
Useful links on preeclampsia
| Organization | Link |
| Preeclampisia foundation | www.preeclampsia.org |
| American Academy of Family Physicians | https://familydoctor.org |
| DrKoop.com | www.drkoop.com/encyclopedia/93/16.html |
| Emedicine (for professionals) | www.emedicine.com/emerg/topic480.htm |
| Preeclampsia Society UK | www.dawnjames.clara.net |
| Action on Preeclampsia (UK based charity) | www.apec.org.uk |
| Australian Action on Preeclampsia | www.aapec.com/index.php |
| Pre-eclampsia experiences and discussion / support group | www.pre-eclampsia.co.uk |
| International Society for the study of Hypertension in Pregnancy | https://www.ncl.ac.uk |
| Mayo Clinic | www.mayoclinic.org |
How to measure blood pressure during pregnancy
The blood pressure measurement procedure takes only a few minutes, but can help prevent very serious health problems. Modern automatic blood pressure monitors do almost everything themselves; you need to use them regularly and follow some rules:
- Take measurements at the same time of day so that the indicators do not change under the influence of hormonal fluctuations and biological rhythms of the body;
- Do not measure blood pressure immediately after exercise, including walking - in this state the pressure may temporarily increase, there is nothing to worry about;
- Do not take measurements less than an hour after eating - due to the active activity of the digestive system, the blood volume is redistributed, so the result will be biased;
- Measure the pressure in a sitting position, the hand lies on the table top, the muscles are relaxed;
- Do not move or talk during the measurement.
You should not measure your blood pressure in a state of strong excitement. First you need to calm down, lie down for a few minutes. Repeated measurement is carried out no earlier than after 10 minutes, if necessary.
What is considered normal
Doctors do not always perceive normal blood pressure in pregnant women as the usual 120/80, since changes in hormonal levels directly affect a woman’s well-being and physiological indicators. Until about the twentieth week of gestation, the pressure level is often reduced. This is due to the active production of the hormone progesterone.
This substance controls the tone of the uterus and relaxes muscle tissue to prevent premature birth. For this reason, even a pressure of 100 over 60 is considered normal if the expectant mother feels well. Measuring blood pressure is a standard procedure that is performed on pregnant women at every appointment with a gynecologist, starting from the 12th week.
The tonometer readings that the doctor receives indicate the general condition of the body, in particular, the functioning of the cardiovascular system. If blood pressure is within the normal range, and the woman does not complain about her health, the gynecologist has no reason to perceive even the numbers 130/90 as a pathology.
Below is a visual table showing the permissible pressure limits for women carrying a child. It is advisable to take measurements daily, especially if before conception the expectant mother had problems with the heart and blood vessels.
| Systolic reading (mmHg) | Diastolic reading (mmHg) | |
| Optimal pressure level | Up to 120 | Up to 70 |
| Normal pressure | Below 130 | Below 80 |
| Blood pressure is higher than normal | 130–139 | 80–90 |
| Not expressed arterial hypertension | 140–159 | 90–100 |
| Moderate arterial hypertension | 160–179 | 100–110 |
| Severe arterial hypertension | More than 180 | More than 110 |
Normal blood pressure is different for each person, with which he feels comfortable, works and performs household duties. As for pregnant women, their normal range varies quite widely and this is not considered a pathology. Features of tonometer indicators in expectant mothers:
Psychosomatics of high blood pressure
- pressure may increase in the third trimester, since after 13–14 weeks of gestation the load on the circulatory system doubles;
- An increase in tonometer readings can be observed under stress, fear of future childbirth, lack of awareness about the upcoming process, etc. In this case, the adrenal cortex produces an excessive amount of stress hormones;
- in the early stages of pregnancy, the pressure drops 5–10 units below normal due to the activity of the hormone progesterone, and in the second or third trimester it increases.
It is difficult to single out specific numbers that a tonometer should show in a pregnant woman - they are individual for each expectant mother. If the indicators go beyond the acceptable limits in one direction or another, the number of measurements needs to be increased. And if dangerous symptoms occur, immediately consult your doctor.