High diastolic pressure usually indicates pathology associated with peripheral vessels. Why can it increase in a person without an increase or with a slight increase in systolic, and what to do in such a situation? Let's try to figure it out.
Increased lower diastolic pressure may be a sign of kidney disease
Forms of the disease
Physiological
One of the normal options. The disease can develop due to excessive physical activity or when moving to a high mountain region (low blood pressure is observed during the adaptation period).
Pathological
- Primary. It can be reversible or over time take a chronic form, that is, turn into a hypotensive disease, accompanied by dizziness, headaches, etc. It occurs against the background of puberty, stress, overwork, thinness, heredity, etc. Source: K.M. Dzilikhova, M.G. Dzgoeva, Z.D. Kaloeva, S.Ch. Khestanova, A.K. Shavlokhova Primary arterial hypertension in children // Pediatrics, 2010, v. 89, no. 3, pp. 116-122
- Secondary. It manifests itself due to cardiovascular disorders, pathologies of the endocrine system, diseases of the kidneys and adrenal glands, pneumonia, diabetes mellitus, etc. The second reason is certain drugs, after discontinuation of which arterial hypotension goes away. Source: N.N. Arkhipova Arterial hypotension in children and adolescents // Practical Medicine, 2008, No. 4(28), pp. 63-65
Blood pressure – systolic and diastolic
Blood pressure (BP) is the force with which blood presses against the walls of the arteries. It is measured in millimeters of mercury (mmHg) and includes two indicators that are written across a line as a fraction. The upper, or systolic, pressure shows the force with which the blood acts on the walls of the blood vessels at the moment of systole, i.e., contraction of the heart muscle, and the lower, or diastolic, shows the force of the peripheral resistance of the vessels at the moment of relaxation of the heart, i.e., diastole.
Normally, in a healthy person, diastolic pressure is in the range of 60–90 mmHg. Art.
Diastolic pressure is often elevated in patients with kidney disease, which is why it is also called “renal pressure,” although in fact it can be caused by other factors, such as atherosclerosis.
The development of arterial hypertension is indicated in cases where three control measurements recorded blood pressure above 140/90 mmHg. Art. More often there is a simultaneous increase in both systolic and diastolic pressure, but sometimes there is an increase in only the lower indicator.
Diagnosis of pathology
The following methods are used to detect arterial hypotension:
- ECG;
- ECHO-KG;
- EEG;
- clinical and biochemical blood tests (indicators of cholesterol, glucose, etc. are important).
The pressure is measured by a specialist three times and a cuff is selected according to age. Therefore, it is highly not recommended to independently diagnose a child and begin self-medication based on the readings of a home blood pressure monitor. Reduced numbers when measured should only be a reason for rechecking with a pediatrician.
During diagnosis, the child may be prescribed 24-hour blood pressure monitoring. This is a very informative study that can identify pathology at an early stage.
Causes of the disease
This disease can develop even in newborns.
If we talk about older children, then number of factors cause arterial hypotension :
- heredity (usually from the mother);
- adolescence (puberty);
- strong psycho-emotional stress, which is typical for schoolchildren;
- stress;
- poor living conditions;
- sedentary lifestyle;
- chronic infections;
- excessive workload at school;
- decreased function of the adrenal glands, thyroid gland, pituitary gland.
What does high blood pressure mean?
The cause of high diastolic pressure is usually diseases of the internal organs (kidneys, thyroid gland, adrenal glands, heart). It often happens that high lower pressure becomes one of the first symptoms of these pathologies. Therefore, if it is elevated, you should definitely undergo a medical examination.
Diastolic pressure is often elevated in patients with kidney disease, which is why it is also called “renal pressure,” although in fact it can be caused by other factors, such as atherosclerosis.
Other causes of increased diastolic pressure may include:
- psycho-emotional disorders (depression, manic psychosis, stress);
- abuse of drinks containing caffeine (strong tea, coffee, cola, energy drinks);
- alcohol abuse.
Another reason for high lower pressure is fluid retention in the body caused by overeating, eating large amounts of salty foods, and smoking.
In pregnant women, increased lower blood pressure is often one of the first symptoms of a dangerous complication of pregnancy - OPG-preeclampsia.
Symptoms of arterial hypotension
For newborns, diagnosis is difficult. Even parents often cannot see problems in behavior, as a result of which they do not draw the attention of the pediatrician observing the child. At this age, the child almost always sleeps, but during periods of wakefulness, a healthy baby will be active and cry. If the child is always calm and rarely cries, then this should alert you. Excessive calm is not typical for a newborn. Source: T.M. Tvorogova, N.A. Korovin Arterial hypotension in children and adolescents // Russian Medical Journal, 2007, No. 21, pp. 1519-1524
At a very early age, children can be susceptible to physical inactivity, which results in decreased muscle tone. The external manifestation is the child’s ability to straighten an arm or leg more than 180 degrees in the joint area. Children with low blood pressure, among other things, lag behind in the development of motor skills and have difficulty sucking and swallowing.
Since the baby cannot complain about feeling unwell, parents must be very attentive!
Older children may present complaints, and they are also characterized by noticeable symptoms :
- if the child abruptly assumes a vertical position, he or she may faint or complain of severe dizziness;
- poor tolerance of stuffy rooms;
- frequent mood swings, short temper, timidity;
- nosebleeds;
- sudden attacks of poor health, accompanied by weakness, nausea, increased heart rate, cold sweat, pallor (this condition is called “vegetative crisis”)
- pain in muscles and joints, in which the child can hardly determine where exactly it hurts;
- decreased performance, fatigue even under light loads, lack of improvement after rest and even sleep;
- pain in the heart area;
- headaches in the area of the crown, back of the head, forehead, most often manifested in the morning;
- feeling of suffocation;
- weather sensitivity.
“SM-Clinic” recommends that if you detect any of the listed symptoms, you and your child should visit a pediatrician as soon as possible. This disease is especially dangerous for newborns, because it can cause abnormal development and lag behind peers. Be sure to consult a doctor and do not self-medicate!
Arterial hypotension may be accompanied by symptoms such as increased gas formation, cramping abdominal pain, impaired bowel function, constipation, and frequent belching.
Why is high diastolic pressure dangerous?
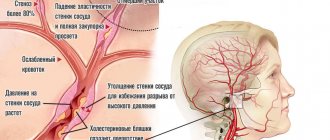
Increased diastolic pressure with normal systolic pressure indicates the presence of some pathology of the vascular system, leading to difficulty in normal blood flow through the vessels.
Normally, in a healthy person, diastolic pressure is in the range of 60–90 mmHg. Art.
If you do not take measures aimed at normalizing blood pressure, then the internal organs and brain do not receive enough nutrients and oxygen. This leads to the development of ischemia and tissue hypoxia, increasing the risk of myocardial infarction and cerebral stroke. An increase in diastolic pressure in older people is especially dangerous, since their blood vessels are significantly altered (atherosclerotic plaques, decreased elasticity of the walls) and the risk of complications of arterial hypertension is higher.
Treatment methods
Therapy may be prescribed with or without medications. For long-term and persistent forms of the disease, a combination of two methods is often used.
Non-drug therapy involves lifestyle adjustments:
- good sleep;
- strict daily routine;
- walks in the air every day for about two hours;
- easy charging after waking up;
- eating small portions 4 to 6 times a day (unlike hypertension, with arterial hypotension there is no need to limit salt intake).
Physiotherapy, water procedures, psychotherapy, medicinal baths can be used.
In some cases, the doctor prescribes a massage course for the child. It can be general or one of the areas: calves, hands, neck-collar area.
If non-drug therapy does not demonstrate effectiveness, drugs are added to the treatment plan. In some cases, according to a specialist, drug treatment begins immediately. It includes a set of medications, their type and dosage are selected strictly individually.
In recent years, interest in the problem of diagnosing and treating arterial hypertension (AH) in individuals with aldosterone hypersecretion has increased. Experimental and clinical studies indicate an unfavorable effect of aldosterone on the development and progression of hypertension, heart failure, and kidney pathology, independent of other factors [1, 2].
From a clinical point of view, the forms of hypertension in which hypersecretion of aldosterone is accompanied by suppression of the renin-angiotensin-aldosterone system (RAAS) deserve special attention - low-renin forms of hyperaldosteronism (LRHA), which are heterogeneous in their etiology, the structure of histomorphological changes in the adrenal cortex, which determines different approaches to their treatment. In the last decade, data have been obtained indicating a high prevalence of primary hyperaldosteronism (from 5 to 15%) among all forms of hypertension [3–6]. However, it is difficult to judge the true prevalence of this heterogeneous pathology, since there is often no information about which forms of NRHA were subject to analysis.
The majority of patients with tumor and non-tumor forms of hyperaldosteronism have severe hypertension [7–9]. In 20% of cases with refractory hypertension, various forms of hyperaldosteronism are diagnosed [10].
For the first time, hypertension caused by hypersecretion of aldosterone by an adenoma of the adrenal cortex was described a little less than six decades ago - in 1955. The syndrome, described by the American surgeon D. Conn under the name “primary aldosteronism,” included hypertension, severe hypokalemia and moderate hypernatremia. Removal of an adenoma with mineralocorticoid activity (aldosteroma) led to normalization of blood pressure (BP) and elimination of electrolyte disturbances, which confirmed the secondary (symptomatic) etiology of this form of hypertension. In most cases, aldosteromas are benign tumors; less commonly (no more than 1% of cases), Conn's syndrome is observed with carcinoma of the adrenal cortex that produces aldosterone. In isolated cases, primary hyperaldosteronism syndrome is associated with extra-adrenal tumor localization.
In some (30–50%) patients with clinical manifestations of Conn's syndrome, diffuse or diffuse nodular hyperplasia of the adrenal cortex is detected, often with bilateral localization. For this pathology, the definition of “idiopathic”, or “pseudo-primary” hyperaldosteronism has been proposed. Surgical treatment (even total adrenalectomy) does not lead to normalization of blood pressure in this category of patients. Among the non-tumor forms of hyperaldosteronism, there is also a primary, predominantly unilateral, form of adrenal hyperplasia. The primary genesis of this form of the disease is substantiated by the remission of hypertension and normalization of aldosterone secretion after unilateral adrenalectomy.
Clinical manifestations of Conn's syndrome also include a rare monogenic form - familial hyperaldosteronism type 1. A characteristic feature of the disease is the normalization of blood pressure and aldosterone secretion during glucocorticoid therapy (this form of the disease is also known as “hyperaldosteronism”, correctable with glucocorticoids). To control blood pressure and aldosterone secretion, a minimum dose of glucocorticoids (dexamethasone or prednisolone) should be used, which has corrective effects [11, 12]. If the hypotensive effect is insufficient, mineralocorticoid receptor antagonists, as well as drugs from other classes of antihypertensive therapy, are used.
In most cases, with all the considered forms of NRHA, severe hypertension is observed, the treatment of which is differentiated depending on the diagnosed form of hyperaldosteronism.
Unilateral adrenalectomy is the optimal treatment method for patients with unilateral aldosteroma or primary adrenal hyperplasia [11]. After removal of the aldosteroma, 50–70% of patients experience normalization or a significant decrease in blood pressure. In almost all cases, the concentration of aldosterone in the blood plasma is normalized, hypokalemia and associated neuromuscular symptoms disappear, and plasma renin activity (PRA) increases. In recent years, preference has been given to endoscopic adrenalectomy. Compared with open adrenalectomy, the use of endoscopic techniques is associated with a decrease in hospitalization duration and faster postoperative rehabilitation [13, 14]. Open adrenalectomy is performed when tumors larger than 5 cm in diameter are detected, when the presence of carcinoma cannot be excluded [15].
In 30–50% of cases, removal of aldosteroma does not lead to a proper reduction in blood pressure, despite the normalization of aldosterone secretion, which is associated with a long history of hypertension, the severity of hypertension before surgery, severe organ damage and a number of other reasons. In this category of patients with residual hypertension, to achieve target blood pressure levels, it is necessary to use antihypertensive drugs from the recommended main and additional classes in the form of mono- or combination therapy, depending on the severity of hypertension, target organ damage and associated clinical conditions [16].
The possibilities of drug correction of hypertension are also considered in cases of primary aldosteronism with an established diagnosis of an adrenal tumor, when patients refuse surgical treatment or when concomitant pathology makes its use unlikely [17, 18]. For this category of patients, as well as for patients with idiopathic aldosteronism, drug therapy should be aimed not only at lowering blood pressure, but also at eliminating the adverse effects of aldosterone: the formation of endothelial dysfunction, the development of cardiovascular complications. First of all, pharmacotherapy includes the use of mineralocorticoid receptor antagonists - spironolactone or eplerenone.
Mineralocorticoid receptor antagonists not only effectively reduce blood pressure, but also provide hypertension-independent organ protection against excess aldosterone [19]. Spironolactone blocks the physiological and pharmacological effects of aldosterone in hyperaldosteronism of any etiology and is used in the preoperative period by patients with aldosteroma to correct hypokalemia, as well as by patients with hyperplastic forms of hyperaldosteronism for whom surgical treatment is not indicated [7, 8, 11, 20, 21].
For primary and idiopathic hyperaldosteronism, spironolactone as monotherapy is taken orally at a dose of 50–400 mg/day in 1–2 doses. According to data presented in the literature, which included 122 observations of patients with idiopathic aldosteronism, the use of spironolactone for 1–96 months helped reduce systolic blood pressure by 25%, and diastolic blood pressure by 22% [22, 23].
According to our data, when treated with spironolactone at a dose of 200 mg/day during the 1st week and at a dose of 250 mg/day during the 2nd week, patients with adrenal aldosteroma observed a significant decrease in systolic and diastolic blood pressure by 24 ± 5/7 ± 2 mmHg Art., and in patients with idiopathic hyperaldosteronism - by 18 ± 4/14 ± 2 mm Hg. Art. [7]. The level of aldosterone in patients with aldosteroma decreased slightly (to a greater extent in the 1st week of treatment), while ARP increased. In patients with idiopathic aldosteronism, the concentration of aldosterone did not change significantly, but in some cases, after 2 weeks of treatment, this indicator exceeded the initial level by 2-3 times. Based on the observed initial decrease in the concentration of aldosterone in the blood plasma (lasting from 4–6 weeks to several months) with its subsequent increase, some authors distinguish two phases of the action of spironolactone on the RAAS [24]. In the first phase, the inhibitory effect of spironolactone on the biosynthesis of aldosterone in cells of the adrenal cortex with tumor or hyperplastic changes is revealed; in the second phase, “escape” from this effect occurs and as the peripheral effect of spironolactone manifests itself under the influence of increased natriuresis and a decrease in intravascular volume, the RAAS is activated.
Currently, it is not recommended to use spironolactone in patients with hypertension against the background of hyperaldosteronism as monotherapy in high doses. Long-term use requires selection of the minimum effective dose – up to 25–50 mg/day. [6, 8]. In all cases, spironolactone therapy is carried out under the supervision of an electrocardiogram (metabolic changes) and the level of potassium in the blood plasma, taking into account possible hyperkalemia. Among the adverse reactions of spironolactone, gynecomastia is noted, and menstrual disorders in premenopausal women are also possible. Gynecomastia treated with spironolactone is a dose-dependent effect. Data are provided on the presence of gynecomastia in 6.9% of patients after 6 months of treatment at a dose of less than 50 mg/day and in 52% of patients when treated at a dose of more than 150 mg/day [25].
Eplerenone is a new selective antagonist of mineralocorticoid receptors, which is currently used in clinical practice among patients with hypertension [26]. Eplerenone binds mineralocorticoid receptors longer and more strongly than aldosterone and blocks them. In this case, an increase in the plasma concentration of aldosterone is observed, especially at the beginning of the use of the drug; subsequently, the secretion of aldosterone by a negative feedback mechanism is suppressed. The affinity of eplerenone for mineralocorticoid receptors is slightly less than that of spironolactone. The advantage of eplerenone is its high selectivity for aldosterone receptors. Eplerenone does not have an anti-androgenic effect, and therefore has fewer adverse endocrine side effects than spironolactone. This drug has antihypertensive efficacy comparable to spironolactone and can be successfully used by patients with idiopathic hyperaldosteronism, especially in cases where the use of spironolactone leads to undesirable endocrine effects [21].
In a prospective randomized study of patients with idiopathic hyperaldosteronism, a comparison of the hypotensive efficacy of spironolactone and eplerenone over 24 weeks of therapy demonstrated the achievement of target blood pressure (less than 140/90 mm Hg) after 16 weeks of treatment in 76.5% of cases on spironolactone therapy and in 82. 4% of cases on eplerenone therapy [27].
Drug therapy for hypertension in patients with NRHA also includes the use of potassium-sparing diuretics - epithelial sodium channel blockers - amiloride, triamterene [28]. The use of amiloride helps reduce blood pressure, normalizes potassium balance, in addition, this drug is devoid of the steroid side effects of spironolactone, but does not have a beneficial effect on endothelial function [29].
The use of diuretics that do not have potassium-sparing properties in patients with NRHA requires caution due to the possibility of worsening hypokalemia against the background of hyperaldosteronemia. At the same time, the refractory course of hypertension and manifestations of heart failure dictate the need to include a diuretic in therapy. In this regard, the loop diuretic torasemide, which increases potassium excretion to a lesser extent than furosemide, has attracted attention, which is explained by its ability to block the effects of aldosterone [30]. Clinical research in this direction seems promising.
Patients with hypertension against the background of various forms of hyperaldosteronism in most cases belong to the category of high cardiovascular risk. This category of patients often experiences severe hypertension. According to our data, in 75% of cases among patients with primary hyperaldosteronism, grade III hypertension is detected, and the syndrome of malignant course of hypertension is detected in 7.8% of cases [31].
To achieve an adequate hypotensive effect in this part of patients, combined, often multicomponent drug therapy is necessary, including, in addition to mineralocorticoid receptor antagonists, drugs from the class of calcium channel blockers (CCBs), angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor antagonists (AT1 subtype).
The effectiveness of the use of CCBs and drugs that block the effects of angiotensin II in patients with low-renin forms of hypertension has been poorly studied to date. Single observations have demonstrated the ability of nicardipine sustained release (SR - Sustained Release) to normalize blood pressure, potassium levels and aldosterone concentrations in the blood plasma of patients with idiopathic aldosteronism [32]. There are a few observations indicating differences in the influence of individual representatives of the CCB class on aldosterone secretion [33, 34]. In recent years, experimental studies have shown that some dihydropyridine CCBs have mineralocorticoid receptor antagonist properties [35]. These properties can be expressed to varying degrees: they are more present in nimodipine and felodipine, and to a lesser extent in amlodipine. Data from Japanese researchers indicate a high potential for antimineralocorticoid activity of the L-, N- and T-type calcium channel blocker benidipine [36]. To confirm the effectiveness of the drugs in question in clinical practice for patients with various forms of hyperaldosteronism, further research is necessary.
ACE inhibitors and AT1-angiotensin receptor antagonists have not found widespread use among patients with hypertension and URGA [37]. There are isolated observations of the effectiveness of blood pressure control in patients with idiopathic hyperaldosteronism, which is explained by the increased sensitivity of adrenal tissue to angiotensin II in this category of patients [38]. The use of drugs of these antihypertensive classes can be recommended when selecting rational combination therapy, especially in refractory hypertension. In case of normokalemia, the combination of these drugs with mineralocorticoid receptor antagonists requires caution (hyperkalemia is possible).
Non-dihydropyridine CCBs (diltiazem and verapamil) do not have mineralocorticoid receptor antagonist properties. Due to the fact that diltiazem and verapamil do not affect the secretion of aldosterone, their use is acceptable to ensure adequate control of blood pressure during the study of the concentration of aldosterone in the blood plasma for diagnostic purposes, when it is necessary to exclude the use of antihypertensive drugs that affect the level of aldosterone concentration in the blood plasma [ eleven].
In recent years, studies have been conducted to explore the possibility of using an aldosterone synthase inhibitor for hyperaldosteronism. Data from experimental studies indicate the organoprotective effectiveness of the drug under study [39]. Large studies of hypertensive patients with hyperaldosteronism in this direction have not yet been carried out. The results of a clinical study of the aldosterone synthase inhibitor LCI699 involving 14 patients with primary aldosteronism are presented, who after 4 weeks of therapy demonstrated a decrease in the concentration of aldosterone in the blood plasma by 70–80% from the initial level, normalization of the level of potassium in the blood plasma, and a moderate decrease in predominantly systolic blood pressure [40] . Despite the short treatment period and the small number of patients, the results obtained in this study are interesting and seem promising in terms of reducing aldosterone secretion in patients with severe hyperaldosteronemia. The possibility of using this drug in clinical practice for NRHA requires further research.
Thus, the tactics of treating patients with hypertension with tumor and non-tumor forms of hyperaldosteronism provides for a differentiated approach, which is based on the correct timely diagnosis of various forms of hyperaldosteronism. Detection of aldosteroma in unilateral (primary) adrenal hyperplasia determines the need for surgical treatment. Timely elimination of the cause of hyperaldosteronism helps to normalize or significantly reduce blood pressure. For idiopathic hyperaldosteronism, pharmacotherapy is indicated, including primarily mineralocorticoid antagonists; for refractory hypertension, the addition of drugs of the CCB class and other antihypertensive classes. For familial hyperaldosteronism type 1, glucocorticoids are used in small doses.
Adequate targeted treatment of hypertension in various forms of hyperaldosteronism is the way to overcome the refractoriness of hypertension and reduce cardiovascular complications against the background of uncontrolled hyperaldosteronemia.
Disease prevention
Nutrition plays one of the most important roles in the prevention of arterial hypotension. It should be frequent (4-6 times a day) and in small portions. You should not eat before bed, with the exception of fresh vegetables. The diet should contain a lot of protein foods (cheese, peas, cottage cheese, lentils and other legumes), little sweets, with the exception of marshmallows, dark chocolate, marshmallows, fruits, dried fruits. If a teenager has arterial hypotension, do not limit him to coffee or black tea. Protect your child from stress and family quarrels, create conditions for him to engage in hobbies, and offer to enroll in a sports section.
Advantages of contacting SM-Clinic
In our clinic you can visit a pediatrician and pediatric cardiologist without queues and at an affordable cost. Some of the best specialists in St. Petersburg work at SM-Clinic; they have modern equipment and diagnostic equipment. The doctor will quickly determine the presence and extent of the disease and prescribe treatment that will return your child to the joy of a healthy and fulfilling life.
Sources:
- N.N. Arkhipova. Arterial hypotension in children and adolescents // Practical Medicine, 2008, No. 4(28), pp. 63-65.
- T.M. Tvorogova, N.A. Korovina. Arterial hypotension in children and adolescents // Russian Medical Journal, 2007, No. 21, pp. 1519-1524.
- K.M. Dzilikhova, M.G. Dzgoeva, Z.D. Kaloeva, S.Ch. Khestanova, A.K. Shavlokhova. Primary arterial hypertension in children // Pediatrics, 2010, v. 89, no. 3, pp. 116-122.
The information in this article is provided for reference purposes and does not replace advice from a qualified professional. Don't self-medicate! At the first signs of illness, you should consult a doctor.
Treatment of high diastolic pressure
How to reduce diastolic pressure with normal systolic pressure, since conventional antihypertensive drugs lower both lower and upper pressure? You don’t need to do this yourself; you need to see a doctor. The main treatment will be to eliminate the primary pathology that led to an increase in lower pressure.
In pregnant women, increased lower blood pressure is often one of the first symptoms of a dangerous complication of pregnancy - OPG-preeclampsia.
To normalize blood pressure, the following groups of drugs can be used:
- Diuretics (diuretics) – stimulate diuresis, remove excess fluid from the body and eliminate swelling.
- Beta blockers - block receptors sensitive to adrenaline, resulting in relaxation of blood vessels and lowering blood pressure. The heart rate also decreases. These drugs are contraindicated in patients suffering from chronic obstructive pulmonary disease (COPD).
- Calcium channel blockers (calcium antagonists). They prevent the flow of calcium ions from the intercellular substance into the muscle cells of blood vessels and the heart. A decrease in Ca2+ concentration in the smooth muscle of blood vessels promotes their dilation and a decrease in blood pressure.
- Angiotensin-converting enzyme inhibitors (ACE inhibitors). They reduce the concentration of angiotensin in the blood, which leads to a decrease in blood pressure.
- Sympatholytics. Normalizes the tone of blood vessels.
- Antispasmodics. Relaxes muscle cells, including those forming the walls of arteries.
Medications for high diastolic blood pressure should be taken in strict accordance with the doctor's prescription. It is unacceptable to independently change the dose of prescribed medications and the schedule for taking them.
Prices
| Name of service (price list incomplete) | Price |
| Appointment (examination, consultation) with a cardiologist, primary, therapeutic and diagnostic, outpatient | 1750 rub. |
| Prescription of treatment regimen (for up to 1 month) | 1800 rub. |
| Consultation (interpretation) with analyzes from third parties | 2250 rub. |
| Consultation with a candidate of medical sciences | 2500 rub. |
| Electrocardiography (ECG) | 1400 rub. |
| Echocardiography (ultrasound of the heart) | 3500 rub. |