Pressure in a general sense is an integral indicator of the state of the cardiovascular system and human health in general.
Adequate numbers, according to specialized research by scientists and practitioners, are in the range from 100 to 140 by 70-90, with minor variations and deviations in both directions.
There is also the concept of an individual norm, which may differ slightly from generally accepted tonometer indicators (no more than 10 mm Hg).
But if the upper pressure is high and the lower pressure is normal or below the adequate limit, so-called isolated systolic arterial hypertension or ISAH for short occurs. We are talking about numbers of more than 140 at less than 90 mmHg.
This condition is much more dangerous than the classic increase in blood pressure, since it carries a greater risk of complications to internal organs that are dangerous to health and even life.
Causes of the primary form of ISAH
The primary form is extremely rare in practice. These are isolated cases, described in the literature; only 10% of clinical situations occur in the primary form of the disease.
As the name suggests, pathology with increased upper pressure (so-called essential hypertension) has a pronounced vascular origin and occurs in three cases:
- Congestive heart failure with the development of cardiac arrhythmias. The more pronounced the condition, the more elevated the upper pressure, while the lower reading remains normal.
- Stroke in the recent past. There is an adaptive mechanism. We can talk about either a temporary decrease in blood pressure due to an emergency condition or isolated hypertension.
Patients with ISAH need to be monitored more carefully; the high probability of relapse does not allow either doctors or the patient to relax.
- Previous heart attack. In the period up to 6 months (early rehabilitation), you need to carefully monitor the patient's health. Repeated cases of ischemia of the heart muscle are possible. Since isolated systolic hypertension often accompanies patients, problems are likely.
Hereditary factors also play a significant role. Most relevant sources directly indicate this. There is a correlation, and the likelihood of developing isolated systolic hypertension is higher, the more hypertensive people there are in the family.
Even the presence of one relative is enough to increase the risk of pathology in the phenotype of future offspring by almost 50%.
Of course, this is not a verdict. The situation can be corrected if you carefully follow the rules of prevention and do not play with your own life and health.
Age is also given some importance. As the body ages, phenomena that increase blood pressure increase:
- Decreased receptive function of special cells of blood vessels and heart.
- Impaired glomerular filtration.
- A decrease in general blood flow and local renal, cerebral and muscular hemodynamics due to a decrease in the intensity of cardiac output, all this is the cause of increased upper pressure in the elderly.
Treatment methods
In cases of secondary ISAH, the disease that causes the high blood pressure is treated.
Therapy of the primary form is carried out with a combination of drugs from several groups:
| Group of drugs | Examples |
| Diuretics | Indapamide Hypothiazide |
| Beta blockers | Atenolol Bisoprolol |
| Calcium antagonists | Amlodipine Verapamil |
| Angiotensin-converting enzyme inhibitors | Enalapril Lisinopril |
| Angiotensin receptor blockers | Losartan Valsartan |
In the case of the primary form, treatment is long-term (sometimes lifelong).
Factors in the development of the secondary form of ISAH
Secondary isolated arterial hypertension, when high upper pressure with normal lower pressure, is much more common and, as the name suggests, has an indirect origin, due to the course of a particular disease.
The list of such pathologies is quite impressive:
- Diabetes. With the development of such a disease, blood pressure constantly increases in different ways. ISAH phenomena are possible in the most unfavorable case.
The general hemodynamics of the body is disrupted, since diabetes affects all systems and organs.
Patients with such a severe endocrinological diagnosis should be regularly checked and fully treated so as not to miss the moment.
Attention:
Diabetics often develop persistent, resistant types of hypertension if treatment is not started on time.
- Prolonged stressful situations. Strictly speaking, psycho-emotional stress is not a disease.
However, it triggers a pathological mechanism for the production of large amounts of catecholamines and corticosteroids, which cause a sharp jump in the thermometer reading, which is not always uniform.
This is a risk factor for early stroke or heart attack. It is necessary to control yourself so that your health does not fail at the wrong time.
- Atherosclerosis of blood vessels, especially the aorta. Accompanied by severe stenosis or blockage of the lumen of the blood supply structure.
As a result, a plaque or area of narrowing is formed. Blood cannot overcome the obstacle, cardiac output increases - this is why the upper pressure rises, while the lower remains normal.
- Increased concentrations of calcium and sodium in the circulatory system. Both substances provoke fluid retention, as a result of which the filtering function of the kidneys is impaired.
- Itsenko-Cushing syndrome with symptoms of hypercortisolism. A condition where the adrenal glands produce excess amounts of cortisol.
The reason for this is tumors of the glands or disruption of the pituitary gland with excessive synthesis of corticotropin, which stimulates the production of corticosteroids.
It is not difficult to identify such patients even by eye: a characteristic physique, arterial hypertension, problems with bones, muscles, and the reproductive system.
High upper pressure with normal or low diastolic pressure can form due to aortic valve insufficiency.
- Hyperthyroidism. Another significant risk factor for the development of isolated hypertension. In this case, there is an excess of thyroid hormones or active substances produced by the thyroid gland.
- Kidney failure.
- Prolonged increase in body temperature to significant levels.
- All kinds of congenital heart defects that were not diagnosed in time
- Anemia of any etiology.
The two states are easily differentiated. If there is no evidence for objective pathological processes that could cause ISAH, a diagnosis of the primary form is made.
The pulse rate in this case is important only within the framework of determining the etiology of the process. It does not indicate any specific disease.
When the heart rate increases, the cause must be sought in the heart, blood vessels, hormonal status, and kidneys. A low pulse indicates an anemic process and some other pathologies.
Forecast
Arterial hypertension, when the upper pressure is high and the lower pressure is normal in 68%, is combined with diabetes, pathology of lipid metabolism and ischemic disease, which significantly increases the risk of developing vascular and cardiac complications.
75% of people in the older age group are diagnosed with increased blood pressure, of which 52–87% have ISAH. 84% of the population dies every year from vascular pathology due to a constant form of high blood pressure.
Treatment of hypertension reduces mortality by 17%, and the risk of fatal complications (sudden death, stroke, heart attack) by 32%.
There is no complete cure for the disease - hypertension requires constant, lifelong therapy, but its implementation is the key to extending the quality and duration of life.
Is it possible to develop isolated hypertension during pregnancy?
Yes, such a scenario is quite possible. The mother's body optimizes its activity, devoting all its strength to the benefit of the fetus.
Depending on the initial parameters, such as general health, endocrine status, the presence or absence of bad habits, the nature of professional activity, physical activity, normal blood pressure before pregnancy, we can talk about certain conditions during gestation.
Women more often have arterial hypotension, that is, low blood pressure. But everyone cannot be assessed by one criterion. ISAH also occurs. As a rule, the condition returns to normal after childbirth and stabilizes within the first month.
In any case, it is recommended to be observed by a cardiologist, especially if childbirth does not improve the situation.
What is high blood pressure?
High blood pressure (BP) is said to occur when its systolic and diastolic components rise above the physiological threshold.
Normal blood pressure according to WHO:
- systolic (upper) – 120-129 mm Hg. st;
- diastolic (lower) – 80-84 mm Hg. Art.
If, when measuring blood pressure, the upper number is 140 or higher, and the lower number is 90 or higher, then this pressure is considered elevated. It should be understood that systematically recorded high blood pressure is considered a pathology. Episodes of its increase in the morning, during intense physical activity, fear, and stress are natural for the body.
According to medical observations, the following blood pressure levels are considered very dangerous - for the upper 180, for the lower 120. In this case, there is a high probability of developing a hypertensive crisis.
How can you reduce the upper pressure without affecting the lower reading?
It is impossible to solve such a survey on your own. Qualified medical assistance is required.
Moreover, if the systolic pressure is in the range of 170-180 or higher, you should not wait, you need to call an ambulance to resolve the issue of hospitalization in a cardiology hospital.
Before doctors arrive, you need to take a semi-sitting position with your legs bent to normalize blood flow in the brain.
Taking pills is strictly prohibited; this can lead to unpredictable consequences, including a stroke or heart attack.
The maximum that can be done is to take mild sedatives in tablet form, such as motherwort or valerian, Valocordin.
High systolic pressure and low diastolic pressure require hospitalization. Even medications prescribed by a doctor cannot be used: the risks of inadequate pharmaceutical exposure are high.
All recommendations circulated online and in print publications of dubious quality about showers, baths, rubdowns, and folk remedies should be ignored. This is sabotage advice, fraught with dangerous consequences.
What is the danger?
The situation when systolic pressure increases one-time due to temporary reasons (for example, strong emotional overexcitation) is not quite dangerous. As soon as a person manages to cope with his experiences, the pressure normalizes on its own.
A frequent increase in the indicator is a rather dangerous phenomenon that can lead to all sorts of complications:
- hypertensive crisis;
- circulatory disorders in the brain - stroke;
- acute myocardial infarction;
- rapid development of heart failure;
- rapid development of irreversible kidney pathologies.
One of the most dangerous complications of increased upper pressure is the development of malignant hypertension. This pathology cannot be treated: 2-3 months after the development of the disease, the patient dies due to the appearance of associated complications.
Symptoms requiring an ambulance call
It is recommended to call an ambulance in any case as soon as the patient realizes that isolated hypertension is occurring.
The list of manifestations dangerous to health and life is characterized by the following points:
- Headache of significant intensity. Caused by hemodynamic disturbances and stenosis (narrowing) of blood vessels in the brain.
- Dizziness, especially severe.
- Nausea, accompanied by repeated vomiting without signs of mitigation.
- Chest pain of a pressing, aching nature. They give it to the epigastric region, the hands, and do not allow breathing.
- Shortness of breath, as they say, out of the blue without physical exertion. This is explained by a violation of cellular nutrition, which is very dangerous.
- Changes in the nature of the heart rhythm (an increase of more than 100 beats per minute, or a decrease of less than 60).
- Fainting states of any frequency.
- Impairments of consciousness, up to the development of mental disorders.
- Inability to speak normally or control one’s own body.
All these are symptoms that require urgent qualified help. Without treatment, dangerous and even fatal complications are possible. Therefore, amateur activities are excluded. At the first suspicion, you should call doctors and calmly wait for their arrival.
Diagnostics
It involves a complete examination of the patient by several specialists: a cardiologist, an endocrinologist, a nephrologist and a neurologist in the system.
An approximate list of diagnostic measures looks like this:
- Questioning the patient. It involves identifying subjective sensations. That is, the actual symptoms of the condition.
- Anamnesis collection. The factors of the presence of bad habits and somatic diseases are established.
- Measuring blood pressure levels on both arms with minor breaks.
- Daily Holter monitoring using an automatic tonometer.
- Electrocardiography. In the right hands it is highly informative.
- Encephalography.
- Study of hormone levels.
- Blood biochemistry, general analysis.
- Urine examination.
- Angiography or Dopplerography as necessary.
The final list of measures is determined by doctors; it can be either shorter or longer.
How is isolated arterial hypertension with high systolic values treated?
The set of measures is generally identical to those for classical hypertension. Etiological treatment is necessary to eliminate the underlying disease that caused the pathological condition.
Symptomatic therapy consists of the use of combination drugs or the use of narrowly targeted medications:
- ACE inhibitors.
- Diuretics of various types.
- Calcium channel blockers and beta blockers.
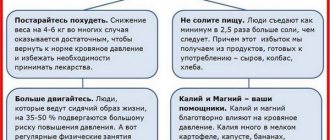
This, however, is not enough. The use of medications is a half-measure. It is necessary to radically change your lifestyle. Quit smoking and alcohol, even in the smallest doses.
It is necessary to optimize the regime of physical activity, no physical inactivity, but you should not bother. Drinking regimen (2 liters of water per day), amount of salt consumed per day (less than one teaspoon).
The diet should contain fresh vegetables and fruits, protein. You need to worry less; stress is one of the risk factors. Although this is not so easy to do.
These methods are quite sufficient to normalize the health of the cardiovascular system.
Preventive measures
{banner_banstat9}
Primary and secondary prevention measures do not present any difficulties. It is enough to follow simple recommendations and follow common sense:
- Quit cigarettes and tobacco products altogether.
- Avoid alcoholic beverages.
- Normalize your diet. As many fortified foods as possible, as little fatty, fried, smoked and sweet foods as possible.
- Move more, but don't overexert yourself. This is fraught with a stroke.
- Consume less table salt.
- Regularly undergo examinations by doctors of the profile described above to monitor the state of the cardiovascular system.
- When prescribing therapy, take the prescribed medications in a timely manner.
A set of measures will prevent the development of hypertension in the future.