Hypovolemia: a dangerous condition that requires immediate attention
What do we know about hypovolemia?
Hypovolemia is a condition when, as a result of fluid loss, the volume of blood that circulates in the human body decreases.
This violation poses a serious threat to the health and life of the patient. A severe degree can lead to hypovolemic shock and the development of multiple organ failure. Therefore, as a rule, the patient requires immediate medical attention: hospitalization and intensive care. Treatment is carried out in a hospital setting.
In rare cases, hypovolemia is caused not by the loss of fluid, but by its redistribution in the tissues of the body. At the same time, the filling of blood vessels with blood is reduced. This phenomenon is called relative hypovolemia. Blood loss and dehydration are absolute.
1.General information
The word “hypovolemia” literally means insufficient blood volume. In most cases, the term is used in relation to a life-threatening condition known in emergency medicine as hypovolemic shock: a sharp reduction or, rather, redistribution of circulating blood volume due to massive traumatic blood loss. However, the content of such concepts as hypo-, hyper- and normovolemia, as well as criteria for objective diagnosis, strategy and tactics of response, remained controversial over the last century and needed a clearer definition.
Most often, the normal volume of circulating blood (BCV) implicitly means a quantity that exactly corresponds to the volume of the vascular bed, ensuring sufficiently effective hemodynamics and metabolism at all levels, normal heart rate and respiratory movements, optimal tone for the body of the main and peripheral vessels . At the same time, “volume of the vascular bed” is also an intuitive concept rather than an objectively measured one. However, hypovolemia in any case poses a serious threat to the further existence of the body; it is manifested by pronounced, severe, often catastrophic symptoms, requiring urgent or emergency resuscitation measures.
A must read! Help with treatment and hospitalization!
What causes the condition
Most cases are associated with severe dehydration, blood loss, and large burns.
Dehydration can be caused by:
- repeated vomiting and diarrhea, excessive sweating
- insufficient fluid intake,
- taking medications, such as diuretics.
Hypovolemia that is caused by loss of plasma rather than blood is called polycythaemic.
Blood loss occurs as a result of injury, surgery, or internal bleeding. Blood loss associated with internal bleeding is considered especially dangerous, since it is not always possible to immediately determine where it is localized.
Massive blood loss is caused by:
- gastrointestinal bleeding,
- rupture of the fallopian tube during ectopic pregnancy,
- rupture of an aortic aneurysm.
A general decrease in blood volume is called normocythemic hypovolemia.
Literature:
- Prehospital correction of hypovolemia / O. A. Tsarev; State budgetary educational institution of higher education prof. education "Saratov State. Medical University named after V. I. Razumovsky" Ministry of Health of the Russian Federation. — Saratov: Saratov State Publishing House. Medical University, 2015. - 141 p.
- From symptom to diagnosis: a guide for doctors / Scott Stern, Adam Saifu, Dayne Altcorn. - Moscow: GEOTAR-Media, 2008. - 810 p.
The text was checked by expert doctors: Head of the socio-psychological service of the Alkoklinik MC, psychologist Yu.P. Baranova, L.A. Serova, a psychiatrist-narcologist.
CAN'T FIND THE ANSWER?
Consult a specialist
Or call: +7 (495) 798-30-80
Call! We work around the clock!
Symptoms
The condition can be recognized by the following signs:
- dry mucous membranes
- pale skin
- decreased skin turgor
- rapid breathing
- lowering blood pressure levels
- tachycardia
- anxiety, confusion
- weak pulse (due to decreased cardiac output)
- thirst
- dizziness
- lack of urination for a long time.
Acute hypovolemia leads to an emergency condition - hypovolemic shock, which can result in coma.
Diagnostics
The main means of establishing a diagnosis is examination and interview (if possible) of the patient.
If hypovolemia is caused by visible trauma, large-area burns, its diagnosis is not difficult.
If a patient is suspected of dehydration or internal bleeding, the patient is sent for a clinical and biochemical blood test, a urine test, which will determine whether there is a change in the water-electrolyte balance.
Also, to clarify the diagnosis, the doctor performs CT, X-ray, ultrasound and endoscopy of organs in which bleeding may develop.
2. Reasons
Most often, the normal volume of circulating blood (BCV) implicitly means a quantity that exactly corresponds to the volume of the vascular bed, ensuring sufficiently effective hemodynamics and metabolism at all levels, normal heart rate and respiratory movements, optimal tone for the body of the main and peripheral vessels . At the same time, “volume of the vascular bed” is also an intuitive concept rather than an objectively measured one. However, hypovolemia in any case poses a serious threat to the further existence of the body; it is manifested by pronounced, severe, often catastrophic symptoms, requiring urgent or emergency resuscitation measures.
Visit our Cardiology page
Hypovolemia in children
Danger of condition
The child's body is not sufficiently adapted to compensate for fluid deficiency. This feature should be taken into account when hypovolemia is suspected, since a state of shock in a child can occur much faster than in an adult. This is even more important the younger the child is. Thus, in children up to one year old, the ductus arteriosus may remain open, which, when fluid or blood is lost, actually deprives the lungs of blood supply. Therefore, the issue of hospitalization of the child is resolved immediately.
Causes
In newborns, hypovolemia can develop due to blood loss through the placenta, internal bleeding as a result of injury, or fluid accumulation in the abdominal or pleural cavity.
In older children, in addition to blood loss, the condition is caused by uncontrollable vomiting and diarrhea due to intestinal infections and intoxication; non-compliance with drinking regime.
Treatment
Treatment is prescribed based on the patient's condition.
Mild degrees require fluid replacement (drip, intravenous).
If the cause is injury, the first thing to do is stop the bleeding. Then restore normal hemodynamic parameters and breathing, while simultaneously treating the injury and pain relief for the patient.
Significant blood loss requires transfusion of plasma, red blood cells, platelets, and donor blood. Further therapy is aimed at preventing thrombosis, associated infections, and preventing renal dysfunction.
Hypovolemia in burn disease
Plasma losses during burns with a large area cause a decrease in blood volume, hypovolemia and hemoconcentration.
The diagnosis of hypovolemia in burns should be proactive in the sense that the diagnosis should be formulated and treatment started even before symptoms of a decrease in blood volume appear. Otherwise, treatment of hypovolemia and burn disease may be significantly more difficult, and the results may worsen. This is explained by the great rapidity of plasma loss during burns and the severe influence of increasing hypovolemia on hemodynamics, the degree of intoxication and the deterioration of the overall results of treatment of the patient.
Due to the predominant loss of plasma during burns, treatment, including restoration of the volume of circulating plasma, should consist mainly of the administration of plasma and albumin solutions. This does not exclude the use of colloidal and crystalloid solutions necessary for the rehydration of tissues suffering from exsiccation. The criteria for choosing infusion media for burn disease are data from central and peripheral hemodynamics, indicators of blood viscosity and electrolyte composition, elimination of symptoms of tissue excision, and intensity of diuresis.
Drugs for hypovolemia
Treatment is carried out in a hospital, often in the intensive care unit. In most cases, infusion therapy is used.
The drugs of choice are solutions of colloids (solutions of gelatin and dextran, for example, rheopolyglucin) and crystalloids (Ringer's solution), blood substitutes (voluven, refortan).
To avoid infections, the patient is prescribed broad-spectrum antibiotics.
To raise the patient's blood pressure, norepinephrine and dobutamine are prescribed.
Treatment of hypovolemia
The main task of the doctor in treating this pathology is to eliminate the deficit in blood volume.
Additionally required:
- Strengthen the work of the heart.
- Improve oxygen supply to tissues.
- Remove toxins.
- Carry out symptomatic pharmacotherapy for acute disorders.
To achieve these goals, infusion-drip therapy is used.
Depending on the stage of the process, droppers are prescribed containing:
- Crystalloids, isotonic solution and 5% glucose.
- Reamberin, Reosorbilact.
- Dextran solution, Ringer.
- Plasma substitutes.
Cardiac and respiratory stimulants, hepatoprotectors, nootropics, and metabolic agents are added to the droppers.
In particularly severe cases, red blood cells are used and a blood transfusion is performed.
To prevent the development of hypovolemia in alcoholism, timely treatment of this pathology in a drug treatment clinic, psychotherapy, coding and rehabilitation is required.
List of used literature
- Savelyev V.S. Comparative effectiveness of plasma substitutes for normovolemic hemodilution and correction of acute blood loss / V.S. Savelyev, N.A. Kuznetsov // Vestn. surgery. –1985.
- Bryusov P.G. Emergency infusion-transfusion therapy for massive blood loss / P.G. Bryusov // Hematology and transfusiology. –1991. – No. 2.
- Pshenisnov K.V., Aleksandrovich Yu.S. Massive blood loss in pediatric practice. Hematology and transfusiology. 2020;65(1):70-86
- Pleskov A.P. Invasive monitoring of central hemodynamics. // Intensive care, ed. V.D.Malysheva, M.: Medicine, 2002. P. 175–190.
Frequently asked questions about hypovolemia
What diseases can cause hypovolemia?
The condition occurs with gastrointestinal diseases, accompanied by uncontrollable vomiting and diarrhea, kidney disease, sharp drops in blood glucose levels, and some allergic reactions. However, hypovolemia is most often caused by blood loss or extensive burns.
How does hypovolemia manifest?
The patient has dry mucous membranes, tachycardia, thirst, and impaired skin turgor. As the condition worsens, a drop in blood pressure, weak pulse, and rapid breathing occur. In the acute stage - confusion.
How is hypovolemia treated?
The main method of treatment is fluid replacement. In most cases, intravenous administration of saline or electrolyte solutions is used.
Etiology and pathogenesis of hypovolemia
What can happen in the body during hypovolemia:
- The level of proteins and electrolytes in the liquid component of the blood and in the extracellular space changes.
- Peripheral vessels dilate, thereby increasing the capacity of the vascular bed as a whole.
- Hypovolemia can develop due to the direct removal of blood cells and plasma from the body.
The causes of hypovolemia may be the following:
- Bleeding accompanied by blood loss.
- Shock.
- Development of burn disease.
- Allergic reaction.
- The development of dehydration against the background of damage to the body by intestinal infection.
- Pathological or physiological hemolysis.
- Vomiting during pregnancy, caused by toxicosis.
- Excessive urine output due to kidney disease.
- Diabetes mellitus and diabetes insipidus.
- Inability to drink water, for example due to tetanus or rabies.
- Overdose of certain medications. In terms of the development of hypovolemia, special caution should be exercised in relation to diuretics.
When blood volumes in the body decrease, it leads to various disorders in the body. First, he tries to compensate for them on his own, and then these violations lead to irreversible consequences. They cannot be corrected even through therapeutic measures. Therefore, hypovolemia should be eliminated immediately after its detection.
The capacity of the vascular bed and blood volumes are two concepts that exist in a tight connection in the human body. When the volume of fluid changes, the vascular bed changes its capacity to compensate for its deficiency or excess. If the body's blood volume decreases, it reacts to this with a spasm of the capillaries, which allows it to replenish its reserves in large vessels. Thus, it compensates (fully or partially) for the resulting hypovolemia.
In case of allergies and poisoning, when blood volumes do not change, an increase in the vascular bed occurs, thus the body also tries to compensate for the relative hypovolemia. Indeed, against the background of these reactions, the return of venous blood to the heart decreases. This threatens to disrupt its functioning and oxygen starvation of tissues.
Hypovolemia can develop with pathologies of the endocrine and urinary systems. Blood volumes decrease due to the abundant removal of water from the body, and along with it come salts that can retain fluid. Diabetes mellitus contributes to the development of hypovolemia due to the fact that urine contains glucose, which attracts large volumes of fluid.
Disturbances in the functioning of the pituitary gland can lead to the development of hypovolemia, since a deficiency of antidiuretic hormone provokes frequent and copious urination. In this case, hypovolemia will not have a severe course, since the body loses not blood reserves, but extracellular fluid during such a violation.
Burn disease contributes to the development of hypovolemia due to the fact that with such tissue damage significant plasma losses occur. Intoxication of the body worsens the situation. In addition, with serious burns, blood microcirculation in the area that was damaged is completely disrupted.
Intestinal infections contribute to the development of hypovolemia, since fluid will be quickly eliminated from the body against the background of severe diarrhea. Vomiting makes the situation worse. About 7 liters of liquid are formed in the intestines of a healthy adult per day; a certain part of it also comes from food, but no more than 2% of these volumes are excreted with feces. Diarrhea can lead to dehydration very quickly.
Diarrhea and vomiting due to intestinal infection in children are very dangerous. The younger the child, the faster he becomes dehydrated and the more difficult it is to restore fluid reserves. Already 2 days after the onset of the disease, the child’s condition can become very serious. The situation is especially dangerous if an intestinal infection is accompanied by high body temperature.
Although a person does not notice it, he loses fluid during breathing and also when he sweats. When an individual is healthy, the body keeps these processes completely under its control. The volume of water that a person drinks throughout the day is enough for him to make up for these losses (if he drinks in accordance with his age norm). When exposed to heat, feverish conditions, or excessive physical exertion, the balance of water in the body may change.
Blood loss is the most common reason that leads to the development of hypovolemia. Bleeding can be external or internal. First of all, blood loss affects the functioning of the heart.
This affects the body as follows:
- Blood pressure decreases, which leads to the supply of blood from reserve reserves - from the muscles and liver.
- Urination is delayed to conserve fluid reserves in the body.
- The blood coagulation system is activated.
- Small blood vessels spasm.
The body uses all these mechanisms to compensate for hypovolemia: it uses blood depots, tries to preserve it in large vessels due to capillary spasm, and activates the blood coagulation system to stop bleeding. This allows you to continue to supply blood to life-supporting organs: the brain, heart and kidneys for as long as possible.
At the same time, the inclusion of such compensation mechanisms negatively affects the blood supply to peripheral organs. After all, they begin to suffer from hypoxia and acidification of the internal environment. In small vessels, the likelihood of blood clots increases.
Provided that the person does not receive emergency assistance, he will die from hypovolemic shock.
So, the mechanisms of development of hypovolemic shock are identical, regardless of the cause that provoked it. At first, the body tries to compensate for the existing disorder by concentrating blood volumes in life-supporting organs, but over time, the blood flow is decentralized, which leads to disruption in the functioning of all organs. The state of shock, if it occurs, progresses very quickly.
Hypovolemic shock is the end stage of hypovolemia. Very often, shock leads to irreversible consequences, is difficult to correct, and causes serious changes in blood vessels and internal organs. Blood pressure decreases greatly, all tissues experience acute hypoxia. A person develops liver, eye, heart and respiratory failure. The patient falls into a coma, which ends in death.
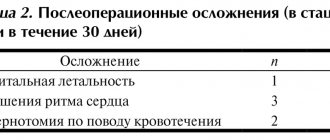
The picture below shows a graph of the development of hypovolemia during hemorrhage: