The term “chronic cor pulmonale” refers to changes in the heart muscle caused by lung diseases. This excludes cases of pathology complicating diseases of the heart and large vessels (mitral stenosis, cardiosclerosis after a heart attack, congenital defects, dilated cardiomyopathy).
In diagnosis, an indispensable condition must be a primary violation of the structure of the lung tissue and its functions. The prevalence of the recorded pathology among the adult population allows us to place it in third place after ischemic and hypertension diseases.
In the International Classification of Diseases (ICD-10), types of chronic pulmonary heart disease are included in the general class of cardiovascular diseases. Codes I26, I27, I28 differ in etiological factors. All cases are united by the gradual formation of overload of the right side of the heart due to the development of high blood pressure in the pulmonary circulation.
Causes
Depending on the causes, the WHO Expert Committee has developed a classification of chronic pulmonary heart disease. Diseases are divided into 3 groups:
- group 1 - diseases associated with impaired passage of air through the alveoli, these can be mechanical obstacles (bronchial asthma), inflammatory lesions (tuberculosis, chronic bronchitis, bronchiectasis, pneumoconiosis), replacement of lung tissue with fibrous tissue (systemic lupus erythematosus, sarcoidosis, eosinophilic infiltration ), a total of 21 nosologies are included;
- group 2 - diseases that impair ventilation of the lungs by affecting the auxiliary mechanisms of breathing (skeletal skeleton of the chest, ribs, muscles), this includes curvature of the spine, adhesions in the pleural cavity, chronic diseases associated with impaired neuromuscular conduction (poliomyelitis) , artificial hypoventilation after surgical interventions on the chest organs;
- group 3 - vascular lesions of the lungs (arteritis, thrombosis and embolism, compression of the main vessels by a tumor, aortic aneurysm and others).
All risk factors for underlying disease accelerate and negatively affect the heart.
Classifications and examples of diagnosis formulation
The severity of circulatory failure (CI) is assessed according to the classification of the Association of Phthisiologists and Pulmonologists of Ukraine (2003). The classification involves dividing patients into groups according to three stages of NC:
1) NC stage I: the presence of mild signs of blood stagnation in the systemic circulation - swelling in the legs, enlarged liver, which disappear under the influence of therapy only for the underlying disease or in combination with diuretics;
2) NC stage II: the presence of pronounced edema and hepatomegaly, requiring intensive, often combined treatment with diuretics; at this stage, as a rule, disturbances in the contractile function of the myocardium are observed, and therefore complex treatment using drugs to correct vascular tone, inotropic drugs, and antiplatelet agents is advisable;
3) NC stage III: terminal stage, characterized by secondary damage to other organs and systems; the only remedy that can at least slightly prolong the life of these patients is continuous oxygen therapy.
The above division of patients into groups depending on the stage applies only to NK in the systemic circulation, since post-capillary stagnation of blood in the pulmonary circulation (left ventricular failure in the form of cardiac asthma and pulmonary edema) in patients with chronic lung diseases, as a rule, is not observed.
The formulation of the diagnosis consists of four components: the name of the disease (indicating the degree of severity and phase of the course), LN (indicating the degree), chronic pulmonary heart disease, NC (indicating the stage). For example: chronic obstructive pulmonary disease, stage III, exacerbation phase, stage II pulmonary disease, chronic pulmonary heart disease, stage I NC.
What happens in the body
In patients of groups 1 and 2, all changes develop due to spasm of small arterioles in the lung tissue as a reaction to insufficient oxygen supply. In group 3, in addition to spasm, there is a narrowing or blockage of the vascular bed. The pathogenesis of the disease is associated with the following mechanisms.
- Alveolar hypoxia (lack of oxygen in the alveoli) - scientists associate vascular spasm in response to hypoxia with disturbances in sympathoadrenal regulation. There is a contraction of vascular muscles, an increase in angiotensin-converting enzyme (ACE), calcium in the blood, and a decrease in relaxation factors of the pulmonary vessels.
- Hypercapnia - an increase in the concentration of carbon dioxide in the blood does not directly affect the vascular wall, but through acidification of the environment and a decrease in the sensitivity of the respiratory center of the brain. This mechanism enhances the production of aldosterone (adrenal hormone), which retains water and sodium ions.
- Changes in the vascular bed of the lungs - compression and emptying of capillaries due to developing fibrous tissue is important. Thickening of the muscular walls of the pulmonary vessels contributes to the narrowing of the lumen and the development of local thrombosis.
- An important role is played by the development of anastomoses (connections) between the bronchial arteries, belonging to the systemic circulation, and the pulmonary vessels.
- The pressure in the systemic circle is higher than in the lungs, so the redistribution goes towards the pulmonary vascular bed, which further increases the pressure in it.
- In response to hypoxia, blood cells that carry hemoglobin and erythrocytes change. Their number increases simultaneously with platelets. Favorable conditions for thrombus formation are created and blood viscosity increases.
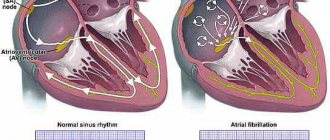
All taken together leads to increased load on the right ventricle, hypertrophy, and then failure of the right heart. An enlarged right atrioventricular orifice contributes to insufficient closure of the tricuspid valve.
Pathogenesis
In accordance with the modern, so-called vascular theory, hypercapnia plays a key role in the pathogenesis of edema syndrome in CLS. Carbon dioxide, being a vasodilator, with an increase in its content in the blood, reduces peripheral vascular resistance and increases the capacity of the arterial bed. Due to the reduction of precapillary tone, the filtration equilibrium point in the capillaries shifts distally, which leads to the movement of fluid outside the vascular bed and loss of plasma volume. Of great importance in the development of edema in CLS is compensatory erythrocytosis in response to hypoxemia, an increase in hematocrit with a violation of the rheological properties of blood, the formation of erythrocyte aggregates, the development of capillary stasis, which causes perfusion disturbances and the movement of the liquid fraction of blood outside the vascular bed. The occurrence of edema is also facilitated by extrathoracic deposition of blood due to increased intrathoracic pressure and prolongation of exhalation, which significantly worsens the conditions for venous return of blood to the heart and creates the preconditions for stagnation in the systems of both the superior and inferior vena cava.
As the resistance load increases due to pulmonary hypertension (PH), hypoxemia, and metabolic disorders in the myocardium, hypertrophy, dilatation and failure of the right ventricle of the heart develop. In patients with diseases that primarily affect the pulmonary vessels (idiopathic PH, postthromboembolic PH, etc.), the leading cause of the development of peripheral edema is right ventricular heart failure (HF) due to hemodynamic overload caused by high PH.
Clinical course
Soviet pulmonologists B. Votchal and N. Palev proposed a clinical description of the stages of development of the pulmonary heart:
- in the initial (preclinical) stage - there are no symptoms of hypertension in the pulmonary circulation, hypertension is possible temporarily with an exacerbation of pulmonary disease;
- in the second stage - there is right ventricular hypertrophy, but all signs are compensated; instrumental examination reveals stable pulmonary hypertension;
- third stage - accompanied by decompensation (pulmonary heart failure), there are symptoms of right ventricular overload.
Clinical manifestations
At the early stage of the disease, the manifestations of chronic pulmonary heart disease do not differ from the typical symptoms of major pulmonary diseases. They intensify with exacerbation and are treatable.
Shortness of breath is a consequence of oxygen deficiency, but it also accompanies inflammation of the lung tissue, emphysema. The intensity does not always correspond to the degree of hypoxia.
Changes in the phalanges occur due to impaired nutrition of the periosteum
Tachycardia is a nonspecific symptom; the heart rate increases in various diseases that are associated with an activated sympathetic nervous system and increased release of adrenaline.
Chest pain is not similar to angina. They are believed to be caused by insufficiency of the coronary vessels, which have to feed the thickened muscle of the right ventricle. Spasm of the arteries of the heart and intoxication of the myocardium with inflammatory products are also important.
Increased fatigue and weakness occur when the shock capacity of the heart decreases. Peripheral tissues of various organs, including the brain, lack blood supply.
Heaviness in the legs, swelling - in addition to myocardial weakness, an increase in the permeability of the vascular wall plays a role. Swelling occurs on the feet and legs. They intensify in the evening and subside during the night. In the third stage, they spread to the thighs.
The feeling of heaviness and pain in the right hypochondrium is caused by an enlarged liver and stretching of its capsule. In a severe form of the disease, ascites simultaneously appears and the abdomen “grows” rapidly. This symptom is more pronounced in elderly patients with concomitant atherosclerosis of the abdominal arteries.
A cough with a small amount of sputum is more associated with the underlying pathology of the lungs.
Manifestations of encephalopathy - chronic lack of oxygen and excess carbon dioxide cause pathological disorders in the brain, disrupt vascular permeability, and promote edema. Patients have 2 possible symptoms:
- increased excitability, aggressive behavior, euphoria, development of psychosis;
- lethargy, lethargy, indifference, drowsiness during the day, insomnia at night.
In severe cases, seizures occur with loss of consciousness or dizziness, cold sweat and decreased blood pressure.
Clinical picture
The basis for the clinical diagnosis of CHL is the addition to the clinical symptoms of the underlying disease (cough, wheezing in the lungs, etc.), manifestations of pulmonary insufficiency (shortness of breath, cyanosis), pulmonary hypertension (emphasis of the second tone over the pulmonary artery, Graham-Still noise) signs of blood stagnation in the large circle - peripheral edema and hepatomegaly. Swelling initially occurs on the feet and legs, progressing to the upper parts of the body. In the evening, as a rule, they increase. The liver is enlarged mainly due to the left lobe, has a rounded edge, is sensitive or moderately painful on palpation. In some cases, the liver can protrude from under the edge of the costal arch even if its size is normal, which is often observed with pulmonary emphysema and a low position of the diaphragm.
Swelling of the neck veins is often a consequence of increased intrathoracic pressure, with the veins swelling during exhalation and collapsing during inspiration. With the development of right ventricular failure, the dependence of the filling of the jugular veins on the respiratory phase decreases.
Diagnostics
In people with chronic cor pulmonale, the diagnosis can be suspected by their appearance: in the compensation stage, dilated skin vessels appear in the cheek area (blush) and on the conjunctiva (“rabbit eyes”). Cyanosis is found on the lips, tip of the tongue, nose, and ears.
When examining the fingers, changes in the nail phalanges are visible: they become flat and widened (“drumsticks”). Unlike heart failure, the arms and legs remain warm to the touch.
Swollen veins in the neck indicate the formation of stagnation at the level of the veins of the systemic circulation, more pronounced at the height of inspiration
When auscultating the heart, the doctor hears:
- characteristic changes in tones above the pulmonary artery;
- in the stage of decompensation - a murmur indicating insufficiency of the right atrioventricular valve;
- a lot of different types of wheezing in the lungs against the background of altered breathing.
The x-ray reveals a typical bulging of the contours of the pulmonary artery, an enhanced tissue pattern, and an expansion of the zone of lymphatic vessels. This indicates an increase in pressure in the pulmonary circle. In the decompensation stage, the heart shadow expands to the right.
Echocardiography assesses the strength of the right ventricle, the degree of dilatation, and overload. Due to increased pressure, the wall of the interventricular septum bends to the left.
Respiratory functions are measured with special devices, and the spirogram is deciphered by a doctor in the functional diagnostics office.
The study of pressure in the pulmonary artery is carried out in complex diagnostic cases. A reliable sign of hypertension in the pulmonary circle is considered to be a resting pressure of 25 mm Hg. Art. and higher, and with load - over 35.
Instrumental and other diagnostic methods
X-ray of the chest organs. In patients with chronic lung diseases, small sizes of the atria and ventricles are usually observed; there may be signs of hypertrophy of the outflow tract from the right ventricle - bulging of the pulmonary cone. In severe cases, the second arch of the pulmonary cone protruding along the left contour can imitate the mitral configuration of the heart. In subsequent stages of development of CHL, a progressive enlargement of the right ventricle due to hypertrophy and dilation is determined. In patients with the vascular form of CHL (idiopathic and chronic post-embolic PH), the trunk and main branches of the pulmonary artery are significantly dilated. A reliable sign of high PH is an increase in the diameter of the right descending branch of the pulmonary artery by more than 18 mm. Sometimes the expansion of the right descending branch becomes aneurysmal in nature, and the aneurysm on the radiograph is mistaken for a neoplastic or tuberculous process. The sizes of the right atrium and right ventricle are sharply increased, while the left parts of the heart may be reduced.
Electrocardiography (ECG) allows you to confidently diagnose right ventricular hypertrophy in patients with the vascular form of CHL (Rv1 > 7 mm, often in combination with complete right bundle branch block, Rv1 + Sv5 > 10.5 mm and other direct signs of hypertrophy). In patients with CLS caused by primary damage to the bronchi and lung parenchyma, an S-type electrocardiogram is usually recorded. However, it should be noted that hypertrophy is a normal reaction of the myocardium to hyperfunction (compensatory increase in cardiac output in response to hypoxemia and resistance load due to PH), which is observed in patients without signs of circulatory decompensation, that is, without CHL. An ECG can be useful if concomitant diseases of the cardiovascular system are suspected, for example, coronary artery disease (depression of the S-T segment, changes in the T wave, etc.), in diagnosing metabolic disorders in the heart muscle, manifested mainly by disorders of myocardial repolarization processes.
Echocardiography (EchoCG) is the most accurate method for diagnosing hypertrophy, dilatation and failure of the right ventricle of the heart; measurement of the thickness of the anterior wall of the right ventricle is carried out in M-mode using a standard anterior approach. In healthy individuals, this figure usually does not exceed 0.3 cm, in patients with chronic lung diseases, the thickness of the anterior wall ranges from 0.3 to 0.45 cm, in vascular forms of CHL - more than 0.5 cm. Assessment of the degree of dilatation of the right ventricle based on determining the anteroposterior size of its cavity is not reliable enough; a more reliable way is to analyze orthogonal sections from the apical approach based on the Simpson method. The main sign of impaired contractile function of the right ventricle is a decrease in the ejection fraction (normal - 46.8 ± 1.48%).
The study of the gas composition and acid-base state of the blood allows you to diagnose and assess the severity of arterial hypoxemia (PaO2 < 65 mm Hg, SaO2 < 93%), hypercapnia (PaCO2 > 40 mm Hg), and respiratory acidosis. Signs of compensated respiratory acidosis are an increase in PaCO2, bicarbonate content and excess buffer bases at normal blood pH. Signs of uncompensated acidosis are an increase in PaCO2, a decrease in the level of bicarbonates, excess buffer bases and blood pH. In idiopathic and post-embolic PH, right ventricular heart failure often develops against the background of hypocapnia and respiratory alkalosis.
Functional classes
During the examination, it is necessary to establish the functional class of manifestations of cor pulmonale.
- Class 1 - the main symptoms are diseases of the bronchi and lungs, hypertension in the pulmonary circle is detected only with instrumental examination and stress tests;
- Class 2 - in addition to the listed symptoms, there is respiratory failure due to narrowing of the bronchi;
- Class 3 - respiratory failure is severe, followed by cardiac failure. Constant shortness of breath, tachycardia, dilatation of the neck veins, cyanosis. Studies reveal persistent hypertension in the pulmonary circulation;
- Class 4 - decompensation, all clinical manifestations are pronounced, there are congestion, respiratory and heart failure of the third degree.
Doppler examination allows you to quantify the pressure in the pulmonary artery, measure the reverse flow of blood (regurgitation) from the right ventricle into the atrium
Treatment
Treatment of chronic pulmonary heart disease should begin with the prevention of exacerbations of respiratory diseases, especially colds and flu, with the timely use of antiviral and antibacterial treatment.
Mode Changes
Patients are advised to limit physical activity. Do not visit mountainous areas, since in high altitude conditions even a healthy person experiences oxygen deficiency. And in patients with pulmonary diseases, a reflex vascular spasm occurs and the degree of tissue hypoxia deepens.
Women should be aware of the negative effects of birth control pills.
It is necessary to stop smoking and even staying in a smoky room.
Directions of therapy
All treatment methods are aimed at eliminating or weakening the existing mechanisms of pathology, these include:
- treatment of the underlying pulmonary disease and compensation of lost respiratory function;
- decreased vascular resistance in the pulmonary circulation and unloading of the right ventricle;
- restoration of normal blood composition, antithrombotic therapy.
Oxygen treatment
Oxygen is supplied in a humidified form through a mask, cannulas in the nasal passages, and some clinics use oxygen tents with special air saturation conditions. For a therapeutic effect on chronic pulmonary heart disease, the oxygen level in the inhaled air must be at least 60%.
Therapy is carried out for an hour up to 5 times a day and more often.
Oxygen supply can reduce all symptoms of the disease caused by hypoxia
How to lower pulmonary artery pressure
To reduce pressure in the pulmonary artery, medications of different groups are used:
- calcium antagonists (possible swelling and redness of the face, headache, feeling of heat, decreased blood pressure);
- α-adrenergic blockers - dilate blood vessels, reduce the ability of platelets to stick together (the side effects are the same, increased irritability and weakness are possible);
- inhaled nitric oxide (has no side effects);
- diuretics - medications with a diuretic effect unload the general bloodstream, facilitate the work of the heart (control of the potassium content in the blood is required);
- group of prostaglandins - selectively act on small blood vessels (side effects such as nasal congestion, increased cough, increased blood pressure, headache).
The drugs Heparin and Pentoxifylline are necessary to improve blood flow and antithrombotic action.
In case of severe heart failure, cardiac glycosides are prescribed very carefully.
Patients with symptoms of decompensation are treated in a hospital. Observation and clinical examination are carried out by a local therapist and pulmonologist.
Forecast
The mortality rate of patients from chronic pulmonary heart disease remains high: 45% of patients survive in the decompensation stage for about two years. Even with intensive therapy, their life expectancy is no more than four years. Lung transplantation gives 60% of patients survival over the next two years.
The disease is very difficult to treat. Any person has the opportunity to rid himself of bad habits and take care of his health in a timely manner. The appearance of cough, shortness of breath and other symptoms requires immediate medical attention.