Treatment tactics
Treatment of pulmonary artery diseases depends on the severity of the process. As for stenosis, in the absence of pronounced manifestations, there is no need for surgical intervention, but clinical observation and symptomatic therapy are required.
As the pathology progresses, the question of surgical treatment arises. When the pressure gradient increases above 50 mmHg, the question of surgery is not discussed - it must be performed immediately. Operation options are different. Valvuloplasty can be open, closed, endoscopic - balloon. Indications for a specific intervention are determined by a specialist.
The main directions in the treatment of pulmonary hypertension are the prevention of thrombosis, elimination of spasm of vascular smooth muscle fibers, stopping the proliferation of connective tissue structures of the vascular wall. In this case, the following application is indicated:
· drugs that normalize blood clotting;
· diuretics;
cardiac glycosides;
· vasodilators;
· oxygen therapy.
In case of hypertension, called secondary, complex measures should correct the underlying pathology - the root cause of the increase in pressure in the artery. The list often includes bronchodilators and corticosteroids.
Surgical treatment for hypertension: embolectomy, lung transplant, pulmonary-cardiac complex transplant.
Pulmonary embolism (PE) - symptoms and treatment
Pulmonary embolism (PE) is a blockage of the pulmonary arteries with blood clots of various natures, most often formed in the large veins of the lower extremities or pelvis.
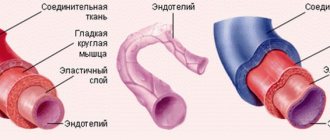
Risk factors for pulmonary embolism include pathological conditions in which there is impaired venous blood return, endothelial damage or endothelial dysfunction, and hypercoagulability disorders.
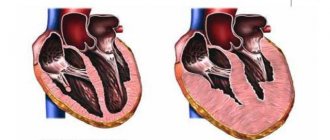
As a result of thromboembolism of the pulmonary arteries, the blood supply to the lung tissue stops, necrosis (tissue death) develops, infarction-pneumonia, and respiratory failure occur. The load on the right parts of the heart increases, right ventricular circulatory failure develops: cyanosis (blue discoloration of the skin), edema in the lower extremities, ascites (fluid accumulation in the abdominal cavity). The disease may develop acutely or gradually over several hours or days. In severe cases, the development of pulmonary embolism occurs rapidly and can lead to a sharp deterioration of the patient’s condition and death.
Every year, 0.1% of the world's population dies from pulmonary embolism. In terms of the frequency of deaths, the disease is second only to IHD (coronary heart disease) and stroke. More patients with pulmonary embolism die than patients with AIDS, breast and prostate cancer, and victims of road accidents combined. The majority of patients (90%) who died from pulmonary embolism were not correctly diagnosed in time and did not receive the necessary treatment. PE often occurs where it is not expected - in patients with non-cardiological diseases (trauma, childbirth), complicating their course. The mortality rate for pulmonary embolism reaches 30%. With timely, optimal treatment, mortality can be reduced to 2-8%.[2]
Symptoms of pulmonary embolism depend on the size of the blood clots, the suddenness or gradual onset of symptoms, and the duration of the disease. The course can be very different - from asymptomatic to rapidly progressing, up to sudden death.
PE is a ghost disease that wears the mask of other heart or lung diseases. The clinic may be infarct-like, reminiscent of bronchial asthma, acute pneumonia. Sometimes the first manifestation of the disease is right ventricular circulatory failure. The main difference is the sudden onset in the absence of other visible reasons for the increase in shortness of breath.
Etiology
PE usually develops as a result of deep vein thrombosis, which usually develops 3-5 days before the onset of the disease, especially in the absence of anticoagulant therapy.
Risk factors for pulmonary embolism
When diagnosing, the presence of risk factors for thromboembolism is taken into account. The most significant of them are: fracture of the femoral neck or limb, replacement of the hip or knee joint, major surgery, trauma or brain damage.
Dangerous (but not so strong) factors include: knee arthroscopy, central venous catheter, chemotherapy, chronic heart failure, hormone replacement therapy, malignant tumors, oral contraceptives, stroke, pregnancy, childbirth, the postpartum period, thrombophilia. In malignant neoplasms, the incidence of venous thromboembolism is 15% and is the second leading cause of death in this group of patients. Chemotherapy treatment increases the risk of venous thromboembolism by 47%. Unprovoked venous thromboembolism may be an early manifestation of malignancy, which is diagnosed within a year in 10% of patients with an episode of PE.[2]
The safest, but still risky, factors include all conditions associated with prolonged immobilization (immobility) - prolonged (more than three days) bed rest, air travel, old age, varicose veins, laparoscopic interventions.[3]
Some risk factors are common to arterial thrombosis. These are the same risk factors for complications of atherosclerosis and hypertension: smoking, obesity, sedentary lifestyle, as well as diabetes, hypercholesterolemia, psychological stress, low consumption of vegetables, fruits, fish, low level of physical activity.
The older the patient, the more likely it is to develop the disease.
Finally, today the existence of a genetic predisposition to pulmonary embolism has been proven. The heterozygous form of factor V polymorphism increases the risk of initial venous thromboembolism by three times, and the homozygous form by 15-20 times.
The most significant risk factors contributing to the development of aggressive thrombophilia include antiphospholipid syndrome with an increase in anticardiolipin antibodies and a deficiency of natural anticoagulants: protein C, protein S and antithrombin III.
Treatment
Standards for the treatment of pulmonary hypertension require a combination of adequate therapy with the use of drugs, implementation of recommendations to reduce symptoms, and surgical methods. Non-drug methods of treating pulmonary hypertension syndrome involve maintaining a water-salt balance, moderate physical activity and oxygen therapy. Doctors at the Yusupov Hospital recommend that patients diagnosed with pulmonary hypertension observe the following restrictions:
- Reduce fluid intake - no more than 1.5 liters per day. Also reduce salt intake;
- Avoid climbing to heights (no more than 1000 meters);
- Avoid fainting, shortness of breath and chest pain, which can be achieved through dosed physical activity.
To treat pulmonary hypertension, drugs are used whose action is aimed at restoring the function of the respiratory and cardiovascular systems. Using medication, specialists are able to reduce the load on the heart, dilate blood vessels and lower blood pressure.
At the Yusupov Hospital, cardiologists prescribe the following pharmacological drugs to patients with pulmonary hypertension:
- Calcium antagonists. They change the heart rate, relax the muscles of the bronchi, reduce spasm of pulmonary vessels, reduce platelet aggregation, increase the stability of the heart muscle;
- Diuretics. Remove excess water from the body, reduce blood pressure;
- ACE inhibitors. Dilate blood vessels, reduce the load on the heart, reduce blood pressure;
- Nitrates;
- Antiplatelet agents. Reduce the ability of red blood cells and platelets to stick together. Prevents them from sticking to the inner lining of blood vessels;
- Direct acting anticoagulants. These drugs prevent the formation of fibrin (a substance in the blood that forms the basis of a blood clot) and also prevent the formation of blood clots (thrombi);
- Indirect anticoagulants. Drugs belonging to this group affect blood clotting and also reduce blood clotting;
- Endothelin receptor antagonists;
- Bronchodilators. These drugs improve ventilation;
- Nitric oxide NO in the form of inhalations - for vasodilation;
- Antibiotics - if there is a bronchopulmonary infection;
- Prostaglandins. Powerful vasodilators that have a whole range of additional effects, such as preventing the adhesion of platelets and red blood cells, slowing down the formation of connective tissue, and reducing damage to endothelial cells.
Severe pulmonary hypertension in adults requires surgical treatment:
- Thromboendarterectomy – removal of blood clots from blood vessels;
- Atrial saptostomy - creating an opening between the atria to reduce pressure;
- Transplantation of the lung and heart complex or just the lung is used in the later stages of the disease and in the presence of other diseases.
To stop the progression and prevent complications of the disease, contact specialists at the Yusupov Hospital in a timely manner.
Functional classification of pulmonary hypertension
| Class I | There is no restriction on physical activity. Ordinary physical activity does not cause shortness of breath, weakness, chest pain, or dizziness |
| Class II | some decrease in physical activity. Ordinary physical activity is accompanied by shortness of breath, weakness, chest pain, dizziness |
| Class III | severe limitation of physical activity. Little physical activity causes shortness of breath, weakness, chest pain, dizziness |
| Class IV | inability to perform any physical activity without the above clinical symptoms. Shortness of breath or weakness may be present even at rest, discomfort increases with minimal exertion |
Non-invasive diagnostics
Electrocardiography (ECG) reveals signs of hypertrophy and overload of the right ventricle, dilatation and hypertrophy of the right atrium (p-pulmonale), deviation of the electrical axis of the heart to the right.
Chest X-ray allows you to clarify the etiology of PH: identify interstitial lung diseases, acquired and congenital heart defects, and also judge the severity of PH. The main radiological signs of PH are bulging of the trunk and left branch of the pulmonary artery, which form the second arch in the direct projection along the left contour of the heart, expansion of the roots of the lungs, and enlargement of the right parts of the heart. In patients with post-embolic pulmonary hypertension, signs can be identified that indicate the presence of blood clots in the large branches of the pulmonary artery (PA) - dilation of the trunk and main branches of the PA, a symptom of deformation and shortening of the root. A specific symptom is the depletion of the pulmonary pattern in the area of impaired blood supply.
Echocardiography (EchoCG) - Ultrasound of the heart is considered the most valuable non-invasive method for diagnosing PH, as it not only allows one to assess the level of pressure in the pulmonary artery, but also provides important information about the cause and complications of PH. Using this method, it is possible to exclude damage to the mitral and aortic valves, myocardial disease, congenital heart defects with blood shunting, leading to the development of PH. Unfortunately, the method does not allow differentiating post-embolic pulmonary hypertension from other forms of precapillary PH. The exception is rare cases of the presence of massive thrombi in the trunk and main branches of the pulmonary artery in the immediate vicinity of the bifurcation.
Kinds
Doctors distinguish several main types of pulmonary hypertension:
- Primary – a disease of unknown origin, which can be either congenital or acquired. The disease is called “idiopathic pulmonary hypertension.” It is characterized by changes in the pulmonary artery and enlargement of the right ventricle. Primary pulmonary hypertension causes disability for the patient, and if left untreated, leads to death;
- Secondary - develops as a complication of other diseases: congenital and acquired heart defects, HIV infection, connective tissue diseases, bronchial asthma, pathology of the respiratory system. The disease can develop due to blockage of blood vessels by blood clots. In this case, chronic pulmonary hypertension is diagnosed.