Acute coronary syndrome (ACS) is a serious condition caused by impaired coronary circulation and myocardial ischemia. When the blood supply to the heart muscle completely stops, hypoxia occurs, which is the direct cause of heart attack and death. This deadly pathological process is popularly called a pre-infarction condition or a heart attack. ACS is a general concept that includes a number of processes that are equal in origin and similar in course, but differ in prognosis and likelihood of cure.
Diseases of the cardiovascular system, which are based on coronary insufficiency syndrome, are designated by the term ACS. This is what clinicians call heart diseases in which its blood supply deteriorates: myocardial infarction and unstable angina. These diseases have similar initial manifestations, pathophysiological mechanisms and some treatment principles. That is why the concept of “acute coronary syndrome” was introduced into medical practice. It is used to make a preliminary diagnosis, when all the characteristics of the patient’s pathological process are not fully clarified.
Acute coronary syndrome has an ICD-10 code of 124.9 and the name “Acute coronary heart disease, unspecified.” The causes of the pathology most often are: thrombosis and thromboembolism caused by rupture of an atherosclerotic plaque or erosion of the endothelium of the coronary artery. There is a special form of the syndrome that is of allergic origin. It is associated with excess production of inflammatory mediators by mast cells. Symptoms of the syndrome are: shortness of breath, irregular heart rhythm, pressing chest pain that occurs at rest or with minor physical stress. The most dangerous sign of ACS is sudden cardiac arrest. This diagnosis is usually made in the intensive care unit.
Coronary disease occurs with pronounced periods of exacerbation and remission. IHD worsens under the influence of provoking factors. In this case, its mild form develops - unstable angina or a severe form - myocardial infarction. In the first case, acute ischemia of the heart muscle does not lead to necrosis. Due to narrowing or blockage of the coronary arteries, trophic changes occur that develop gradually, slowly, in steps. After exposure to the trigger factor, an attack of ACS occurs. With myocardial infarction, irreversible cell death occurs. This pathology is much more dangerous - it is accompanied by severe chest pain, impaired breathing and consciousness, and an avalanche-like death of cardiomyocytes. Destruction of large areas is manifested by the most severe symptoms. With angina pectoris, there are no ECG signs of myocardial necrosis and specific biochemical markers in the blood. It is possible to transition from one clinical form of IHD to another.
The characteristic clinical picture of the syndrome allows you to quickly make a diagnosis and help the patient. To save his life, you should know the algorithm for providing emergency medical care and be able to carry out all the necessary measures before the arrival of qualified specialists. Emergency treatment of ACS will help avoid the development of serious complications and death. It is effective only if diagnosed early. General therapeutic measures prescribed to patients depend on clinical manifestations, the severity of pathological changes and the general well-being of the patient.
Currently, acute coronary syndrome is a pressing medical problem. This is due to the high frequency of its occurrence and the need for preventive measures. The development and implementation of a new medical strategy can save the lives of patients with ACS.
Etiology
Various provoking factors and pathological processes lead to the development of acute coronary syndrome.
Atherosclerosis of the coronary arteries is the main cause of the disease. The fatty substances that form the plaque narrow the blood vessels and impede the flow of blood through the narrowed area. The heart stops fully pumping oxygen-rich blood. This leads to chest pain and heart attack. At early stages of the process, lipid structures are highly soluble. As the pathology progresses, they calcify and become rock-hard. You can only get rid of such formations surgically.
When the surface of an atherosclerotic plaque ruptures, a blood clot forms at the site of damage, the lumen of the vessel narrows, and its patency is impaired. These morphological elements of the disease reduce coronary blood flow and disrupt the blood supply to the myocardium. Blood stops circulating normally, and the heart rate increases to compensate for the resistance. Patients' blood pressure rises and their pulse quickens. If the blood flow completely stops due to a plaque or thrombus blocking the vascular lumen, an irreversible process develops - myocardial infarction, and generalized vascular dysfunction occurs.
Currently, there is no unified theory of the origin of acute coronary syndrome. Using statistical and experimental data, scientists were able to identify the main factors that most often lead to the development of coronary diseases.
Factors that trigger the atherosclerotic process and predispose to the development of the syndrome:
- Stress, psycho-emotional stress, nervous shock,
- Persistent spasm of blood vessels of various origins,
- Postoperative complications
- Coronary artery embolism,
- Inflammation of the vascular wall,
- Congenital anomalies of cardiac structures,
- Overweight,
- Smoking,
- Drug use
- Lack of physical activity
- Imbalance of fats in the blood,
- Alcoholism,
- Genetic predisposition to cardiovascular pathologies,
- Increased blood clotting
- High blood pressure,
- Diabetes,
- Autoimmune or infectious vasculitis,
- General hypothermia of the body,
- Taking certain medications
- Age over 55 years.
There are secondary provoking factors that lead to the development of ACS and are not associated with ischemia of the heart muscle. These are non-atherosclerotic causes of the disease that can cause myocardial infarction. These include:
- Traumatic injury
- Long-term insolation,
- Hyperfunction of the thyroid gland,
- Arteritis.
Pathogenesis
ACS is a deadly condition that requires emergency medical care and emergency resuscitation measures. The disease, caused by primary damage to the coronary arteries or secondary changes in them, occurs in various clinical forms that have similar diagnostic and therapeutic features. The slightest delay or incorrect first aid actions can lead to death.
Pathogenetic links of ACS:
- Impact of etiological factors,
- Coronary thrombosis,
- Isolation of biologically active substances from platelets - thromboxane, histamine,
- Arterial spasm,
- A decrease in the intensity of blood flow in the heart,
- Deterioration of blood supply to the myocardium,
- Accumulation of toxins that inhibit contractility,
- Hyperproduction of adrenaline and calcium ions,
- Persistent narrowing of the coronary vessels,
- Blocking the anticoagulant system,
- The release of enzymes into the blood that destroy cells in the necrosis zone,
- Scar formation in the heart muscle
- Impaired contractile function of the heart,
- Inability of the heart chambers to function adequately,
- A drop in oxygen saturation,
- Poor nutrition of the brain, distant organs and systems.
The degree of blocking of the heart vessels by a plaque or thrombus largely determines the mechanism of development of the syndrome:
- Partial narrowing of the lumen - periodic attacks of angina pectoris,
- Complete occlusion - the appearance of dystrophic foci in the myocardium, quickly transforming into necrosis,
- Sudden ischemic changes—ventricular fibrillation and death.
The essence of the pathology, regardless of the type and form of the process, is a malnutrition of the heart muscle caused by stenosis or blockage of the coronary arteries. The main reason that triggers a complex cascade of pathogenetic reactions is atherosclerosis, congenital or acquired defects. Acute coronary syndrome over time can lead to the death of the patient. Recovery requires urgent action.
Contraindicated or not recommended manipulations in patients with ACS:
- do not use a combination of metamizole sodium (analgin) with diphenhydramine (diphenhydramine) for pain relief, do not use antiplatelet drugs against the background of a hypertensive crisis (high risk of hemorrhage - and bleeding) - do not administer drugs intramuscularly - do not use dipyridamole and myotropic antispasmodics (cause steal syndrome) - do not use lidocaine for prophylactic purposes (risk of heart block) - do not use atropine to prevent the vagomimetic effects of morphine
In the following materials, we will consider in detail the treatment algorithm for ACS without ST segment elevation after hospitalization of the patient in the hospital and the features of patient management after discharge from the hospital.
This article is for informational purposes only. Self-medication can be harmful to your health. The use of any drugs mentioned in this article is possible only as prescribed and under the supervision of a physician.
References: 2021 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation European Heart Journal (2021) 42, 1289-1367. doi:10.1093/eurheartj/ehaa575.
Register on our website now to have access to more training materials!
Subscribe to our pages:
Symptoms
Chest pain or cardialgia is the main clinical sign of ACS. This symptom occurs first, is paroxysmal in nature and radiates to the shoulder or arm. With angina, the pain is squeezing, burning, pressing, short-lived, and with a heart attack it is intense, stabbing and cutting, leading to painful shock and requiring immediate hospitalization. The pain is so severe that it prevents you from moving or breathing normally. Persons with ACS cannot find a comfortable position, rush about and are afraid of dying.
Anginal pain is often associated with previous physical or emotional stress. During a heart attack, it lasts more than an hour and brings severe suffering to the patient. With angina pectoris, the attack lasts ten minutes and is repeated periodically. The pain is practically not relieved by nitroglycerin. To relieve it, narcotic analgesics are used.
Symptoms that accompany chest pain and are not mandatory:
- Cold sweat,
- Fluctuations in blood pressure,
- Euphoria and motor overexcitation,
- Worry and anxiety
- Blackout,
- Panic and fear
- Presyncope or syncope,
- Pale skin
- Cyanosis of the nasolabial triangle,
- Shortness of breath, suffocation,
- Cough,
- Nausea and vomiting,
- Heartburn,
- Abdominal pain
- Dizziness,
- Causeless weakness.
The presented points are the basis of coronary syndrome. Manifestations of the disease may not be the same in all people. Their combination allows experienced specialists to quickly and correctly make a preliminary diagnosis. Symptoms may differ depending on the gender and age of the patient, the degree of circulatory disorders and the individual characteristics of the body, as well as the presence of concomitant diseases. Such a clinical picture should alert the patient and force him to see a doctor. You should take the symptoms of ACS very seriously, as this condition is life-threatening.
Establishing diagnosis
Patients with suspected ACS are examined, their complaints are analyzed, the heart is auscultated and percussed, and blood pressure and pulse are measured.
Electrocardiographic examination is the main diagnostic method for ACS. An ECG should be done as soon as possible after the onset of cardialgia. This technique involves recording the electrical activity of the heart using electrodes attached to the skin. First, electrical impulses in the form of waves are displayed on a monitor and then printed on paper. When the myocardium is damaged, its conductive function is impaired. The ECG shows the form of ACS - angina or heart attack.
As soon as the patient’s condition becomes satisfactory, you can move on to a full diagnostic program, including:
- 24-hour Holter monitoring – measuring blood pressure and pulse over 24 hours.
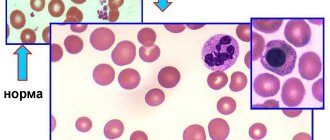
- General blood test, blood for hormones - general examination of the body.
- Clinical examination of urine to determine the functional state of the kidneys.
- BAC - detection of the level of cholesterol, glucose, as well as enzymes that, during the development of myocardial infarction, are released from damaged cardiomyocytes into the blood.
- Coagulogram is an assessment of the functional state of the blood coagulation system.
- Echocardiography is an ultrasound examination of the heart to detect lesions. Ultrasound waves are sent from the device's sensor to the heart and then returned back. The received signals are processed by a computer, and a video image is formed on the monitor screen.
- X-ray examination of the chest cavity - determining the size and shape of the heart and large blood vessels.
- Coronary angiography is an invasive test that identifies the location and extent of narrowing or occlusion of the coronary arteries. A long catheter is inserted into the heart vessels through the large arteries of the arms or legs. The vascular bed is filled with a liquid contrast agent and a series of x-rays are taken, in which the areas of narrowing are clearly visible. During the catheter procedure, the doctor can use tiny balloons to relieve the narrowing. They are introduced into the affected vessel and inflated. At the same time, the narrowing expands and the occlusion is eliminated. To prevent repeated spasm, a stent - a mesh tubular frame - is installed in the artery.
- Scintigraphy – detection of coronary blood flow disorders. Radioactive substances are injected into the blood, and special cameras monitor their uptake by the myocardium. Thus, where blood flow is obstructed, less radioactive material passes through. In the resulting image, such zones appear as dark spots.
- Computed tomography with contrast is performed in difficult diagnostic cases when other methods cannot determine the cause of anginal pain. Before the examination, the patient is injected with a contrast agent intravenously, and then the CT scanner takes a series of images, from which the computer creates a three-dimensional image of the heart. CT scans allow doctors to evaluate the condition of the arteries and detect narrowing or blockages in them.
- Bicycle ergometry is a stress test that is performed after acute signs of cardiac pathology have been removed. This technique allows you to determine the reaction of the heart and blood vessels to physical stress.
- Pulse oximetry - determining the level of oxygen in the blood.
ACS on ECG
All diagnostic measures are carried out under the constant supervision of a cardiologist. If the patient’s condition is serious, he is not examined comprehensively, but is limited only to visual examination data, pulse and pressure indicators, and ECG results. After stabilizing the patient’s well-being, they proceed to diagnostic measures.
Healing procedures
Acute coronary syndrome is a serious pathological condition that requires emergency medical care aimed at stabilizing the patient’s condition, preserving life and preventing further progression of myocardial ischemia and necrosis.
Before the ambulance arrives, the patient needs to measure blood pressure and pulse, open the window for fresh air, sit him down and give him Nitroglycerin. Currently, there are fast-acting remedies for relieving anginal pain - Nitromint and Nitrosorbide sprays. One injection under the tongue is enough to provide relief. The patient is monitored, excluding all possible risk factors.
Inpatient treatment is considered radical. It is selected individually, depending on the severity of the pathology. Patients are prescribed strict bed rest, oxygen inhalations, and medications. Diet therapy is of great importance. Patients should avoid animal products, fatty, spicy and salty foods.
Drug treatment regimen for a patient with ACS:
- Narcotic or non-narcotic painkillers - “Morphine”, “Fentanyl”, “Promedol”,
- Beta blockers – “Atenolol”, “Propranolol”, “Metoprolol”,
- Calcium antagonists - Nifedipine, Amlodipine, Verapamil,
- Nitrates – “Nitroglycerin”, “Erinit”, “Nitromint”,
- Disaggregants – “Plavix”, “Aspirin-Cardio”, “Cardiomagnyl”,
- Statins – “Atoris”, “Simvastatin”, “Cardiostatin”,
- Fibrinolytics – “Urokinase”, “Fibrinolysin”,
- Cardioprotectors - Mildronate, Riboxin, Preductal.
If there is no effect from conservative therapy, patients undergo surgery:
- Stenting of the coronary arteries - expansion of the lumen of the vessel using a balloon and installation of a stent in the narrowed vessel,
- Coronary artery bypass grafting is the replacement of affected areas of blood vessels with special shunts, the creation of an alternative route for blood flow bypassing pathologically altered arteries, and the restoration of coronary circulation.
There are traditional medicine recipes that improve the trophism of the heart muscle. These include: decoctions of nettle or eryngium, infusion of centaury or oat grains.
Experts give patients clinical recommendations that allow the body to recover faster from illness and prevent relapse of the syndrome:
- Eliminate psycho-emotional stress,
- Limit physical activity
- Take a walk in the fresh air every day,
- Eat properly,
- Don't drink or smoke,
- Lead a healthy lifestyle,
- Normalize body weight,
- Monitor blood pressure, cholesterol and blood sugar levels.
Carrying out instrumental examination
- Registration of ECG in 12 leads or transmission of biometric ECG signals to the advisory telemetry center for their urgent interpretation; in the absence of characteristic ECG signs at the beginning, ECG registration can be repeated at intervals of 20-30 minutes
- Pulse oximetry to determine blood oxygen saturation (normal≥95%)
- Conducting risk stratification* in order to optimize the patient’s transportation plan (to select a structural unit of a healthcare institution with the ability to conduct invasive diagnostics and interventional interventions in the optimal time frame)
Forecast
The prognosis for ACS is ambiguous. It depends on the impact of provoking factors, the general condition of the body, age, existing concomitant diseases and structural and functional disorders of the cardiovascular system.
- The prognosis for unstable angina is determined by the location of the lesion: narrowing of the proximal arteries ends in death, and the distal ones are more favorable. With the development of left ventricular failure, the prognosis becomes more complicated.
- Myocardial infarction with ST segment elevation has a benign course. In the absence of this ECG sign, the area of the lesion is important - the larger it is, the more severe the patient’s condition.
Acute coronary syndrome is a dangerous pathology that, if medical instructions are not followed, can lead to serious complications: arrhythmia, persistent cardiac dysfunction, pericarditis, rupture of the dilated aorta, cardiac arrest, stroke, cardiogenic shock, and death. Even with timely and adequate treatment, there remains a high risk of complications. To avoid this, you need to monitor your health, regularly visit a cardiologist and strictly follow all his recommendations.
Treatment of acute coronary syndrome
Hospitalization
A patient with acute coronary syndrome should be admitted to the intensive care unit or intensive care unit for a day. Whether to leave the patient there further is determined by doctors, focusing on ECG indicators over time, his condition (severity), blood tests, etc.
Medicines
The following groups of drugs are used to treat acute coronary syndrome:
- p-blockers
- Nitrates
- Thrombolytic therapy indicated for segment elevation
- Slow calcium channel blockers
- Antithrombotic antithrombin drugs: heparin sodium, low molecular weight heparins - nadroparin calcium, enoxaparin sodium, dalteparin sodium
- Antithrombotic antiplatelet drugs: acetylsalicylic acid, clopidogrel, abciximab, eptifibatide
Nitrates
Nitrates are prescribed to those who have persistent episodes of myocardial ischemia (the clinical picture is mainly pain). Administered intravenously. The dosage is increased until the symptoms disappear. But the clinical picture may persist, but side effects appear, then the nitrates are canceled. Side effects are manifested mainly by headaches or increased blood pressure. If the effect of the drugs is achieved, oral medications are then prescribed instead, according to the recommendations of the 2003 VNOK.
If nitrates are administered IV, the infusion rate should initially be 10 mcg/min. The dose is then increased by 10 mcg/min every 3-5 minutes until symptoms begin to subside or the blood pressure responds.
p-blockers
Drugs from this category have the following effects:
- They reduce myocardial oxygen consumption due to systolic blood pressure and afterload, a decrease in heart rate, and a weakening of myocardial contractility.
- They increase coronary blood flow by improving diastolic perfusion, increasing distal coronary perfusion, and favorable epicardial-endocardial shift.
An effective medicine is Propranolol, the initial dose of which is 0.5-1.0 mg. After an hour, the patient should take the medicine orally at a dose of 40-80 mg every 4 hours up to a total dose of 360-400 mg per day. Metoprolol is effective, its initial dose is 5 mg, administered intravenously over 1-2 minutes. A repeat dose is administered every 5 minutes until the total reaches 15 mg. 15 minutes after the last intravenous administration, oral administration of 50 mg every 6 hours for 48 hours is indicated. Further, the intervals between doses can be increased. The maintenance dose is 100 mg 2-3 times a day. The desired effect is provided by another drug from the series of p-blockers - Atenolol, which is first administered in a dose of 5 milligrams.
Heparin
Unfractionated heparin is used as an anticoagulant treatment. But taking it can lead to bleeding from various parts of the body and organs. To avoid this, you need to monitor the patient's blood coagulation system. The starting dose ranges from 60 to 80 units/kg, it cannot exceed 5000 units.
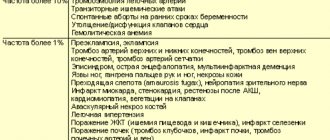
An alternative to unfractionated heparin is low molecular weight heparins . Their administration is simple, sensitivity to platelet factor 4 is less than that of unfractionated heparin, which is one of the advantages of this group of drugs. The following tools are relevant:
- Dalteparin sodium
- Enoxaparin sodium
- Nadroparin calcium
Acetylsalicylic acid
Therapy with these drugs more than halves the risk of death and the development of MI in people with ACS without elevation of the 5G segment. The first dose is 250-500 mg; only uncoated tablets are used. Next you need to take 75-325 mg orally once a day.
Clopidogrel
This drug is prescribed mainly to patients with a high risk of myocardial infarction and death. On the first day you need to apply a loading dose, which is 300 mg, then the dose is 75 mg per day. The course of treatment is 1-9 months.
Conducting a stress test
It is performed for those who are in the low-risk group on days 3-7 after a characteristic attack in the absence of repeated episodes of myocardial ischemia at rest.