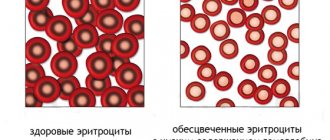
Iron deficiency anemia or IDA is the most common blood disease that occurs in people of different age groups and social classes. But it is especially often diagnosed in pregnant women and children. Iron deficiency anemia is characterized by the occurrence of iron deficiency in the body and a decrease in the number of red blood cells. This may be a consequence of various reasons, but, regardless of their nature, IDA is fraught with the development of disorders of hematopoietic processes, pathologies of the cardiovascular system, decreased immunity, deviations from the norm in the functioning of the organs of the reproductive system, etc.
Iron in the body
In the human body, iron is mainly present in the form of hemoglobin, which contains it. Hemoglobin is a protein with a quaternary structure, responsible for binding oxygen entering the blood during inhalation and transporting it to every cell of the body. Having given them oxygen, it takes carbon dioxide and, entering the lungs with the bloodstream, gives it away, again becoming saturated with oxygen. As a result, during exhalation, a person exhales metabolic products.
In this case, the binding of oxygen and its transportation is ensured precisely by the non-protein part of hemoglobin, or rather by the iron atom directly included in its composition. Therefore, maintaining its amount in the body at the proper level is extremely important.
Hemoglobin is carried by red blood cells and accounts for about 95% of the total intracellular space of each red blood cell. Red blood cells are the most numerous group of blood cells and have a characteristic biconcave disc shape. It is this form of red blood cell that ensures the most efficient performance of the gas exchange function in the body. Therefore, when, due to heredity or the action of other factors, human red blood cells acquire a different shape, for example, a sickle (sickle cell anemia), they are no longer able to maintain gas exchange at the proper level.
But in addition to ensuring the transport of oxygen and carbon dioxide in the body by iron as part of hemoglobin, i.e., performing the function of gas exchange, it is also necessary for:
- synthesis of thyroid hormones;
- maintaining immunity;
- the occurrence of a number of metabolic processes, cell division;
- myelination of nerve fibers (formation of a protective sheath around the nerve);
- DNA products;
- proper breathing, maintaining muscle tone;
- proper functioning of the brain.
The adult body contains an average of 4 g of iron, which depends on gender and age. More than half is concentrated in hemoglobin, 27% is contained in muscles in the form of myoglobin, and 7-8% is deposited in the liver.
Iron is stored or deposited by a specific protein called ferritin. Each ferritin molecule is capable of holding 3000 iron atoms. If there is insufficient supply from the outside, the body begins to use ferritin to meet its needs. But with prolonged iron deficiency, ferritin reserves are depleted, which leads to disruption of metabolic processes and iron deficiency anemia.
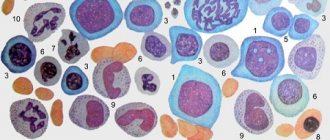
Myelodysplastic syndrome
Myelodysplastic syndromes (MDS) is a pathology of the Stobur cells of the cerebrospinal fluid, which leads to ineffective hematopoiesis and, as a result, to various combinations of anemia, neutropenia and thrombocytopenia. These syndromes are sometimes called pre-leukemic due to their nature and sometimes transform into acute leukemia. MDS in patients with less than 50 years of age rarely occurs, but in patients with more than 65 years of age, the frequency is 5%. To confirm the diagnosis, a bone marrow biopsy is required. This disease is characterized by the presence of chronic cytopenia, hyperplasia of the cerebrospinal fluid and morphological pathology of the progenitor cells in the cerebrospinal fluid.
The response to treatment with chemotherapy, immunosuppressants, growth factors (granulocyte-stimulating hormone and erythropoietin) is limited, and the survival rate of patients does not increase. Therefore, in older patients, treatment is alternated with blood transfusions and other symptomatic therapy.
Prepared by Bogdan Boris
What is ZhDA
IDA is a condition in which the body is deficient in iron, which causes a decrease in the number of red blood cells. As a result, various disturbances in the functioning of the body develop, primarily associated with inadequate gas exchange. Therefore, iron deficiency anemia is characterized by weakness, dizziness and even loss of consciousness, as well as a number of other changes in the condition. This may be a consequence of both insufficient intake of iron from food, and a violation of its absorption in the body or excessive consumption.
Therefore, iron deficiency anemia cannot be a primary disease. It is always a consequence of the occurrence of certain violations. At the same time, it accounts for about 80% of all anemia, which requires careful attention to this problem and its detailed consideration.
WHO statistics show that more than 2 billion people worldwide suffer from iron deficiency anemia. But this is only according to official data. In reality, their number is significantly higher.
Normally, iron enters the body along with plant and animal foods. In plant sources it is found in the form of ferric iron, and in animal sources - ferrous. These forms of iron differ in different rates and degrees of absorption. Iron from animal food sources, or heme, is easily absorbed. But trivalent or non-heme iron obtained from plant foods must first be transformed under the action of hydrochloric acid of the stomach into divalent, and after entering the initial parts of the small intestine with the food bolus, it must again transform into the trivalent form.
Some of the iron accumulates in the mucous membrane of the small intestine, and the rest is absorbed into the blood. Moreover, no more than 2.5 mg of iron can be absorbed per day. In the blood it is bound by the protein transferrin, the production of which is responsible for the liver. The amount of iron absorbed and deposited in the intestines is regulated depending on its level in the body. If excess iron comes from food, it is retained in a larger volume in the cells of the mucous membrane of the small intestine, which are subsequently naturally exfoliated and excreted along with feces.
Iron absorbed into the bloodstream is transported by transferrin in two main directions:
- through the portal vein it enters the liver, where it is deposited in the form of the protein ferritin;
- is delivered to red bone marrow cells, where it is used for the synthesis of hemoglobin and takes part in tissue redox reactions.
If disturbances occur at any of these stages, the body develops iron deficiency. Thus, with a decrease in the acidity of gastric juice, which may be a consequence of atrophic gastritis, the use of antacids, or gastric resection, the body’s ability to convert ferrous iron into ferric iron decreases. This means that it cannot be fully absorbed and subsequently participate in biochemical transformations.
With the development of chronic pathologies affecting the intestinal mucous membranes, their ability to absorb iron also decreases. Therefore, it cannot enter the blood in sufficient quantities.
If the binding process of iron by transferrin is disrupted, it cannot be transported effectively throughout the body. Therefore, it does not enter the red brain cells in the required quantities.
In any of these cases, the consequence is a decrease in the ability to form hemoglobin and other iron-containing proteins, i.e., the development of iron deficiency anemia and other metabolic disorders. As a result of a decrease in hemoglobin production, the resulting young red blood cells are smaller in size, and their total number decreases.
Reasons for development
Thus, we can distinguish 4 main reasons for the development of IDA:
- insufficient intake of iron into the body from food;
- increasing the body's need for iron;
- violation of its absorption;
- disruption of iron transport throughout the body.
Insufficient intake of iron into the body
Food is the main source of iron for the human body. And an unbalanced diet is one of the most common causes of iron deficiency anemia in both children and adults.
In most cases this is due to:
- prolonged fasting;
- vegetarian or vegan diet;
- consumption of monotonous foods with insufficient amounts of heme and non-heme iron;
- anorexia.
For infants, especially during the first six months of life, the only source of iron is mother's milk. Provided that a nursing woman does not have IDA, the child receives it in the required amount. At the same time, transferring a baby to artificial feeding or early introduction of complementary foods often becomes the reason for the development of iron deficiency anemia.
Nan-O-Fer (Switzerland)
Nan-O-Fer (Switzerland) – capsules for oral use, created taking into account the peculiarities of iron absorption in the body. It is Nanofer that today is one of the priority drugs for the treatment of IDA, since it contains liposomal iron in the form of pyrophosphate, and in order to improve the quality of its absorption, vitamins B12, B6 and folic acid are added to the drug.
Eslotin
Check availability
If a nursing mother has a severe form of iron deficiency anemia, this can lead to congenital iron deficiency in the child. This can also occur in premature babies, as well as those born from multiple pregnancies. In such situations, they speak of congenital iron deficiency, and its symptoms appear from the first weeks of the child’s life.
Increasing the body's need for iron
An increased need for iron is usually characteristic of women during pregnancy and breastfeeding. This is due to:
- an increase in blood volume and the number of red blood cells, which requires about 500 mg of iron;
- the need to form the placenta (200 mg);
- ensuring proper development of fetal tissues and organs (300 mg);
- loss of blood during and after childbirth (50-150 mg);
- covering the newborn's needs for this macronutrient (400-500 mg).
During pregnancy and lactation, a woman’s need for iron almost doubles, and with multiple pregnancies it increases even more.
In general, during pregnancy and breastfeeding 1 child, the female body loses about 1 g of iron. Considering the fact that a maximum of 2.5 mg of iron can be absorbed per day, iron deficiency anemia in pregnant women is an almost inevitable condition. But it is within the power of a woman to ensure that it proceeds to the mildest extent through proper preparation for pregnancy, correction of the diet and the use of iron supplements if necessary.
Also, an increase in the body's need for iron occurs during blood loss, which is also most typical for women. Every month, during menstrual bleeding, the female body loses iron. But such losses are physiological and, with proper nutrition, do not lead to the development of IDA. Unfortunately, the lifestyle and diet of most women is not capable of creating sufficient amounts of iron reserves in the body and covering its monthly losses.
But besides menstrual bleeding, other situations accompanied by increased blood loss can lead to iron deficiency anemia in people of any gender and age. But single losses of even a large volume of blood, for example, during severe injuries or operations that violate the integrity of soft tissues, usually do not provoke IDA, since the iron reserves in the body are sufficient to replace them.
Iron deficiency anemia usually develops against the background of chronic and prolonged bleeding, typical of:
- peptic ulcer of the stomach and duodenum;
- hemorrhoids;
- intestinal diverticula;
- Crohn's disease;
- endometriosis;
- uterine fibroids;
- hematuric form of chronic glomerulonephritis;
- frequent nosebleeds;
- systemic vasculitis, systemic lupus erythematosus;
- intestinal polyposis;
- malignant tumors in the terminal stage.
IDA can also occur in donors who donate large volumes of blood more than 4 times a year.
Other reasons for the increased need for this macronutrient are:
- heavy physical labor, active sports;
- period of puberty and active growth;
- parasitic infestations.
Iron malabsorption
Iron absorption occurs through the mucous membrane of the duodenum and the initial parts of the small intestine. This is only possible if their mucous membrane is in normal condition. But there are many diseases that can lead to changes in it, and therefore to disturbances in the absorption of iron from food. These include:
- enteritis is a disease accompanied by inflammation of the intestinal mucosa;
- celiac disease is a hereditary pathology in which the body is not able to absorb gluten, which leads to impaired absorption of all nutrients in the intestines in its presence;
- atrophic and autoimmune gastritis – gastrointestinal pathologies in which destruction of cells of the gastric mucosa is observed;
- resection of the stomach and/or small intestine - surgical interventions performed in the presence of compelling indications, but capable of disrupting the production of hydrochloric acid, which is necessary for the transformation of ferrous iron into ferric iron;
- Crohn's disease is an autoimmune disease of the gastrointestinal tract, accompanied by inflammation of the mucous membranes of the intestines, and sometimes the stomach;
- Helicobacter pylori infection is the main cause of the development of gastritis and peptic ulcers of the stomach and duodenum with impaired formation of hydrochloric acid;
- cystic fibrosis is a hereditary pathology in which the functioning of most glands of the body is disrupted;
- oncological diseases of the stomach and duodenum.
Alcoholism also contributes to damage to the mucous membranes of the gastrointestinal tract, which leads to impaired iron absorption. In addition, alcohol inhibits the activity of red bone marrow, which can aggravate the course of iron deficiency anemia.
Also, the use of a number of medications can provoke disturbances in the absorption of iron in the intestines. This is typical for the use of antacids that reduce the acidity of gastric juice, iron-binding drugs, as well as NSAIDs that are often used by people without prescription and supervision by a doctor (Paracetamol, Ibuprofen, Nurofen, Nise, Diclofenac, Aspirin, etc.). The latter drugs have anti-inflammatory and analgesic properties, but at the same time they negatively affect the condition of the mucous membranes of the gastrointestinal tract and thin the blood.
In such situations, IDA will occur even if there is sufficient intake of heme and non-heme iron in food.
Transportation disruption
The main carrier of iron throughout the body is the protein transferrin. But in a number of situations there is a violation of its synthesis in the body. This is typical for:
- congenital disorders of transferrin production, in which case signs of iron deficiency anemia will be observed from the first months of the child’s life;
- liver pathologies, in particular cirrhosis and hepatitis;
- tuberculosis;
- severe infectious diseases.
Epidemiology
According to the Ministry of Health of Italy, Belgium, Germany and Spain, the annual incidence of iron deficiency anemia is 7.2-13.9 per 1000 inhabitants per year. Increased incidence is observed in women, young and elderly people, patients with gastrointestinal disorders, pregnant women and women with menometrorrhagia, and people taking aspirin or antacids. In countries where meat is not a major part of the diet, iron deficiency anemia is observed 6-8 times more often than in European countries. This occurs even despite equivalent total iron in the diet, since heme iron from meat products is better absorbed than non-heme iron. In a study of children and adolescents from Sudan and Nepal, iron deficiency anemia was found in 2/3 of those included in the study. Moreover, in some regions, intestinal parasites significantly worsen the course of iron deficiency anemia due to constant blood loss in the gastrointestinal tract.
Symptoms
IDA can manifest itself differently in different people. In general, this disease is characterized by the development of 2 syndromes: sideropenic and anemic.
Sideropenic syndrome is caused by the occurrence of disturbances in the condition of the skin and mucous membranes against the background of a lack of iron in the body, i.e., a disturbance in the course of metabolic processes. Therefore, with IDA, the following may occur:
- dryness, decreased skin tone, peeling and cracking;
- fragility and separation of nails, the formation of transverse stripes on them, the development of onychodystrophy with flattening or acquisition of a concave shape by the nail;
- cracks and ulcers in the corners of the mouth (cheilitis);
- development of stomatitis (ulceration of the oral mucosa);
- deterioration of hair condition, including loss of shine, hair loss, increased fragility, which leads to split ends;
- disorders of taste preferences with the appearance of a tendency to eat chalk, lime, coal, earth, paint, etc.;
- pathological desire to inhale unpleasant and even downright toxic odors of solvents, paints and varnishes, gasoline, fuel oil, exhaust gases, etc.;
- diseases of the gastrointestinal tract, including damage to the tongue (glossitis, cracking), gums (gingivitis, periodontal disease), teeth (caries), stomach and intestines (enteritis, gastritis);
- unproductive cough, sensation of a foreign body in the throat, difficulty swallowing;
- discomfort during sexual intercourse, increased incidence of infectious urological diseases;
- disruption of the functioning of the sphincters (circular muscles that close the intestines, urethra, etc.), which leads to stress urinary incontinence, for example, when coughing, nocturnal enuresis, etc.
The most characteristic symptom that occurs in most patients with iron deficiency anemia is pale skin. Often it even takes on a greenish tint. In this case, the sclera (whites) of the eyes may become bluish.
Anemic syndrome develops as a result of impaired gas exchange against the background of a drop in hemoglobin levels. Its main manifestations are:
- weakness;
- fast fatiguability;
- the appearance of drowsiness during the day;
- attacks of dizziness;
- loss of consciousness;
- frequent headaches;
- noise in ears;
- flashing spots before the eyes;
- attacks of shortness of breath during physical exertion;
- increased heart rate (tachycardia);
- discomfort in the heart area;
- lowering blood pressure levels.
Sometimes with iron deficiency anemia there is a persistent increase in body temperature to subfebrile levels, and this may be the only symptom of the pathology. While taking iron supplements, the temperature normalizes.
Quite often, the decrease in the level of iron in the body, and therefore the hemoglobin produced, proceeds smoothly. Therefore, many organs and systems manage to adapt to the changed conditions of existence. During this time, the patients’ well-being gradually deteriorates, but since this happens slowly, they do not notice pronounced changes in their condition and attribute the symptoms that appear to overwork. Therefore, often at the moment when they undergo examination or go to the doctor, a severe form of IDA is already observed.
How does normochromic anemia manifest?
This pathology is characterized by a typical clinical and hematological syndrome
– these are not only changes in the analysis of peripheral blood, but also certain symptoms. First of all, patients note severe weakness and increased fatigue. Often there is dizziness, flickering of spots before the eyes, and some stupor. There may be loss of consciousness, especially when standing up suddenly - so-called orthostatic hypotension. With moderate and severe anemia, shortness of breath appears due to general hypoxia of the body.
Many patients note dullness and brittleness of hair and nails.
Upon examination, the doctor notes the pallor of the skin and visible mucous membranes, the bluish color of the sclera, and a rapid pulse due to the compensatory work of the heart muscle in order to increase the blood pumped per minute and, thus, supply the body tissues with oxygenated blood.
Severe diseases that provoke the occurrence of normochromic anemia have the corresponding symptoms:
- with hemolysis
- yellowness of the skin and sclera, there may be pain in the hypochondrium, body temperature rises, - in case of malignant tumors, the “minor sign syndrome” is very relevant
- pallor, significant weight loss, lack of appetite, aversion to meat food, low-grade fever, - in case of chronic renal failure
- edema, shortness of breath, dyspeptic symptoms due to “slagging” of the body with urea and creatinine, decreased or absent urination, - in chronic inflammatory diseases
- signs of damage to the relevant body systems.
Types and stages of iron deficiency anemia
During the disease there are 3 stages:
- Prelatent iron deficiency. At this stage, there is a decrease in the amount of iron entering the red bone marrow, and a decrease in the volume of iron deposited in the form of ferritin. At the same time, the blood still maintains a normal level of serum iron, as well as hemoglobin and red blood cells. At the stage of prelatent deficiency, most often there are no symptoms of iron deficiency.
- Latent iron deficiency. At this stage, iron reserves in the body are already depleted. The body directs the bulk of its mass for the synthesis of hemoglobin, so its amount in the blood remains within normal limits. But at the same time, the lack of iron is already beginning to affect tissue metabolism, which leads to the appearance of the first, but still mild, signs of anemic and sideropenic syndromes.
- Actually iron deficiency anemia. During this stage, iron levels drop to low levels and iron stores are depleted, resulting in decreased serum iron levels, hemoglobin levels, and red blood cell counts. This is accompanied by an increase in the clinical picture.
Iron deficiency anemia itself can vary in severity, depending on the level of hemoglobin in the blood. Normally, women should have 120-140 g of hemoglobin in each liter of blood. For men, 130-160 g/l is considered normal. Based on the concentration of hemoglobin in the blood, 3 degrees of IDA are distinguished:
- light – 90-120 g/l;
- average – 70-89 g/l;
- heavy – less than 70 g/l.
How to treat normochromic anemia?
Therapy for this type of anemia always comes down to treating the underlying disease. Treatment tactics vary. For anemia of chronic disease (ACD) caused by renal, autoimmune or oncological mechanisms, intramuscular administration of human recombinant erythropoietin
at a dosage of 10,000 IU three times a week.
If the patient has a combined type of anemia, for example, in patients with rheumatoid arthritis (folate deficiency when taking the cytostatic methotrexate and normochromic anemia of a chronic disease), folic acid
, and medications prescribed by a rheumatologist that can reduce autoimmune inflammation in the body.
Regardless of the causative factor, the treatment of normochromic anemia also involves taking iron-containing drugs,
along with treatment of the underlying disease. These are so-called anemias with combined pathogenetic mechanisms. We may also be talking about anemia due to blood loss (posthemorrhagic anemia).
- Mild anemia
(hemoglobin level from 90 to 120 g/l) is treated with a diet high in iron (veal, beef liver, buckwheat, pomegranates), as well as by prescribing tableted forms of iron (ferrum-lek, totema, sorbifer durules) or solutions for intramuscular injections (maltofer). - For moderate anemia
(hemoglobin level from 70 to 90 g/l), intramuscular administration of iron-containing drugs and erythropoietin is indicated. - In case of severe anemia
(hemoglobin level less than 70 g/l), red blood cell transfusion (blood transfusion) is indicated. The treatment is supportive, since the effect of the transfusion only lasts for several months.
Separately, it makes sense to dwell on blood transfusion.
So, the main indication for blood transfusion is a progressive drop in hemoglobin to less than 70 g/l. Erythromass transfusion should only be carried out in a hospital under the supervision of a resuscitator or specialized specialist. The profile of the department can vary - from a surgical or gynecological hospital in the case of massive life-threatening internal bleeding to an oncology or hematology department for the corresponding malignant formations. An absolute contraindication for blood transfusion is acute cardiovascular failure accompanied by pulmonary edema in terminal (extremely severe) patients in an agonal state.
Diagnostics
To diagnose iron deficiency anemia, you should consult a physician or pediatrician, and in complex cases, a hematologist. First of all, the doctor will interview the patient, find out the nature of the complaints, dietary habits, the presence of chronic diseases, etc. Then a clinical blood test must be performed with the preparation of the leukocyte formula. With its help, it is possible to detect not only a decrease in the concentration of hemoglobin and red blood cells, but also other important changes in the blood, in particular:
- blood color index – less than 0.8;
- average erythrocyte volume – less than 70 µm3;
- the average hemoglobin content in an erythrocyte is less than 24 pg;
- hematocrit – less than 40% for men and less than 35% for women;
- ESR.
If changes are detected in the results of the UAC, a biochemical blood test is prescribed. As a rule, they investigate:
- serum iron level;
- ferritin level;
- total iron-binding capacity of blood serum;
- erythropoietin concentration;
- coefficient of transferrin saturation with iron.
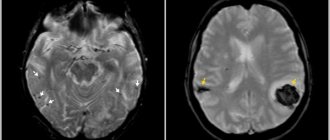
When diagnosing iron deficiency anemia, a search must be made for the reasons that triggered its development. For this purpose the following may be prescribed:
- stool test for the presence of occult blood;
- X-ray examination, which is often carried out using contrast (gastrointestinal tract, chest);
- CT;
- endoscopic examination (esophagogastroduodenoscopy, fibrocolonoscopy);
- Ultrasound of the abdominal organs, kidneys, thyroid gland.
In rare cases, bone marrow puncture examination is performed.
Often in such situations, consultations with specialized specialists involved in the diagnosis and treatment of diseases that provoke the development of IDA are required. This could be an obstetrician-gynecologist, urologist, gastroenterologist, etc.
Why is it important for a doctor to know about this type of anemia?
According to one classification, all anemias are divided into 3 groups:
1) deficiency anemia associated with a lack of iron or vitamins B12/B9; 2) anemia of chronic diseases; 3) hemolytic anemia (including patients with hematological malignancies and conditions associated with bone marrow failure or increased destruction of red blood cells (hemolytic).
Patients from the 1st group are treated, as a rule, by general practitioners, patients from the 3rd group are treated by hematologists, and patients with ACD from the 2nd group are treated by doctors of all specialties - these are patients with oncopathology, infectious-inflammatory and autoimmune diseases.
| In 30–90% of cases, anemia of chronic diseases accompanies long-term tumors, infectious and inflammatory processes, and autoimmune diseases. |
Treatment of iron deficiency anemia
When diagnosing iron deficiency anemia, it is necessary to take a set of measures to replenish iron deficiency, which will lead to improved well-being. In such situations, patients are prescribed iron supplements and diet. But severe anemia may require a red blood cell transfusion.
It is imperative to prescribe treatment for diseases that provoke the development of IDA.
Iron supplements
A course of taking iron supplements is the basis for the treatment of iron deficiency anemia, since it is extremely difficult to compensate for the deficiency of this macroelement only through nutritional correction. In the vast majority of cases, iron supplements are prescribed for oral administration, but in case of malabsorption due to intestinal damage or surgery, they are administered intramuscularly or intravenously. Injections are carried out exclusively in a hospital setting under the constant supervision of medical personnel, since in such cases there is a risk of shock.
For each patient, a drug is individually selected in accordance with his age, the severity of IDA, and the presence of concomitant pathologies. Today there are quite a lot of drugs of this kind, and new drugs that are more advanced regularly enter the pharmaceutical market. Due to the development of technology and a deeper understanding of the course of biochemical reactions, new iron preparations are more effective and safe than those that were synthesized previously. At the same time, the convenience of their use also increases.
Today, the following are most often recommended for the treatment of iron deficiency anemia:
- Nan-O-Fer (Switzerland) – capsules for oral use, created taking into account the peculiarities of iron absorption in the body. It is Nanofer that today is one of the priority drugs for the treatment of IDA, since it contains liposomal iron in the form of pyrophosphate, and in order to improve the quality of its absorption, vitamins B12, B6 and folic acid are added to the drug. This ensures rapid replenishment of iron deficiency with a dose of only 1 capsule per day. Thanks to the special production technology, Nanofer is devoid of side effects typical of other drugs such as constipation, discoloration of teeth, etc., which makes it a first-line drug of choice.
- Totema is a solution for oral use. It is available in dark glass ampoules and contains iron gluconate, copper and manganese. The solution is consumed by dissolving the contents of the ampoule in water. The daily dose for an adult is 2-4 ampoules. At the same time, the finished drink does not have a pleasant taste, which, combined with the frequent development of constipation, abdominal discomfort and the appearance of a metallic taste in the mouth, becomes the reason that patients often voluntarily refuse treatment.
- Sorbifer Durules - tablets for oral administration containing ferrous sulfate and ascorbic acid. Take 2 tablets twice a day half an hour before meals. The drug can also cause digestive problems and a metallic taste in the mouth.
- Maltofer is a line of iron preparations in the form of drops for oral use, syrup and chewable tablets. The daily dose for adults is 1-3 tablets. The disadvantage of these drugs is their high cost and the possibility of developing side effects.
- Ferum Lek is a drug for intravenous administration, although there are also oral forms under this trade name.
All iron supplements are prescribed in a course of 1-5 months, the duration of which is determined by the doctor based on the results of control blood tests.
Thus, the benefits of Nan-O-Fer make it one of the best treatments available today for iron deficiency anemia. Its great advantage is the introduction of iron into the composition in the form of pyrophosphate, as recommended by the Ministry of Health. The recommendation is based on studies that have shown that iron pyrophosphate is absorbed exactly in the amount required by the body. Therefore, its use does not lead to the development of side effects, but at the same time provides complete replenishment of not only mild iron deficiency, but also severe ones. At the same time, the drug Nanofer is affordable, especially in terms of a daily dose.
It is important not to take iron supplements without a doctor’s prescription, since an excess of iron can provoke the development of negative consequences, in particular:
- tooth damage;
- liver damage up to the development of cirrhosis;
- diabetes;
- cardiovascular pathologies;
- severe allergic reactions.
Diet
If iron deficiency anemia is detected, it is important to adjust the diet and introduce foods that contain iron in the most digestible form. This:
- veal and beef, especially liver;
- mutton;
- rabbit meat;
- language;
- egg yolk;
- dog-rose fruit;
- seaweed;
- prunes;
- legumes;
- buckwheat, etc.
It is also recommended to consume foods that are a source of vitamin C during main meals and snacks. These are:
- dog-rose fruit;
- black currant;
- bell pepper;
- parsley;
- broccoli;
- citrus.
Phosphates, phytins and oxalic acid, which are abundant in grains and a number of vegetables, negatively affect the absorption of iron from food and medicines. Tannin present in tea, coffee and cocoa has a similar effect on its absorption.
Red blood cell transfusion
This method is used in the most severe cases when:
- hemoglobin content is less than 70 g/l;
- massive blood loss is observed;
- there is persistent hypotension;
- there is a high risk of complications.
Complications of IDA
With long-term iron deficiency anemia, there is a high risk of complications. Most often they occur after 5 years in the absence of treatment for IDA. By this point, iron deficiency in the body may be so acute that the following may develop:
- damage to the heart muscle, which leads to a decrease in its contractility and the occurrence of heart failure;
- disruption of the immune system, which causes an increase in the incidence of bacterial and viral infections, exacerbation of chronic diseases, in particular sinusitis, tonsillitis;
- liver dysfunction;
- disorders in the reproductive system, which in women often initially manifests itself as disruptions in the menstrual cycle;
- disorders of the nervous system, consisting of irritability, tearfulness, deterioration of memory, attention (with prolonged absence of treatment, IDA, especially when combined with atherosclerosis, diabetes mellitus, sharply increases the likelihood of developing Parkinson's disease, Alzheimer's disease);
- hypoxic coma (occurs in exceptional cases);
- stroke;
- myocardial infarction.
IDA poses a particular danger to children, as it can lead to impairments in intellectual development. Since iron is involved in the production of substances important for the brain, their deficiency leads to decreased memory, concentration and impaired intellectual development in general. In the future, the situation worsens against the background of hypoxia, i.e. oxygen starvation of the brain, against the background of a lack of hemoglobin.
Iron deficiency anemia in pregnant women increases the likelihood of premature birth and disturbances in fetal development.
At the same time, iron deficiency in the body contributes to the worsening of:
- IHD;
- bronchial asthma;
- cerebral ischemia.
Forecast
In most cases of iron deficiency anemia, the therapy provided has excellent results. However, the situation is significantly complicated by the frequent presence of a severe primary disease that causes anemia (most often oncological pathology). In addition, the prognosis of patients with iron deficiency anemia is significantly worsened by diseases of the cardiovascular system.
Iron deficiency anemia is rarely fatal, but severe and moderate cases can cause sufficient hypoxia to aggravate chronic lung and heart disease.
In children, iron deficiency can cause reduced growth rate, reduced IQ and reduced learning ability.