Cerebral amyloid angiopathy
Amyloid angiopathy is a disease of small arterioles with the deposition of protein (amyloid) in the vessel wall, which reduces elasticity and increases the fragility of blood vessels. In this case, microhemorrhages are formed, which are confidently diagnosed on T2*. In addition, this manifests itself in the form of intracerebral hemorrhages with the formation of hematomas in the subcortical areas (lobar hematomas), in contrast to the “typical” hematomas that occur during a hemorrhagic stroke against the background of hypertension with the location of the hematomas in the basal ganglia. This disease occurs mainly in elderly and senile people.
Fig. 1 Cerebral amyloid angiopathy with the presence of small hemorrhages in the cerebral hemispheres (white arrows), as well as traces of previous hemorrhage and lobar hematoma in the left parietal lobe (yellow arrows).
Fig. 2 Blood clot in the left parietal lobe, formed by hemorrhage against the background of amyloid angiopathy (Fig. 2a). Small petecheal hemorrhages in the brain substance, well differentiated on GRE IP (Fig. 2b), Intracerebral acute lobar hematoma in the parietal lobe on the right on CT (Fig. 2c).
Binswanger's disease
Subcortical hypertensive atherosclerotic leukoencephalopathy (Binswanger's disease) is a lesion of the white matter of the brain with widespread gliosis against the background of long-term arterial spasm due to hypertension, cerebral atherosclerosis with chronic cerebral circulatory failure, frequent hypertensive crises, accompanied by encephalopathy and stroke symptoms.
Fig. 3 Diffusely widespread extensive bilateral relatively symmetrical areas of gliosis, located in semi-oval centers, having a hyperintense MR signal on T2 and Flair (Fig. 3a, Fig. 3b), as well as hypodense zones on CT (Fig. 3c).
Causes and prevalence of pathological tortuosity
Pathological tortuosity always develops due to the elongation of the internal carotid artery, which is forced to fold into bends or even loops. Excessive length of the internal carotid artery is often formed during embryonic development, that is, the tortuosity of the artery is most often congenital. With age, further twisting of the redundant carotid artery into a loop may occur. According to some researchers, pathological tortuosity may be the cause of neurological and intellectual problems in children of preschool and primary school age.
Lengthening of the internal carotid artery can also develop as a result of advanced hypertension, when constantly elevated blood pressure causes changes in the artery wall and its bends. Such tortuosity rarely affects cerebral hemodynamics and is more often a phenomenon detected incidentally by ultrasound of the great arteries.
Pathological tortuosity of the carotid arteries was detected in 16% of patients who died from ischemic stroke; more than 23% of children who suffered an ischemic stroke had pathological tortuosity. When examining patients undergoing treatment for cerebrovascular accidents, pathological tortuosity was detected by ultrasound angioscanning in 12%. Various disorders of the internal carotid arteries, according to pathological studies, were identified in 40% of people.
Encephalopathy
Vascular encephalopathy (microangiopathy, chronic cerebral circulatory failure) - the appearance of foci of gliosis on MRI and CT, signs of clinical encephalopathy caused by atherosclerosis of the cerebral arteries, impaired metabolism of fats and carbohydrates, as well as provoked by smoking and arterial hypertension.
Fig. 4 Foci of gliosis in the white matter, located in the centrum semiovale and subcortically, having an increased MR signal in T2 and Flair on MRI (Fig. 4a and Fig. 4b), as well as reduced density on CT (Fig. 4c).
Treatment methods at the Innovative Vascular Center
The vascular surgeons of our clinic have significant experience in unique operations on the carotid arteries with pathological tortuosity. The main problem for surgical treatment is determining clear indications for surgical treatment. Our clinic has developed a clear diagnostic protocol that allows us to determine the clinical significance of a particular tortuosity and the degree of its effect on cerebral blood flow. The experience of successful operations in our clinic for pathological tortuosity exceeds 200 cases.
Cerebral artery stenosis
Fig. 6 Narrowing of the lumen of the arteries, visible by the loss of the MR signal from the projection of the artery section due to a decrease in blood flow velocity against the background of stenosis. Stenosis of the left vertebral artery (arrow in Fig. 6a), stenosis of the supraclinoid segment of the right internal carotid artery (arrows and dotted line in Fig. 6b), as well as stenosis of the basilar artery segment and multiple areas of stenosis of the posterior cerebral arteries (arrows in Fig. .6c).
Symptoms
As mentioned earlier, in the early stages, signs of hypoplasia may be completely absent.
The development of the pathological process can last for years and only when the arterial lumen narrows to a certain value will some symptoms appear. The paradox is that in the complete absence of manifestations of pathology in the early stages, the entry of the disease into the so-called active phase is accompanied by a rich clinical picture. However, in each patient with narrowing of the vertebral artery (right or left), symptoms manifest themselves completely differently:
- Headaches of different nature and specificity. Painful sensations can be periodic or constant, intensify after intense physical activity or occur at rest. With hypoplasia of the cerebral artery, the pain also differs in intensity, from strong, which has to be relieved with analgesics, to weak, which many tolerate without medication. As for the specifics, in most cases we are talking about dull and aching pain, however, they can also be sharp, stabbing.
- Unreasonable dizziness indicates cerebral circulatory disorders. This clinical sign is the second most common and also varies in nature. In some cases, dizziness is not associated with physical exertion, emotional state and other factors; they simply occur more frequently and disappear as quickly as they appeared. In other cases, dizziness begins after a change in body position, any load, stress, etc.
- Often hypoplasia of the right vertebral artery is accompanied by emotional disturbances. A person experiences frequent and sudden changes in mood, depression, which can last up to 2-3 days, then disappear without a trace, constant lethargy, states of apathy and even depressive states.
- If we talk about hypoplasia of the left vertebral artery, this form of the pathological process is more often characterized by changes in blood pressure. Yes, with right-sided hypoplasia they are also present in the clinical picture, but in this case they are noted more often.
- The pathology affects the patient’s body with a state of drowsiness, fatigue, and a feeling of weakness. People with hypoplasia do not get enough sleep even with a full, sound eight-hour sleep, are in a lethargic state, and often yawn.
- The pathology may be accompanied by disorders affecting the vestibular apparatus. In this case, dizziness is also present among the clinical signs, but they become more intense, and are accompanied by nausea, excessive sweating, and changes in skin color (pallor or, conversely, redness of the face). The clearest signs of damage to the vestibular apparatus and the progression of this pathology will be impaired coordination. A loss of balance appears, the gait becomes uncertain, the person sways from side to side, all movements become unclear, and loss of space may develop.
Over time, the symptoms worsen; severe forms of vertebral artery hypoplasia are accompanied by damage to the nervous system. On the one hand, this is expressed in numbness of certain parts of the body (usually limbs), on the other, visual hallucinations. In some cases, partial paralysis even occurs.
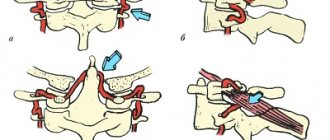
Deviations and bends of the cerebral arteries
Deviations and kinks are common in the extracranial brachiocephalic and vertebral arteries in elderly patients. They can be flat C-shaped, S-shaped, have a bizarre loop or spiral shape (coiling), as well as a bend at an acute angle (kinking). Such bends of the arteries are formed against the background of congenital increased length of the artery, with arteriosclerotic changes, arterial hypertension and changes in the cervical spine against the background of degenerative changes or other pathological conditions leading to a decrease in the height of the neck. Bends of the carotid arteries provoke a decrease in the speed of blood flow, form turbulence in the blood flow and can lead to the deposition of cholesterol with the formation of atherosclerotic plaques and damage to the intima with dissection (dissection).
Fig. 8 Pronounced bilateral S-shaped bends of the internal carotid arteries on T2 in a coronal section (arrows in Fig. 8a). Angiography more clearly demonstrates the presence of an acute bend (kinking) of the extracranial segment of the left internal carotid artery (arrow in Fig. 8b). c-shaped bend of the left vertebral artery (arrow in Fig. 8c).
Causes
Hypoplasia, that is, an anomaly in the development of tissues or an organ, which in this case concerns the vertebral arteries, as mentioned earlier, is a congenital pathology. This means that the main reason for underdevelopment of the artery is problems in the embryonic stages. At the same time, a number of factors can be identified that contribute to the fact that hypoplasia of the vertebral artery occurs in a newborn and manifests itself at a certain age:
- Infectious diseases transmitted by the mother during pregnancy.
- Exposure of the fetus to radiation or ionizing exposure.
- Mechanical injuries, including blows, bruises and other injuries to the abdominal cavity during pregnancy.
- Narrowing of the artery in a newborn can be caused by a genetic predisposition, for example, if the family history includes pathologies of a vascular nature.
- Toxic factor - if during pregnancy a woman smoked, abused alcohol, worked at a chemical plant, or took any potent drugs for a long time, there is a high probability that hypoplasia may be associated with each of these factors.
Venous angioma
Venous dysplasia (angioma) is a congenital vascular malformation in the form of an enlarged dilated vein flowing into the convexital vein or subependymal vein, which in the brain substance breaks up into multiple small venules (looks like a “jellyfish head”), accumulates contrast well and is often located in the subcortical , paraventricular regions, basal ganglia, as well as the cerebellum.
Fig. 9 Venous angioma in the basal ganglia on the right in the form of a hyperdense intracerebral vessel on CT (Fig. 9a), a hyperintense band on T2 (Fig. 9b) and accumulating contrast on T1 after intravenous enhancement (Fig. 9c).
Fig. 10 Weakly hyperdense focus on the axial CT slice - venous angioma (arrow in Fig. 10a) and a hyperdense strip on the coronal section (arrow in Fig. 10b), accumulating contrast after intravenous enhancement with a demonstration of its connection with the internal cerebral and great cerebral vein (arrows in Fig. 10c).
Varicose veins (aneurysm) of the vein of Gallen
Varicose veins of the great cerebral vein (veins of Gallen) are a congenital vascular malformation, often combined with other vascular anomalies, such as dilatation of the straight sinus. The name aneurysm is not entirely suitable for this pathology, since in the context of a vein the interpretation of varicose veins is more acceptable.
Fig. 11 On MRI, varicose veins (aneurysm) of the vein of Gallen have a reduced MR signal on T2 and reduced or isointense on T1 (arrows in Fig. 11a and Fig. 11b). Contrast enhancement is also typical when the cavity of the expanded area is filled with contrast (arrow in Fig. 11c).
Cavernous angioma
Cavernous angioma (cavernoma) is a focus or formation of a vascular nature, congenital in origin (developmental anomaly), which looks like an area surrounded by a ring of hemosiderin and consisting of cavities (cavities) filled with blood plasma. Cavernomas can vary in size from small to giant, and are located in any part of the brain, as well as in the spinal cord. In addition, there may be multiple cavernomas. Complications are not frequent, mainly hemorrhages or bleeding.
Fig. 12 Small cavernoma (formation with a rim of hypointense hemosiderin and a hyperintense center on T2) in the white matter of the right frontal lobe (arrow in Fig. 12a). In the basal ganglia on the right there is a heterogeneous area of slightly hyperdense structure on CT (arrow in Fig. 12b). PI GRE (T2*) or SWI/SWAN has increased sensitivity to cavernous angiomas due to significant susceptibility to hemosiderin derivatives (arrow in Fig. 12c).
Opinion of a specialist, neurosurgeon Andrei Aleksandrovich Zuev:
Some time ago, everyone tried to remove cavernomas, but years later it was proven that the risk of surgery for this formation and the risks of the natural course of the disease are approximately equal. Now only epileptogenic cavernomas and cavernomas with a high risk of bleeding are indications for surgery. The operation, in most cases, is simple if the cavernoma is not localized in the brain stem or in a functionally significant area.
Fig. 13 Cavernoma in the spinal cord with characteristic signs (arrow in Fig. 13a). Native (non-contrast) appearance of a cavernoma on T1 with small dotted areas of increased MR signal (Fig. 13b), weakly accumulating contrast after IV enhancement (Fig. 13c).
Everything about the treatment of hypoplasia of the vertebral arteries
Most diseases affecting the brain are vascular in nature. Hypoplasia is no exception. This is a congenital pathology affecting the intracranial blood supply. The essence of the disease, its symptoms, diagnosis and treatment - this is the subject of research in this article.
Most diseases affecting the brain are vascular in nature. Hypoplasia is no exception. This is a congenital pathology affecting the intracranial blood supply. The essence of the disease, its symptoms, diagnosis and treatment - this is the subject of research in this article.
Diagnostics
It is extremely difficult to identify hypoplasia in the early stages of its development due to the lack of characteristic symptoms and manifestations. There are three main methods for diagnosing narrowing of the lumen of the vertebral arteries, which include:
- Ultrasound examination of the vessels of the head and neck . During the procedure, the image of the artery is recorded using an ultrasound machine, after which the type, intensity and diameter of blood flow is analyzed (a narrowing of the diameter of the vessels to 2 mm or less is considered a serious defect).
- Tomography of the head and neck . Using computer and magnetic resonance imaging, the condition of the vessels filled with a special contrast agent is assessed.
- Angiography . X-ray examination, which reveals abnormalities in the structure of blood vessels and vertebral arteries.
In addition, to diagnose concomitant diseases that may affect the course of hypoplasia (for example, pathology of the cervical vertebrae), the doctor may prescribe additional studies.
- Hypoplasia of the left vertebral artery: what is it, causes and treatment features
At the stage of pronounced clinical symptoms of hypoplasia of the right or left vertebral artery, conservative treatment with vasodilators - they eliminate unpleasant phenomena and improve the patient’s quality of life. In cases where there is a risk of blood clots, taking anticoagulants (blood thinning medications) is indicated.
When is vertebral artery hypoplasia diagnosed?
It is in the intracranial segment that pathological narrowing of the vertebral arteries is most often observed. The diameter of these great vessels is uneven along the entire length and ranges from the smallest value - 2 mm, to a lumen of 4.5 mm. The normal diameter of the PA usually ranges from 3.5 to 4 mm.
Hypoplasia of the vertebral artery is considered to be its critical narrowing of up to two millimeters. Congenital breakage or complete absence of one of the branches is also possible - this pathology is called aplasia.
- Incorrect position of the fetus in the womb, due to which it is exposed to unwanted mechanical stress.
- Carrying a pregnancy to term under negative conditions that negatively affect the development of the embryo: maternal use of alcohol, drugs, smoking;
- finding the future woman in labor in a hazardous environment (working in a chemical production facility, living in a gas-polluted or radioactive area);
- infectious pathologies, injuries, medication, intoxication, poisoning during pregnancy.
Barre-Lieu syndrome
A classic sign of a malnutrition of the occipital lobe of the brain. Gives headache, nausea, and rarely vomiting.
Orientation in space also decreases, pathological fatigue and fatigue are detected.
Insomnia, depressive mood, constant depression, apathy and reluctance to do anything.
Hypoplasia of the vertebral artery: what is it?
One of the most common pathologies of the vertebral arteries is their hypoplasia, that is, underdevelopment. This anomaly manifests itself as a significant narrowing of the lumen of the vessel (it becomes less than 2 mm). The left vertebral artery is affected more often than the right. Hypoplasia occurs in utero - this is a congenital pathology. Various factors can provoke the appearance of the disease in question:
- Bad habits of the expectant mother.
- A woman's use of dangerous drugs in early pregnancy.
- Intrauterine infection of the embryo.
- Effect of radiation on pregnant women.
It is also worth noting that quite often hypoplasia is found in children who do not have a history of any of the listed factors.
Treatment methods
To treat hypoplasia of the vertebral arteries, methods of conservative therapy and surgical treatment are used.
To treat hypoplasia of the vertebral arteries, methods of conservative therapy and surgical treatment are used.
- What is hypoplasia of the right or left vertebral arteries, how to treat this disease?
Diagnosis of hypoplasia of the vertebral artery of the brain
With hypoplasia of the vertebral artery of the brain, typical clinical symptoms are present, which are a direct indication for a number of clinical studies. Typically diagnosis includes:
- X-ray of the cervical spine;
- MRI of brain structures;
- duplex scanning of cerebral blood vessels;
- angiography with the introduction of a contrast agent.
It is worth paying attention to the following negative manifestations of the disease:
Anatomical variants of cerebral arteries
Anatomical variations in the course of the cerebral arteries and the structure of the circle of Willis are due to the variant diversity and manifestation of structural features. The most common variants can be in the form of underdevelopment (aplasia) or underdevelopment (hypoplasia) of any artery, as well as the appearance of an additional (supernumerary) artery and variants of arterial fusion. In this case, it may be difficult to separate the developmental anomaly and the anatomical variant of the norm. Some variations and anomalies are presented below.
Fig. 14 Hypoplasia of the proximal segment (A1) of the right anterior cerebral artery (arrow in Fig. 14a), in which both distal segments (A2) of the ACA are a continuation of the proximal left ACA from the basin of the left internal carotid artery, this option is called incomplete anterior trifurcation of the left internal carotid artery. Apoplasia of the proximal segment (A1) of the right ACA (arrow and dotted line in Fig. 14b), in which both distal segments (A2) of the ACA are a continuation of only the proximal (A1) left ACA from the basin of the left ICA, this option is called complete anterior trifurcation of the left ICA . In Fig. 11c there is a pronounced asymmetry in the diameter of the vertebral arteries (S>D) - hypoplasia of the right vertebral artery (arrow in Fig. 14c).
Fig. 15 The left posterior cerebral artery is a complete continuation of the left posterior communicating artery from the basin of the left ICA, with complete aplasia of the proximal segment (P1) of the left posterior cerebral artery (PCA) - an anatomical variant of the circle of Willis in the form of the so-called posterior trifurcation of the left internal carotid artery ( arrows in Fig. 15a). Bilateral hypoplasia of the vertebral arteries, predominantly expressed on the left (arrows in Fig. 15b). Fenestration of the basilar artery in the form of the presence of a “window” with local short-term doubling of the basilar artery or premature fusion of the basilar arteries with subsequent splitting (arrow in Fig. 15c).
Fig. 16 There is unilateral aplasia of the left posterior communicating artery (dotted line in Fig. 16a), with a normally developed opposite PCA and anterior communicating artery (ACA) (arrows in Fig. 16a). Bilateral hypoplasia of the proximal posterior cerebral arteries (P1) (arrows in Fig. 16b) with incomplete bilateral posterior trifurcation of the PCA, as well as hypoplasia of the left vertebral artery (dotted line in Fig. 16b). There is no fusion of the left vertebral artery (arrow in Fig. 16c) with the right VA, while the left vertebral artery remains a separate vessel, completely passing into the left posterior inferior cerebellar artery.
Fig. 17 Unilateral hypoplasia of the proximal segment (P1) of the left PCA (arrow in Fig. 17a) with the presence of incomplete (partial) posterior trifurcation of the left ICA. There is an accessory anterior cerebral artery (postcommunicative semgent - P2), which arises from the middle of the anterior communicating artery (ACA) (arrow in Fig. 17b). The hypoplastic right VA completely passes into the right posterior inferior cerebellar artery (arrow in Fig. 17c), without merging with the left VA, which is hyperplastic and entirely continues into the main artery, without a clear anatomical boundary between the VA and OA.
International Neurological Journal 3 (57) 2013
Objective: to evaluate the role of cerebral artery (CA) anomalies in the development of cerebral ischemic stroke (CI) in young patients.
Materials and methods of research. We examined 143 patients with diagnosed CI, among whom 67 (46.9%) had CA anomalies (men - 29, women - 38), the age of the patients was from 19 to 50 years (average age - 37.7 ± 1.2 years ). All patients underwent a comprehensive examination, including clinical-neurological, clinical-laboratory and clinical-instrumental studies.
Results. In 46.9% of patients included in the study, anomalies of the CA were identified according to brain MRI angiography. Anomalies of intracerebral arteries (ICA) were diagnosed in 38 (56.7%), anomalies of precerebral arteries (ACA) - in 53 (79.1%) patients with CI, and their combination - in 38 (56.7%) patients. Cerebral circulation was assessed using transcranial duplex scanning of the vessels of the base of the brain and Doppler ultrasound of the vessels of the neck.
All patients with ICA and PCA anomalies showed a decrease in cerebral collateral blood flow. The most significant hemodynamic changes were found in patients with aplasia of the posterior communicating artery (PCA), hypoplasia of the anterior and posterior cerebral arteries (PCA), and in combinations with posterior trifurcation of the left internal carotid artery (ICA). Pathological tortuosity of the ICA was detected in 42 (79.2%) patients: one - in 29 (69%), both ICAs - in 14 (33.3%), S-shaped tortuosity - in 31 (73.8%), loop-shaped - in 11 (26.2%), hypoplasia of both vertebral arteries (VA) - in 24 (57.1%), aplasia of one VA - in 7 (16.7%) patients. ICA tortuosity was considered pathological if local hemodynamic disturbances in the form of turbulence and expansion of the Doppler frequency spectrum were recorded at the site of maximum angulation. Hypoperfusion was found in 37 (55.2%) patients: with aplasia of the PCA - in 7 (16.7%), one PA - in 7 (16.7%), hypoplasia of the PCA - in 23 (62.1%) patients.
Conclusions. A high incidence of CA anomalies was revealed in 46.9% of young people who underwent CI. Among ICA anomalies, the most common (in 56.7% of cases) was separation of the circle of Willis, due to the absence of one or both connecting arteries. When examining the PCA, it was found that they were affected in 79.1% of cases—pathological tortuosity of the ICA. When carrying out ultrasound research methods, a decrease in blood flow velocity, asymmetry of blood flow in the CA and hyperperfusion in pathologically tortuous and hypoplastic vessels were revealed, which indicates the presence of focal hypoperfusion in areas with inadequate circulation and a deficiency of collateral blood flow at the border of the blood supply basins of the brain.
Anatomical variants of cerebral veins
Fig. 19 Reduced blood flow through the superior sagittal sinus due to its hypoplasia (Fig. 19a). Aplasia of the right transverse sinus (dashed line in Fig. 19b) with compensatory overdeveloped occipital and right petrosal sinuses (arrows in Fig. 19). High location of the jugular vein bulb with its location above the level of the foramen lacerum, in which it creates an asymmetrical picture and creates a false impression of the presence of a formation (arrow in Fig. 19c).
Neurovascular conflict
Neurovascular conflict is a pathological interaction between an artery and a nerve, most often manifested in the area of the cerebellopontine angle in the form of a violation of the anatomical relationship between the VII and/or VIII pair of cranial nerves and the VA or branch of the OA. In this case, there may be no dislocation of the nerve by the artery, or otherwise, dislocation of the nerve by the artery is not always clinically manifested by neurological symptoms.
Fig. 21 The VA is dislocated (white arrow in Fig. 21a) and stretches the left vestibulocochlear nerve (black arrow in Fig. 21a). MRA shows the PA dislocation to the left (arrow in Fig. 21b). The close location of the artery and nerve in the region of the right cerebellopontine angle (MCA) (arrow in Fig. 21c).
The issues of prevention and treatment of osteochondrosis (OCS) of the spine are gaining special weight due to the progression of the number of patients in all countries of the world, its significant share in the structure of morbidity, disability and disability of the population. One of the leading clinical symptoms of OSC of the cervical spine (CSP) is ) appears to be vertebral artery syndrome (VA), which may have many pathogenetic mechanisms of formation. In ICD-10 there are several diagnoses that define damage to the vertebrobasilar region (VBB): M 47.0 – VA compression syndrome in spondylosis; M 53.0 – posterior cervical sympathetic syndrome; G 45.0 – syndrome of the vertebrobasilar arterial system. In recent years, the topics of diagnosis and treatment of PA syndrome have attracted increasing interest from doctors of many specialties: neurologists, neurosurgeons, vertebrologists, angiosurgeons, therapists, general practitioners, chiropractors, physiotherapists. Anatomy of PA . In order to present the pathogenesis of the formation of PA syndrome, it is necessary to have an understanding of the anatomy of this vessel. The PA supplies blood to a large area: segments of the spinal cord from C1 to Th3, including (superior medullary arterial basin), inner ear, brain stem structures (BS), occipital lobes, mediobasal areas of the temporal lobes, cerebellum, dorsal parts of the hypothalamic region. From the stellate ganglion, formed by the sympathetic centers of the C3–Th1 segments of the spinal cord, the spinal nerve emerges (posterior cervical sympathicus or Frank’s nerve). It penetrates the canal of the transverse processes, wrapping its branches around the PA. Additionally, branches depart from the vertebral nerve that take part in the formation of the Luschka nerve. This nerve innervates the capsular-ligamentous apparatus of the spine, the periosteum of the vertebrae and the posterior part of the intervertebral discs (IVD). A large proportion of the extracranial segment of the VA passes through the mobile bone canal formed by the transverse processes of the vertebrae. Moreover, the medial wall of the VA is adjacent to the uncovertebral joint, and the posterior wall borders the superior articular process. At the C1-C2 level, the VA is covered only by soft tissue, mainly by the inferior oblique muscle of the capitis. Etiology and pathogenesis . Some clinicians explain the clinical picture of PA syndrome in the case of spinal cord syndrome by compression of this vessel by bone growths of the vertebrae. This theory is based on multiple cases of traumatic injury to the VA or their ligation, followed by stroke in the VBB. However, further experimental and clinical studies have shown that compression of the VA alone cannot cause failure in the VSP. Only with congenital or acquired pathology of the VA (aplasia, abnormal narrowness, atherosclerosis, compression by osteophytes, hemodynamically significant stenotic lesions in the area of the VA orifices, occlusion of one of the VAs, vertebral-subclavian steal syndrome, etc.) can clinical failure of the compressed VA appear. The leading mechanism for the formation of VA compression syndrome seems to be extravascular edema due to mechanical compression, which leads to disruption of venous blood flow. Compression of the veins in the bone canal of the transverse processes of the spinal cord occurs earlier than the arterial one, and the venous outflow formed from compression of the veins in the bone canal aggravates the compression of the VA. Long-term irritation of the sympathetic plexus has been well studied in OSCC. Pathological irritation of this plexus during OSCC of the cervical spine causes spasm of the vessels of the VA system, which is clinically manifested by the dysfunction of the parts of the brain they supply with blood. The irritative type of PA syndrome is mainly recorded in young patients who do not have concomitant VBD pathology.
The etiological causes of PA syndrome can be divided into 3 types:
- Occlusive pathology of VA (atherosclerosis, thrombosis, embolism, arteritis).
- PA deformation (pathological tortuosity and deformation).
- Extravasal compression of the VA (compression by bone anomalies, ribs, muscles, IVD hernias, osteophytes and articular processes of the cervical vertebrae, scars, tumors, etc.).
According to various researchers, mechanical effects can cause PA:
1) bone growths of uncovertebral joints in 55.9% of cases;
2) bone growths of the facet joints (DOS) with spondyloarthrosis - 6.0%;
3) anterior-superior angle of the articular process with subluxation during extension (according to Kovach) in the spine - 25.0%;
4) anterior scalene muscle with a combination of scalenus syndrome with lateral origin of the VA orifice - 7.1%;
5) lateral hernia of the IVD, emerging through the uncovertebral fissure - 6.0%;
6) compression in the atlas region (Klippel-Feil anomalies, Kimmerli anomalies, platybasia);
Clinical picture . PA syndrome is clinically reflected by paroxysmal cephalgia (migraine type), dizziness, ataxia, nausea and/or vomiting, visual and auditory disorders, drop-attack episodes, syncope and hypothalamic attacks. Visual disturbances include the following: darkening in the eyes, a feeling of sand, sparks and other expressions of photopsia, slight changes in the tone of the fundus vessels (recorded in every 4-5 patients). Memory loss is more pathognomonic for individuals with pronounced organic changes. In approximately 60.0% of individuals, the syndrome is associated with certain movements or positions of the spinal cord, accompanied by an increase in VA compression. Of great importance in the formation of the clinical picture of PA syndrome is also concomitant pathology, such as atherosclerosis of the brachiocephalic arteries and cerebral arteries, arterial hypertension, coronary heart disease, etc. The diagnosis of PA syndrome is given to individuals who have a certain range of complaints and clinical syndromes that can be associated with OSCC or SHOP anomalies. Clinical variants of PA syndrome:
Barre-Lieu syndrome (posterior cervical sympathetic syndrome) . In most episodes, this syndrome is caused by arthrosis of the uncovertebral joints and subluxations according to Kovacs in the SHOP. Pain syndrome is associated with an earlier development of OSCC and pathological mobility in the cervical spine. It is characterized by cephalgia in the cervical-occipital region with spread to the front of the head (like “removing the helmet”). Cephalgia is combined with autonomic, cochleovestibular and visual disturbances.
Basilar migraine. It is characterized by visual disturbances on both sides, combined with dizziness, ataxia, dysarthria, and tinnitus. At the height of paroxysm, intense pain develops in the occipital region, combined with vomiting and, in some cases, loss of consciousness.
Vestibulo-atactic syndrome. Dizziness, a feeling of unsteadiness of the body, darkening of the eyes, imbalance with nausea and vomiting prevail. Symptoms progress when moving to the shopping center.
Cochleovestibular syndrome. It appears as noise in the ears or the back of the head, paresthesia, hearing loss, decreased perception of whispers, changes in the audiogram. These disorders are mainly combined with periodic non-systemic dizziness (a feeling of unsteadiness and staggering) or systemic dizziness.
Ophthalmic syndrome. Visual disorders are characterized by paroxysmal photopsia, atrial scotoma, fatigue and decreased vision when reading and other visual stress. Signs of conjunctivitis may be recorded: pain and a feeling of a foreign body in the eyes, redness of the conjunctiva, lacrimation. Cases of paroxysmal loss of visual fields are also recorded, often associated with the position in the SHOP.
Syndrome of autonomic disorders. The following vegetative symptoms are most often recorded: feeling of heat, chills, cold extremities, hyperhidrosis, changes in dermographism. Laryngopharyngeal disorders, as well as recurrent sleep and wakefulness disturbances, may occur.
Dropp-attack attacks . An episode of an unexpected fall is associated with ischemia of the caudal parts of the brainstem and cerebellum and appears in the form of tetraplegia with sudden extension in the spinal cord with rapid restoration of motor function.
Transient ischemic attacks.
Unterharnscheidt syndrome (syncopeal vertebrogenic syndrome) . It represents stroke in the reticular formation of the brainstem trunk, characterized by a short-term switching off of consciousness during rapid movement in the cervical spine or a prolonged forced position.
Diagnostics. To identify vertebrogenic PA syndrome, the presence of 3 clinical diagnostic criteria is necessary:
1. Clinical picture (presence of one of the nine clinical options described above or their combination).
2. The presence of changes diagnosed during MRI or CT in combination with functional spondylography of the spine (spondylosis in the area of uncovertebral joints, arthrosis of the joint joint, subluxation of the articular processes, instability and hypermobility in the spine, lateral hernias of the IVD, anomalies of the bone bed of the VA, craniovertebral junction, etc. .).
3. The presence of changes diagnosed when performing duplex scanning of the VA and/or when performing Dopplerography using functional tests with rotation, flexion and extension in the cervical spine (compression of the VA, asymmetry of the linear velocity of blood flow in the VA, vasospastic reactions in the VA and basilar arteries, hyperreactivity for functional tests, change in PA diameter).
Treatment. Conservative treatment includes: manual therapy, massage, acupuncture, physiotherapy, and spa treatment. According to modern understanding, neuroprotection is a complex of drug therapy aimed at compensating for the developing energy deficit of neurons, protecting them from the influence of damaging factors, activating neuroregeneration processes, and correcting blood flow in the brain. In PA syndrome, neuroprotection seems to be one of the most effective methods for preventing chronic cerebral ischemia, expressed as insufficiency in the VBB. The administration of neuroprotectors helps prevent the formation of metabolic disorders of the brain in individuals with an increased risk of ischemia, especially with a decrease in cerebrovascular reserve. Neuroprotection has the leading value in people with symptomatic stages of PA syndrome - stroke, transient ischemic attacks, syncopal vertebrogenic syndrome, dropp-attack attacks.
Rules for drug treatment of PA syndrome:
1. Drugs acting on venous outflow: semisynthetic diosmin (detralex, phlebodia), troxerutin, ginkgo biloba.
2. Nonsteroidal anti-inflammatory drugs: nimesulide, lornoxicam, celecoxib, Celebrex.
3. Drugs that normalize blood flow in the PA: pentoxifylline, vincamine, vinpocetine, cinnarizine, nimodipine, nicergoline, sermion, instenon.
4. Cholinergic drugs: citicoline, ceraxone, recognan, gliatilin.
5. Complex neuroprotective drugs: cytoflavin, actovegin, cerebrolysin, piracetam, mexidol
6.Metabolic therapy: cytoflavin, mildronate, thiotriazoline, trimetazidine
7. Symptomatic therapy - muscle relaxants: tolperisone, antispasmodics: drotaverine, histamine-like: betahistine, antimigraine: sumatriptan.
Complex conservative treatment includes orthopedic interventions on the source of pathology (cervical spine traction, cervical spine immobilization, manual therapy, etc.); novocaine blockade of spastically contracted and painful muscles of the spinal cord; physiotherapeutic and balneological methods.
Therefore, in the treatment of patients with PA syndrome, along with traditional conservative therapy, puncture methods of influence should be used: blockade of the PA, stellate ganglion, inferior oblique muscle of the head, dereception of the IVD and DOS.
Novocaine blockade of the sympathetic plexus of the PA is both diagnostic and therapeutic. The course includes 4-5 blockades at intervals every other day. The blockade technique is as follows: the patient was placed on his back with a bolster under his shoulders. Using the index finger of the left hand, push the carotid artery laterally, penetrating between it and the middle organs of the neck. The carotid tubercle of the transverse process of C6 is identified. After piercing the skin with a needle, they rest against the indicated tubercle, then, sliding off it, the needle falls through the intertransverse muscle, i.e., into the PA canal. An aspiration test ensures that there is no damage to the vessel. Then 3-5 ml of a 2% novocaine solution is injected. After performing the manipulation, the patient should lie on his back for 20 minutes so that the anesthetic does not spread through the perineural spaces to the stellate ganglion.
At the same time, with pathological impulses from the affected DOS, a persistent or intermittent spasm of the VA occurs. The main advantage of chemical denervation of the DOS over more local influences (laser vaporization, cold plasma coblation, high-frequency destruction) is that the alcohol-vocaine solution turns off a larger number of nociceptive vegetative structures around the DOS, including branches of the Luschka nerve, which play a major role in the formation of reflex syndromes facet syndrome SHOP.
The first minimally invasive methods were chemonucleolysis, IVD dereception and percutaneous nucleotomy. Chemonnucleolysis and dereception of the IVD lead to the development of fibrosis of the nucleus pulposus of the IVD with the creation of conditions for ankylosis of the spinal motor segment at various stages of its dystrophic lesion. The development of fibrosis of the IVD limits the range of movements in the operated segment, while the minimum range of movements that does not lead to local overload of adjacent spinal motion segments is not excluded. The process of IVD restructuring after chemonucleolysis is long and takes 1.5-2 years, which can lead to the development of relapse of the disease.
For vertebrogenic PA syndrome, the following operations are performed:
- decompressive and stabilizing - uncusectomy with ventral interbody fusion;
- decompressive-plastic - transdiscal decompression of the VA;
- decompressive - extradiscal uncusectomy and arteriolysis, resection of abnormal rings of the C1 vertebra, resection of the cervical rib and arteriolysis, etc.;
- stabilizing operations for dynamic compression of the VA;
- laser vaporization of IVD for reflex syndrome of PA and IVD protrusion.
A distinctive feature of surgical treatment of persons with VA syndrome is determined by the frequent combinations of vertebrogenic lesions of the VA with their atherosclerotic or congenital pathology (32.0% of patients), as well as with occlusive and stenotic lesions of the carotid arteries (26.7-28.0%). This indicates the need for precise preoperative examination of these individuals and comprehensive treatment. In patients with combined lesions of the VA and carotid arteries, the first stage is reconstruction of the carotid system.
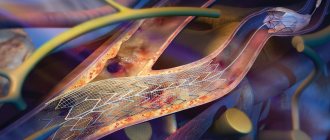
Reconstruction of V1 VA is advisable to apply with intact distal segments (V2-4). When identifying atherosclerotic lesions of the VA in the V1 segment, the following reconstructive operations are performed:
- transposition of the VA into the internal carotid artery;
- transposition of the VA into the common carotid artery;
- transposition of the VA into the subclavian artery;
- transposition of the VA into the thyrocervical trunk;
- modified transposition (replantation) of the VA mouth;
- endarterectomy and angioplasty of VA;
- arteriolysis and desympathization of PA.
Indications for VA reconstruction in the V3 segment:
1) stenosis or occlusion of the V1 and V2 segments of the VA with an open circle of Willis;
2) extravasal compression of the V2 segment of the VA with an open circle of Willis;
3) upcoming reconstruction on the V1 segment of the VA or carotid-subclavian anastomosis;
4) stent fracture or severe restenosis (if repeated stenting is not possible) after stenting of the V1 segment of the VA.
Access to the V3 segment of the VA (between the transverse processes of C1-2) has several advantages: the location of the VA in this area is the most superficial, the ability to perform dissection of the VA without bone resection at a prolonged distance, and the venous plexus in this area is less pronounced than in others.
In case of atherosclerotic lesions of the VA in the V3 segment, the following reconstructive operations are performed:
- transposition of the VA into the internal carotid artery;
- general-distal spinal bypass surgery;
- external carotid-distal spinal shunting;
- intracarotid-distal spinal shunting;
- external carotid-distal spinal anastomosis;
- occipito-distal spinal anastomosis;
- subclavian-distal vertebral bypass surgery.
Conclusion. The clinical picture of PA syndrome does not always have a classic picture, and the most stable signs are cephalalgia, dizziness and tinnitus. The effectiveness of treatment of PA syndrome is inextricably linked with the timely diagnosis of this disease. A comprehensive impact on the possible pathogenetic mechanisms of the formation of PA syndrome is necessary. Conservative treatment of people with PA syndrome can reduce the severity and frequency of clinical symptoms. Minimally invasive methods of treating PA syndrome should take their rightful place in the arsenal of a vertebrologist, neurosurgeon and neurologist. Reconstructive operations on VA for atherosclerotic lesions in specialized departments (vascular surgery and neurosurgery) should also be more widely used. There is also a need for greater awareness among primary care physicians about this disease and how to diagnose and treat it.
Pachionian granulations
Fig. 22 Pachionian granulation in the lumen of the transverse sinus on the right (arrow in Fig. 22a), which can simulate a thrombus, but unlike it, granulation has a hyperintense MR signal on T2. Traces of the presence of expanded pachyonic granulations on the internal plate and in the diploea of the occipital bone on CT in the bone window (arrows in Fig. 22b) and the brain window (arrow in Fig. 22c).
Subarachnoid hemorrhage
Non-traumatic subarachnoid hemorrhage occurs in most cases due to rupture of a cerebral artery aneurysm, less often due to bleeding from a vascular malformation or AV fistula.
Non-traumatic subarachnoid hemorrhage secondary to aneurysm rupture
Fig. 23 Rupture of an anterior cerebral-anterior communicating artery (ACA-ACA) aneurysm, localized by the presence of a small hematoma in the area of the aneurysm rupture (yellow arrow in Fig. 23) with the presence of massive hemorrhage in the subarachnoid space (Fisher IV) (white arrows in Fig. .23a). Blood in SAH differentiates in the subarachnoid space of the SAP and inside the ventricular cavities (arrows in Fig. 23b and Fig. 23c).
The book “Brain Tumors. CT and MRI diagnostics” read, view / order
Author: radiologist, Ph.D. Vlasov Evgeniy Alexandrovich
Full or partial reprint of this article is permitted by installing an active hyperlink to the source
- you have lost the description of your MRI or CT scan,
- The doctor was not satisfied with the description of your MRI or CT scan
- you doubt the conclusions based on your MRI results,
You can order a review of your MRI or CT scan with a detailed transcript here:
Classification of variants of arteries and variants of the arterial circle of the human brain
The characteristics of the structure of the arteries of the human brain have been known for a long time. In fact, T. Willis (1664), having described for the first time a typical arterial anastomosis, began the scientific chronicle of variations in the structure and topography of the arteries of the human brain. Since the 19th century the characteristics of the variants of the structure of the arterial bed of the brain began to be of a systemic nature, and numerous authors began to consider the Circle of Willis not only as an anastomosis consisting of individual arteries, but as a single arterial circle of the cerebrum.
Anastomoses of the arterial circle of the cerebrum (ACCA) are more often observed in the child’s brain; with age, their number decreases. Variants of the structure of the ABM are reduced to three main groups: 1) open variants of the circle - its front and rear semi-rings; 2) variants of atypical origin of cerebral arteries; 3) options with an asymmetrical diameter of the vessels of the right and left parts of the circle. It is important to remember that the identification of arteries as a variant or anomaly depends, among other things, on imaging capabilities. There are types of branching of the internal carotid artery (ICA): fetal, transitional, anterior trifurcation, posterior trifurcation. The following variants of the ACBM structure are of greatest importance during operations: partial and complete anterior trifurcation of the ICA; partial and complete posterior trifurcation of the ICA; partial and complete quadrifurcation of the ICA; aplasia of the posterior communicating artery (PCA).
The classic anatomical or “typical” structure of the arterial bed of the human brain is quite clearly reflected in the “International Anatomical Terminology”. Among the significant attempts to classify variants of the structure and topography of the arterial bed of the brain, taking into account individual arteries from well-known classical and modern literary sources and available Internet resources, perhaps only the classification of R.M. Belenkaya (1979). However, taking into account the knowledge accumulated over the past 40 years, an updated approach to the assessment and interpretation of variations in the structure and topography of both individual arteries and the arterial bed of the brain as a whole is needed. In this regard, we propose for consideration a classification that, on the one hand, distinguishes between simpler and more complex variants of structure and topography, and on the other, more systematically characterizing the morphology of the arterial bed of the brain.
So, the options for the structure and topography of the arterial bed of the human brain are quite numerous and diverse. The very concept of “variant of the structure and topography of the arterial bed of the brain” combines both features of the structure and/or topography of one vessel that differ from generally accepted concepts, and features of the structure and/or topography of two or more vessels simultaneously. In order to distinguish between options according to the degree of complexity, we consider it advisable to introduce the elementary concept of “the phenomenon of the structure and topography of a cerebral artery.” From our point of view, the “phenomenon of the structure and topography of a cerebral artery” should be understood as features of the structure or topography of one vessel, or sometimes two (with the participation of both arteries in the substrate of the phenomenon), that differ from generally accepted ideas. The presence of one or a combination of two or more phenomena forms the actual “variant of the structure and topography of the arterial bed of the brain.”
We have universalized all variants of human cerebral arteries that we found in the available literature into the following sets:
- options for the structure and topography of individual arteries of the brain (options for the structure and topography of each artery separately are considered);
- variants of the structure and topography of the anterior part of the arterial circle of the cerebrum (variants of the structure and topography of two or more arteries of the anterior part of the arterial circle of the cerebrum are considered);
- options for the structure and topography of the posterior part of the arterial circle of the cerebrum (variants of the structure and topography of two or more arteries of the posterior part of the arterial circle of the cerebrum and intracranial parts of the vertebral arteries are considered);
- variants of the arterial circle of the cerebrum as a whole.
According to the magnetic resonance angiography (MRA) data we obtained, the typical structure of the arterial bed of the brain was identified in 166 (51.6%) of 322 practically healthy individuals, and variations in the structure and topography of individual arteries of the brain, the anterior part of the arterial circle of the cerebrum, the posterior part of the arterial circle of the cerebrum and the arterial circle of the cerebrum as a whole were identified in 156 (48.4%) of 322 practically healthy individuals.
According to MRA of the brain, from the phenomena of the structure and topography of the ICA, hypoplasia of the ICA was verified in 2 (1.3%) patients out of 156 practically healthy people. The following phenomena of the structure and topography of the anterior cerebral arteries (ACA) were verified: anterior trifurcation of the ICA in 3 (1.9%), hypoplasia of the ACA in 2 (1.3%), as well as a combination of two phenomena of the structure and topography of the ACA: bending of both ACAs in 3 (1.9%) people. The phenomena of the structure and topography of the anterior communicating artery have not been verified. The phenomena of the structure and topography of the middle cerebral artery have not been verified. Of the structural and PCA phenomena, hypoplasia of one or both PCAs was verified in 7 (4.4%) patients. The following phenomena of the structure and topography of the posterior cerebral arteries (PCA) were verified: posterior trifurcation of the ICA in 8 (5.1%) patients, deviation of the PCA in 1 (0.6%) patient, hypoplasia of the PCA in 1 (0.6%) patient, as well as a combination of two phenomena of the structure and topography of the PCA: posterior trifurcation of the ICA and curvature of the PCA in 10 (6.3%) patients, posterior trifurcation of both ICAs partial and complete in 3 (1.9%) patients, bends of both PCAs in 1 (0 .6%) of the patient. The following phenomena of the structure and topography of the basilar artery (BA) were revealed: BA deviation in 7 (4.5%) patients, BA bending in 5 (3.2%) patients, BA tortuosity in 3 (1.9%) patients, doubling ( non-fusion) BA in 3 (1.9%) patients, BA bifurcation in 1 (0.6%) patient, as well as a combination of two phenomena of the structure and topography of the basilar artery: BA deviation and BA bending in 7 people (2.1%) out of 156 practically healthy people. The following phenomena of the structure and topography of the intracranial parts of the vertebral arteries (ICVA) were verified: hypoplasia of one of the VCPA in 17 people (10.9%), excessive tortuosity of one of the VCPA in 1 (0.6%) patient, S-shaped VCPA in 1 ( 0.6%) of the patient, as well as a combination of two phenomena of the structure and topography of the ICPA: tortuosity and hypoplasia of one HCPA in 4 (2.7%) patients, hypoplasia of both HCPA in 2 (1.3%) patients, tortuosity of both HCPA in 9 (5.8%) patients, as well as a combination of four phenomena of the structure and topography of the ICPA was identified in 3 (1.9%) people: hypoplasia and tortuosity of both HCPA.
We verified the following variants of the structure and topography of the anterior part of the ACBM from 156 practically healthy people:
- hypoplasia of both ICAs and hypoplasia of the PCA in 2 (1.3%) patients;
- hypoplasia of both PCA and hypoplasia of the ACA in 1 (0.6%) patient;
- anterior trifurcation of the ICA, tortuosity and hypoplasia of both MCAs, hypoplasia of the basilar artery.
Variants of the posterior part of the ACBM were verified from 156 practically healthy people:
- hypoplasia of one PCA and bending of the BA in 1 (0.6%) patient;
- hypoplasia of one HFPA and hypoplasia of one PCA in 2 (1.3%) patients;
- hypoplasia of both ICPA and hypoplasia of the PCA in 1 (0.6%) patient;
- hypoplasia of both PCAs and deviation of the BA in 2 (1.3%) patients.
AKBM variants as a whole have been verified:
- hypoplasia of the ACA and hypoplasia of both PCAs in 3 (1.8%) patients;
- anterior trifurcation of the internal carotid artery and curvature of the posterior cerebral artery in 2 (1.3%) patients;
- PCA deviation and PCA hypoplasia in 3 (1.9%) patients;
- hypoplasia of both PCAs and deviation of the BA in 1 (0.6%) patient;
- posterior trifurcation of both ICAs and hypoplasia of both ICAs in 2 (1.3%) people;
- hypoplasia of both PCAs and hypoplasia of the ICPA on one side in 2 (1.3%) people;
- posterior trifurcation of the ICA and hypoplasia of the ICA on one side in 1 (0.6%) patient;
- posterior trifurcation of both ICAs and angulation of the BA in 6 (3.9%) patients;
- hypoplasia of both PCA and hypoplasia of the BA in 3 (1.9%) patients;
- hypoplasia of both PCAs and hypoplasia of both ICPAs in 2 (1.3%) patients;
- posterior trifurcation of the ICA and hypoplasia of both ICAs in 2 (1.3%) patients;
- ACA hypoplasia and HFPA hypoplasia in 5 (3.2%) patients;
- ACA hypoplasia and BA deviation in 4 (2.6%) patients;
- hypoplasia of the ACA and tortuosity of both ICPA in 4 (2.6%) patients;
- anterior trifurcation of the ICA, posterior trifurcation of the ICA and S-shaped BA in 3 (1.9%) patients;
- hypoplasia of both PCAs and deviation of both ICAs in 1 (0.6%) patient;
- hypoplasia of the PCA and S-shaped BA in 2 (1.3%) patients
Thus, among the variants of ACBM, 24 phenomena of the structure and topography of the cerebral arteries were verified, the combination of which determined 49 variants of the cerebral arteries. All identified phenomena of the structure and topography of the arterial bed of the brain, the totality of which makes it possible to systematize and clarify the number of structural variants in close relationship with each other, create a critical need to reflect them in a classification scheme.
- Variants of the structure, topography and branches of individual arteries of the brain (variants of each artery are considered separately).
- Variants of the structure and topography of the arterial circle of the cerebrum (variants of two or more ACBM and VCPA are considered):
- options for the structure and topography of the front part of the battery;
- variants of the structure and topography of the posterior part of the ACBM and variants of the intracranial parts of the vertebral arteries;
- variants of the structure and topography of the arterial circle of the cerebrum as a whole and variants of the intracranial parts of the vertebral arteries.
- Atypical and abnormal (including so-called persistent embryonic anastomoses) arteries as variants of the structure and topography of the arterial bed of the brain.
- Notes:
- a variant of the structure and topography is represented by one phenomenon or a set) of phenomena of the structure and topography of an artery or arteries;
- list of probable phenomena of the structure and topography of the artery or arteries (the phenomenon is indicated as a single event):
- aplasia – absence of an artery;
- hypoplasia - a sharp decrease in the diameter of the artery;
- hyperplasia - a sharp increase in the diameter of the artery;
- bend, curvature, tortuosity, deviation, S-shaped artery - a change in the typical (generally recognized) course or direction of the artery;
- elongation;
- shortening;
- duplication - non-fusion of connecting arteries;
- fusion of paired arteries into a common trunk;
- insular structure - division of an artery in a limited area;
- plexiform structure - division of the artery over a long section;
- anterior trifurcation of the ICA – the origin of both ACAs from one ICA;
- partial posterior trifurcation of the ICA – equality in diameter of the posterior communicating artery and the posterior cerebral artery of one side;
- posterior trifurcation of the ICA is complete – superiority in diameter of the PCA over the proximal segment of the PCA on one side.