Vertebral artery syndrome (VAS) is not a separate disease. It can be observed in a number of different pathologies, in which there is a narrowing of the lumen of one or two vertebral arteries, deformation of the walls and irritation of the nerves located nearby. As a result, the blood supply to certain parts of the brain is disrupted, which leads to a deterioration in their performance, sometimes to the point of critical conditions. In such situations, patients may suffer from persistent migraines, various visual and hearing impairments, loss of consciousness or a stroke. As a result, irreversible changes in the brain can occur, which can result in disability or even death.
Vertebral artery syndrome is a collective term that can be used to describe the clinical picture of many diseases that are fundamentally different in the cause of development, including cervical migraine or Barre-Lieu syndrome, arterial hypoplasia, vertebrobasilar insufficiency, provoked by cervical osteochondrosis, etc.
Vertebral artery compression syndrome is included in the International Classification of Diseases (ICD-10), where it is assigned code G99.2. This allowed doctors to widely use this term when describing a number of diseases and at the same time gave rise to lively discussions in medical circles about the advisability of its use when making a diagnosis, since SPA is nothing more than a complex of symptoms, and the causes of its occurrence can be very diverse.
Anatomy of the vertebrobasilar region and the mechanism of development of SPA
Two vertebral arteries originate in the upper part of the chest, pass through the lumen of the 6th cervical vertebra and rise strictly vertically through similar natural openings in the overlying cervical vertebrae. In the area of the occipital opening they merge into a single vessel called the basilar artery.
Therefore, vertebral artery syndrome can occur both against the background of the development of systemic vascular pathologies, and as a result of damage to the anatomical structures surrounding these blood vessels, i.e. connective tissue formations, muscles, nerves, vertebrae.
The two vertebral arteries and the basilar artery form the vertebrobasilar basin. They provide 15-30% of the blood supply to the brain. These arteries are responsible for the blood supply:
- the spinal cord passing at the level of the cervical spine;
- cerebellum;
- inner ear;
- posterior lobes of the thalamus and hypothalamus;
- midbrain and medulla oblongata;
- certain parts of the temporal and occipital lobes of the brain.
Therefore, if blood flow in the vertebral arteries is disrupted, regardless of the causes and location of the narrowing or blockage of their lumen, the listed parts of the spinal cord and brain experience a deficiency of oxygen and nutrients. This leads to the appearance of manifestations characteristic of SPA in the form of dizziness, pain of varying degrees of intensity, tinnitus, impaired coordination of movements, loss of consciousness, etc.
During vertebral artery syndrome there are 2 stages:
- Functional or dystonic - the initial stage of the development of SPA, at which the emerging manifestations of circulatory disorders mainly consist of the appearance of headaches of a burning, aching or pulsating nature, dizziness, unsteadiness of gait, visual disturbances in the form of darkening in the eyes, signs of photopsia. Most often, such symptoms are paroxysmal in nature and appear when the head is held in a forced position for a long time or there is a sudden movement. If this is accompanied by strong and prolonged spasms of the arteries, the disease leads to the formation of persistent foci of cerebral ischemia, which indicates the transition of SPA to the second stage of development.
- Organic or ischemic - accompanied by the occurrence of persistent disturbances in the blood supply to brain tissue, which leads to severe headaches, dizziness, reflexively causing nausea and vomiting, as well as serious disturbances in coordination, orientation in space, speech and other severe disorders. With a sudden movement, a person may suddenly fall while in the creation or lose it. An improvement in the condition is observed after taking a horizontal position.
Photopsia is a condition in which bright spots, spots, and sparks appear before the eyes.
Causes of development of vertebral artery syndrome
SPA can occur against the background of a large number of diseases. All of them can be divided into 3 groups: congenital anomalies, vascular pathologies and vertebrogenic (spine-related) disorders. But in all cases, either compression of the blood vessels (stenosis) occurs by one or another anatomical structure or a decrease in their lumen, which leads to disruption of blood flow through them.
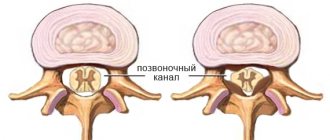
Most often, the vertebral arteries are compressed in the area of 5-6 cervical vertebrae, as they most often suffer from osteochondrosis, protrusions, intervertebral hernias, and spondylosis.
Most often, vertebral artery syndrome is a consequence of:
- Osteochondrosis of the cervical spine and its complications in the form of protrusions and herniations of intervertebral discs, as well as spondylosis. In such situations, a decrease in the height of the intervertebral discs is observed, which leads to disturbances in the anatomy of the spine and compression of one or both vertebral arteries by the approaching vertebrae or by bone outgrowths (osteophytes) formed on their edges.
- Pathological mobility of the cervical vertebrae, basilar impression, subluxation of the articular processes of the vertebrae, Powers and Kimmerly anomalies. In such cases, the vertebral arteries are displaced or compressed by spasmodic muscle fibers or abnormally located bone structures.
- Compression of the spinal roots. This is accompanied by reflex arterial stasis, i.e. stopping blood flow.
- Thrombosis and atherosclerosis of the vertebral arteries. These vascular pathologies lead to a narrowing of the lumen of the arteries as a result of the formation of blood clots or atherosclerotic plaques, the size of which directly affects the quality of blood flow. In some cases, the blood passage can be so weakened or completely blocked that a stroke results.
- Benign and malignant tumors located in close proximity to the vertebral arteries. They are also capable of mechanically compressing vessels and leading to corresponding circulatory disorders in the vertebrobasilar region.
In most cases, the left vertebral artery is affected, since it is in it that atherosclerotic plaques most often form, and developmental anomalies are more often observed on the left side.
Also, the reason for the development of SPA can be:
- fibromuscular dysplasia;
- tortuosity and the presence of kinks of the vertebral arteries;
- hypertension;
- systemic vasculitis;
- myofascial syndrome;
- scoliosis;
- spondylolisthesis, etc.
Treatment measures
The most important task in treatment is to replenish the blood supply with further elimination of causative factors. Typically, therapy involves taking medications in combination with physical therapy measures.
Patients are often prescribed nonsteroidal anti-inflammatory drugs, which are accompanied by analgesic and anti-inflammatory effects. In addition, drugs are used to relieve swelling and replenish blood supply.
In the process of selecting pharmaceuticals, the patient must have a clear understanding of the state of his health. Treatment and signs of extravasal compression of both vertebral arteries are very important. The slightest mistakes in choosing medications can lead to irreparable consequences.
- Asymmetry of blood flow in the vertebral arteries: causes, symptoms and treatment of pathology
As for physiotherapeutic techniques, the following procedures are effective:
- massage,
- physiotherapy,
- acupuncture,
- visiting a physiotherapy room.
If your health suddenly worsens, then you must inform your leading doctor about this so that he can adjust subsequent therapy.
If all of the above methods do not have the desired effect, and the condition does not change in any way, then you may be offered surgery.
At the end of the treatment course, patients are advised to visit a medical and preventive sanatorium to undergo a course of rehabilitation treatment. This will help to quickly recover and improve the patient’s general well-being.
Types of SPA
Depending on what caused the disruption of blood flow in the vertebral arteries, there are 4 forms of SPA:
- compression – occurs when the arteries are mechanically pinched;
- irritative - is a consequence of spasm of the muscle fibers of the arterial walls, which is observed when the nerve fibers innervating it are irritated;
- angiospastic - develops when irritation of receptors located at the level of the affected spinal motion segment of the cervical spine and is also accompanied by reflex vascular spasm;
- mixed – the action of several factors is observed.
Most often, patients are diagnosed with mixed forms of vertebral artery syndrome, namely compression-irritative and reflex-angiospastic.
In this case, vertebral artery syndrome can occur in completely different ways. Based on this, several of its clinical forms are identified, described below.
Barre-Lieu syndrome
This syndrome is also called cervical migraine. Its main manifestation is headache, which occurs in the cervical-occipital region. It tends to quickly spread to the parietal, occipital and frontal parts of the head.
Most often, the pain is shooting, throbbing or constantly present. Mostly they occur in the morning immediately after waking up and are associated with an uncomfortable head position during sleep. They may also appear or intensify during running, fast walking, strong vibrations, for example, during a bumpy ride, or sudden turns of the head.
With Barré-Lieu syndrome, patients may suffer from autonomic disorders, i.e., the appearance of a feeling of heat, chills, a sudden increase in sweating, difficulty swallowing, etc. Also, headaches may be accompanied by difficulties in maintaining body balance and visual impairment.
Basilar migraine
With this form of vertebral artery syndrome in patients, the clinical picture is dominated by migraines, accompanied by:
- bilateral visual impairment;
- severe dizziness;
- impaired coordination of movements while maintaining normal muscle tone;
- tinnitus;
- speech disorders.
During an attack, pain is most acutely felt in the back of the head and often provokes reflex irritation of the vomiting center of the brain. Sometimes the pain can become so severe that the person loses consciousness.
Basilar migraine is a consequence of impaired blood flow in the basilar artery, formed by the fusion of two vertebral arteries.
Vestibulo-atactic syndrome
This form of SPA is manifested by the presence of:
- dizziness;
- imbalance, which leads to a feeling of decreased stability;
- nausea or vomiting;
- darkening of the eyes;
- a feeling of disturbances in the functioning of the cardiovascular system.
These symptoms tend to intensify after a long stay in an uncomfortable position or with sudden movement of the neck.
Cochleo-vestibular syndrome
In this form, the clinical picture of vertebral artery syndrome is dominated by hearing impairment. Patients may experience difficulty recognizing whispers and general hearing impairment. They often complain of tinnitus, the intensity of which depends on the position of the head.
Hearing impairment is confirmed by instrumental diagnostic methods, in particular an audiogram.
Often, hearing impairment in cochleo-vestibular syndrome is accompanied by the occurrence of facial paresthesia, i.e., a decrease in the sensitivity of the facial skin, the appearance of a crawling sensation, and tingling. During an attack, a person may sway, lose a sense of stability, and may feel dizzy.
Ophthalmic syndrome
Visual impairment mainly consists of the appearance of photopsia, increased eye fatigue and deterioration in vision clarity while reading or working at the computer. Often there are signs of conjunctivitis, as well as loss of entire fields of vision, especially in certain positions of the head.
Ischemic attacks
In case of circulatory disorders in the vertebrobasilar system, ischemic attacks can occur, which occur:
- short-term sensory and motor disorders;
- speech disorders;
- partial or complete loss of vision;
- dizziness;
- nausea, vomiting;
- swallowing disorders;
- impaired coordination of movements.
Drop attacks
A drop attack is a causeless fall, often with preservation of the creation, which is caused by a sharp cutoff of blood flow to the brain. They are often observed when the head is thrown back and are caused by sudden paralysis of the limbs. But the restoration of motor function usually occurs quickly.
GBOU "NIKIO im. L.I. Sverzhevsky" of the Moscow Department of Health
Developer institution:
State budgetary healthcare institution "Scientific and Practical Center of Otorhinolaryngology" of the Moscow Department of Health and the Department of Otorhinolaryngology of the Medical Faculty of the State Educational Institution of Higher Professional Education "Russian State Medical University".
Compiled by:
Doctor of Medical Sciences prof. A.I. Kryukov ; Doctor of Medical Sciences, Prof. V.T.Palchun ; Doctor of Medical Sciences prof. N.L. Kunelskaya ; Doctor of Medical Sciences M.V. Tardov ; Ph.D. HER. Zagorskaya; Ph.D. E.S.Yanyushkina, Ph.D. E.V. Baibakova; Ph.D. M.A. Chugunova; Ph.D. Yu.V. Levin ; Ph.D. A.L. Guseva; Z.O.Zaoeva.
Reviewers:
Doctor of Medical Sciences, Professor I.D. Stulindoctor of Medical Sciences, Professor S.V. Morozova
Purpose:
The methodological recommendations describe a diagnostic algorithm for central dysfunction of the vestibular analyzer, a pathology manifested by dizziness - one of the most common complaints during outpatient visits. The methodological recommendations are intended for otorhinolaryngologists, neurologists, otoneurologists and general practitioners.
This document is the property of the Moscow Department of Health and may not be reproduced without appropriate permission.
Introduction
When examining a patient with complaints of dizziness, it is first necessary to differentiate between peripheral and central vestibular syndromes.
The role of nystagmus in topical diagnosis is limited, but some of its types may correspond to certain local brain damage. It should also be noted that there is no nosological specificity of various types of nystagmus.
It is generally accepted that horizontal nystagmus most often corresponds to damage to the peripheral part of the vestibular analyzer. A pronounced rotatory component of nystagmus indicates involvement of central structures in the process.
Vertical nystagmus with a downward fast phase direction may correspond to damage to the cervicomedullary region and inferior cerebellar peduncles, and with an upward fast phase direction it can be recorded with damage to the anterior parts of the vermis or superior cerebellar peduncles (Arnold-Chiari malformation type I). Also associated with pathological processes in the area of the craniovertebral junction is periodic alternating nystagmus - a cyclic disorder in which horizontal jerky nystagmus spontaneously acquires the opposite direction with a periodicity of 1 to 3 minutes.
Retraction nystagmus, characterized by irregular twitching of the eyes into the orbit, is associated with lesions of the midbrain tegmentum or quadrigeminal. This type of nystagmus can be combined with pulsating, as well as convergent nystagmus, which is characterized by slow divergent movements of the eyeballs, interrupted by fast convergent impulses.
Lesions of the caudal parts of the pons sometimes cause floating movements of the eyeballs - rapid downward movements of the eyeballs followed by a return to their original position. Nystagmoid twitching of one eye occurs with severe damage to the midbrain and lower parts of the pons.
Sawtooth nystagmus develops with lesions of the caudal parts of the brain stem and consists of rapid unfriendly eye movements, in which one eyeball turns upward and inward, and the other downward and outward.
A rare, unusual movement disorder of the eyeballs, called opsoclonus, consists of a bout of sequential saccades that are associated with damage to the cerebellum, and less commonly, the brainstem or thalamus. In cases where such saccades occur in the horizontal plane, the terms “ocular myoclonus” or “dancing eyes syndrome” are used.
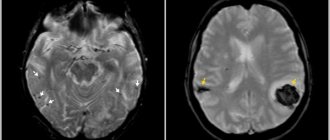
If a peripheral syndrome is diagnosed, it may be necessary, in addition to audiological and vestibulological studies, to conduct: multislice computed tomography (MSCT) of the temporal bone to assess the pathology of the labyrinth; magnetic resonance imaging (MRI) to verify the formation of the cerebellopontine angle and vaso-neural conflict.
If a violation of the functions of balance and coordination of the central type is diagnosed, then a neurological examination should determine the areas of damage: the vestibular nuclei of the brainstem, the upper brainstem structures, the cerebellum and its pathways, the frontal or parietal cortex. Confirmation of the topical diagnosis is provided by MRI of the brain, and to clarify the etiological factors, radiography of the cervical spine and cranio-vertebral junction, as well as ultrasound examination of blood flow in the main arteries of the neck and head are used.
Anatomy and physiology of the vertebrobasilar system
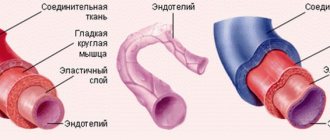
The paired vertebral artery (VA), arising from both sides of the subclavian artery, is its first and largest branch (Fig. 1). According to A.V. Pokrovsky, the following segments of PA are distinguished:
Figure 1. Trajectory of the vertebral artery.
1) The first segment (V1) from the mouth to the entry into the canal of the transverse processes of the cervical vertebrae. As a rule, the artery enters the transverse process of the sixth or fifth cervical vertebra.
2) The second segment (V2) – before the exit from the foramen of the transverse process of the second cervical vertebra. In the absence of vertebral pathology, the course of the vessel in this segment is relatively straightforward: each vertebral artery is held almost exactly in the center of the opening of the transverse process with the help of thin connective tissue trabeculae and remains intact during any movement in the cervical joints within the limits of physiological mobility.
3) The third segment (V3) – before entering the cranial cavity. After leaving the opening of the transverse process of the axis, the vertebral artery deviates outward and enters the opening of the transverse process of the atlas. Further in the horizontal plane, heading dorsally, it bends around the lateral mass of the atlas, turns up and forward and, piercing the atlanto-occipital membrane, penetrates into the cranial cavity through the foramen magnum. In this segment, the artery makes four bends in different planes, including two at right angles, which, in accordance with the laws of hydrodynamics and similar to the siphon of the internal carotid artery, ensures smoothing of the pulse wave and uniformity of blood flow.
4) The fourth segment (V4) - to the confluence of the right and left vertebral arteries on the lower surface of the medulla oblongata or the bridge into the basilar artery (BA).
At the level of the first cervical vertebra, the VA is surrounded by the atlanto-occipital sinus, in which it is “suspended” by fibrous cords. The walls of the sinus are unyielding; As a result, the pulsation of the artery in the sinus cavity stimulates the outflow of venous blood, being an important regulatory mechanism of cerebral hemocirculation.
The radicular arteries depart extracranially from the VA, supplying the lower cervical (C4-C8) and upper thoracic (Th1-Th3) segments. The four upper cervical segments (C1-C4) are supplied by the anterior spinal artery, which is formed by the fusion of the anterior spinal arteries, branches of the vertebral arteries. The PA and anterior spinal arteries on the anterior surface of the medulla oblongata form an anastomotic rhombus.
Intracranially, the vertebral and basilar arteries give off small branches that supply blood to the medulla oblongata and the pons, respectively.
The largest branch of the VA is the posterior inferior cerebellar artery, which provides vascularization to the inferior surface of the cerebellum. It also gives branches to the villous plexus of the fourth ventricle, the ventrolateral surface of the medulla oblongata, and to the roots of the X, IX, VIII and VII cranial nerves. The same artery is the source of the posterior spinal artery.
From the caudal segment of the basilar artery arises the anterior inferior cerebellar artery, which supplies the inner ear (Fig. 2), part of the inferior peduncles and the ventral part of the cerebellum.
| 1 – main artery; 2 – anterior inferior cerebellar artery; 3 – anterior vestibular artery; 4 – artery of the labyrinth; 5 – common cochlear artery; 6 – main cochlear artery; 7 – posterior vestibular artery |
Figure 2. Blood supply to the inner ear.
The oral portion of the basilar artery gives rise to the superior cerebellar artery, which carries blood to the convexital surface of the cerebellar hemispheres.
The main artery in its normal development is divided into the right and left posterior cerebral arteries, the branching area of which extends to the lower surface of the temporal and occipital lobes to the parieto-occipital sulcus. The area of the artery's blood supply includes the hypothalamus, cerebral peduncles, posterior parts of the corpus callosum, hippocampus, ependyma of the lateral ventricles, choroid plexuses and, most importantly, the visual cortex.
Intravasal factors influencing
on the vertebrobasilar blood flow
In addition to regulatory factors, the features of cerebral vascular architecture have a huge impact on blood flow in the vertebrobasilar system. Analysis of the structure of the arterial system of the brain showed that its typical structure (Fig. 3) occurs in no more than 50% of cases. It is important to emphasize that the variability in the development of the arteries of the posterior basin significantly exceeds the variety in the structure of the branches of the carotid system: thus, posterior trifurcation is recorded with a frequency of up to 25% of cases, and variants of the structure without fusion of the vertebral arteries are also found. The diameters of the vertebral arteries are often different - in 25-30% of cases the right vertebral artery predominates, and the left one can predominate with the same frequency.
| 1 – intracranial part of the internal carotid artery; 2 – middle cerebral artery; 3 – anterior cerebral artery; 4 – anterior communicating artery; 5 – posterior communicating artery; 6 – posterior cerebral artery; 7 – main artery; 8 – superior cerebellar artery; 9 – anterior inferior cerebellar artery; 10 – posterior inferior cerebellar artery; 11 – vertebral artery. |
Figure 3. Structure of the large arterial circle of the brain.
The variant of the origin of the vertebral artery from the subclavian artery is important. There are frequent cases where the mouth of the vertebral artery is located not on the upper, but on the posterior and even lower wall of the subclavian artery, which leads to deformation of the initial segment of the VA with a high probability of the formation of a local hemodynamic difference, limiting the blood flow in the vessel.
Separately, mention should be made of such important intracranial anastomoses as the posterior communicating arteries: the absence of one posterior communicating artery is recorded in 6-10% of cases, and the absence of both posterior communicating arteries is not uncommon - complete separation of the posterior sections of the circle of Willis.
Intravascular factors affecting the vascularization of the brain include various types of stenotic processes in the vertebral and basilar arteries: atherosclerotic, inflammatory, fibromuscular hyperplasia.
Extravasal effects on vertebrobasilar blood flow
Persistent or transient compression of the vertebral artery in the canal of the transverse processes or, less frequently, in the intermuscular spaces can cause a decrease in blood supply to the vertebrobasilar region, as well as a narrowing of the lumen of the artery due to a plaque or thrombus. The clinical picture of suffering develops depending on the development of collaterals and the structure of the arterial circle at the base of the brain. In the latest version of the International Classification of Diseases, 10th revision, such a symptom complex is defined as “vertebrobasilar arterial system syndrome” within the framework of “transient transient cerebral ischemic attacks (attacks) and related syndromes” (G 45.0).
According to the areas of vascularization of the vertebral basin and the basilar artery, the symptoms associated with impaired blood flow in the VBS are diverse and include cochleovestibular disorders, visual and oculomotor disorders; violations of statics and coordination of movements. It is this symptom complex that occurs in more than 80% of patients with circulatory failure in the posterior circulatory system.
Visual and oculomotor disorders are very common phenomena and are manifested by blurred visual fields, blurred vision of objects, photopsia or scintillating scotomas and loss of visual fields. Oculomotor disorders are expressed by transient diplopia (in different directions of gaze) with mild paresis of the eye muscles and convergence insufficiency.
Static and dynamic ataxia is one of the most common symptoms, manifested by complaints of instability and staggering when walking. Coordination of movements may also be affected.
Cochleovestibular disorders manifest themselves in the form of acutely developing systemic or non-systemic dizziness, sometimes with spontaneous nystagmus, dizziness is often accompanied by nausea and vomiting. There is tinnitus of various timbres: from high (squeaking and whistling) to low tones (surf noise, buzzing). In this case, dizziness as a monosymptom can be regarded as a reliable sign of dyscirculation in the VBS only in combination with other signs of circulatory disorders in it in patients with a relatively persistent otoneurological symptom complex.
Less known, although not uncommon, are optic-vestibular disorders. These include symptoms of “shading shadows” and “convergent vertigo,” when sufferers experience dizziness or unsteadiness when seeing flashes of light and shadow or when looking down. Various types of visual agnosia with impaired optical-spatial perception can be identified, as well as elements of sensory and amnestic aphasia as a result of ischemia in the distal cortical branches of the posterior cerebral artery.
Characteristic symptoms are attacks of sudden falling and immobility without loss of consciousness (drop attacks) and with loss of consciousness (Unterharnsteidt's syndrome), usually occurring with sudden turns or throwing back the head. Manifestations of diencephalic disorders include severe general weakness, irresistible drowsiness, disturbances in the rhythm of sleep and wakefulness, as well as various autonomic-visceral disorders, sudden increases in blood pressure, heart rhythm disturbances, etc.
The basis for the expanded diagnosis of the syndrome of transient circulatory disorders in VBS may be the unjustified inclusion of symptoms related to the initial stages of the well-studied “vertebrogenic vertebral artery syndrome”. Its initial or angiodystonic stage is defined as a syndrome of vertebrogenically caused irritation of the perivascular sympathetic plexus of the vertebral artery with typical pain (vegetalgic) symptoms. These peculiar cervico-occipital pains, spreading to the parietal, temporal regions and orbit, are often described as “removing the helmet.” The predominant pain component is felt as a burning sensation, paresthesia, a feeling of squeezing or fullness in the eyes, ears, and throat. The described phenomena intensify with a sharp change in the tilt of the head or in an uncomfortable position, especially after sleep. Visual and cochleovestibular symptoms are also peculiar and usually arise or worsen not as isolated symptoms, but during attacks of characteristic headache.
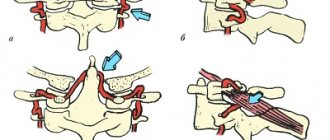
Features of the course of the vertebral artery in the intermuscular spaces and in the canal of the transverse processes determine the options for possible extravasal influences on it. The effect of muscles on PA is associated with their segmental tonic tension, usually as part of myofascial syndromes associated with osteochondrosis of the cervical spine.
Before entering the canal of the transverse processes, the vertebral artery may be compressed by the edge of the anterior scalene muscle or the longus colli muscle. A more common option is compression of the VA before entering the cranial cavity by the inferior oblique muscle of the head, which, with a sharp turn and tilt of the head, stretches and can impinge on the greater occipital nerve, branches of the second cervical nerve and the VA itself.
More complex and ambiguous effects on the VA can be exerted by the structures that make up the canal of the transverse processes. Arthrosis of the uncovertebral joints can lead to direct compression with changes in the course of the entire intraosseous segment of the vertebral artery. With ultrasound angioscanning or radiopaque imaging methods, the artery takes on a “tortuous” appearance, bending around the deformed joints.
Excessive mobility (instability) of the motor segments of the cervical spine creates conditions for mechanical effects on the VA: compression of the artery or irritation of the periarterial sympathetic plexus.
Complex effect on the vestibular analyzer
As a rule, individual manifestations of abnormalities of the cervical spine or the vascular system of the brain are not so significant as to cause dizziness or impair coordination. The clinical situation may vary due to a combination of several abnormal and pathological factors.
For example, a combination of hypoplasia of one of the vertebral arteries and incompetence of the contralateral posterior communicating artery (Fig. 4) may not lead to coordination disorders. However, in the case of the development of instability or muscular-tonic phenomena against the background of a violation of the statics of the cervical spine - phenomena that can cause a mechanical effect on the hemodynamically predominant VA - cerebral syndrome may debut with dizziness.
| 1 – right posterior communicating artery; 2 – absence of the left posterior communicating artery; 3 – hypoplastic right vertebral artery; 4 – hemodynamically predominant vertebral artery |
Figure 4. Combination of vertebral artery hypoplasia and contralateral posterior communicating artery incompetence.
A similar situation may arise if the patient has an Arnold-Chiari malformation. This pathology may not manifest itself clinically until a violation of the motor stereotype of the cervical spine is formed or arterial hypertension develops, accompanied by microcirculatory disorders, especially at the level of the venous segment. These processes can ultimately lead to compression of the VA or the cerebellar tonsils themselves, and to liquorodynamic disorders.
Thus, identifying positional (vertebrogenic) nystagmus requires expanded examination: ultrasound examination of blood flow in the VBS and radiation examination of the cervical spine.
Radiation diagnostics of spinal pathology.
Survey radiographs of the spine, in accordance with the recommendations, are necessarily performed in two projections, which makes it possible to study the structure of the vertebral body, the height of the intervertebral spaces, and the condition of the intervertebral and hamate joints. Spot-on images of the atlantoaxial joint demonstrate the features of Cruvelier's joint. If an anomaly of the craniovertebral joint is suspected, a special imaging technique is used to calculate the angles between the components of the skull base and the axis of the odontoid process.
A large group of radiological symptoms of osteochondrosis is associated with impaired static function of the spine. On radiographs, this is manifested by a change in the axis of the spine - straightening of the cervical and lumbar lordosis or increased thoracic kyphosis. When the C5-C7 discs are affected, complete straightening of the cervical lordosis is usually determined; changes in the C3-C5 discs cause only partial straightening of the lordosis. Kyphosis may form. In this case, the distance between the processes at the level of kyphosis increases.
| Figure 5. Spondylolisthesis. |
Objective data on the mobility of the cervical spine are provided by functional x-ray studies with flexion and extension, accompanied by the effect of strengthening or weakening hidden displacements of the vertebrae. Radiographs with functional tests may reveal displacement of the vertebrae (Fig. 5) forward and backward. The simultaneous displacement of two or more vertebrae in the same direction is referred to as scalene displacement. These changes indicate a loss of the fixation ability of the disc and the initial manifestations of osteochondrosis.
Instability of motion segments in the cervical spine is common, which is often associated with posterior extensor subluxation according to Kovacs. A characteristic feature of subluxation according to Kovacs is the presence of displacement of the lower edge of the articular process during extension, which is normalized in a neutral position or during flexion. Such a subluxation appears during extension and indicates pathological mobility of the spinal motion segment (SMS) and the possibility of a direct vertebrogenic effect on the VA. Another symptom of pathological mobility is the bevel of the anterior-superior angle of the vertebra in the lateral projection.
The indicator of instability of the SDS is determined for all segments of the cervical spine. Particularly clinically significant is pendulum-shaped polysegmental instability at the mid-cervical level (the level of passage of the VA in the canals of the transverse processes) with a high degree of instability - the instability index is above 3 mm.
The most important from a clinical point of view and studied in detail in relation to X-ray diagnostics are the following forms of degenerative-dystrophic lesions of the spine: osteochondrosis, spondylosis deformans, fixing ligamentosis (Forestier disease), disc herniation (posterior cartilaginous node), Schmorl's hernia, spondyloarthrosis.
It is important to identify, using radiography, anomalies of the craniovertebral junction - congenital or acquired disorders of the structure of the base of the skull or the upper cervical spine. The abnormal structure of bone structures leads to a narrowing of the bone spaces containing the lower parts of the brain stem and the cervical spinal cord, which can lead to hemo- and liquorodynamic disorders, as well as compression of the brain elements themselves, manifested by cerebellar, vestibular and spinal disorders. A clinical picture of damage to the caudal group of cranial nerves may also be observed. The most common are:
- assimilation of the atlas (fusion of the first cervical vertebra with the skull) in the area of the foramen magnum;
- platybasia – flattening of the base of the skull;
- basilar impression – displacement of the odontoid process upward into the area of the foramen magnum;
- Klippel-Feil anomaly – fusion of cervical vertebrae;
- atlantoaxial dislocation – displacement of the atlas anteriorly in relation to the axis (second cervical vertebra), often observed in the absence or underdevelopment of a tooth, its non-fusion with the vertebral body;
- Kimerli's anomaly - the presence of an additional bone arch-semi-ring, forming a bone canal instead of the groove of the vertebral artery above the arch of the first cervical vertebra (Fig. 6);
| Figure 6. Kimerli anomaly. 1 – vertebral artery, 2 – bone bridge |
- Arnold-Chiari malformation type I - descent of the cerebellar tonsils into the foramen magnum (Fig. 7).
| Figure 7 . Arnold-Chiari malformation. 1 – cerebellum; 2 – cerebellar amygdala; 3 – atlas; 4 – spinal cord. |
If there are clinical signs of pathology of the cervical roots (shooting pain, loss of tendon reflexes, sensitivity zones), an MSCT or MRI of the cervical spine is necessary. It is these techniques that make it possible to reliably diagnose Arnold-Chiari malformation.
Tomography data is used to determine the presence of protrusions and herniations of intervertebral discs and their effect on the posterior longitudinal ligament and spinal nerve roots. Compression of the spinal cord or anterior spinal artery causes not only segmental sensitivity and movement disorders, but also conduction sensitivity disorders, and in severe cases, pyramidal insufficiency and dysfunction of the pelvic organs, which corresponds to the concept of cervical level myelopathy.
Ultrasound examination of cerebral blood flow.
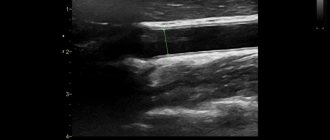
The primary assessment of the condition of the neck arteries is carried out using a linear sensor of an ultrasound scanner: after excluding developmental anomalies of the brachiocephalic arteries, the parameters of flow velocity and resistance are recorded. Then a Doppler study of blood flow in the cerebral arteries is performed using transtemporal and suboccipital access using standard methods. The middle (MCA), anterior (ACA), posterior (PCA), vertebral (VA) arteries on both sides and the basilar artery (BA) are located. Using compression tests, the functions of the connecting arteries are assessed. Next, blood flow rates in the cerebral venous trunks are assessed: veins of Rosenthal, Galen, middle cerebral veins; straight and cavernous sinuses.
When assessing the LSC in the located arteries, the symmetry (equality) of the LSC in paired vessels is taken into account, as well as the compliance of the LSC with age standards and the observance of the proportions between the LSC in the extra- and intracranial arteries.
The next step is to study the PA in the third segment after repeating the head rotation three times at the maximum angle from side to side (pendulum test - MP). In this case, a Dopplerogram is recorded corresponding to the third cardiac cycle in a standard position after completion of movements. Turning the head in a flexion position makes it possible to evaluate the effect on PA at the upper cervical level, in a neutral position - in the interscalene space, and tilting the head back and forth - at the mid-cervical level. Before Doppler tests, blood pressure is measured with an electronic tonometer.
Ultrasound angioscanning plays an important role in studying the trajectory and intraluminal contents of arterial arteries, which makes it possible to detect stenosis of the lumen (atherosclerotic plaque, thrombus, fibromuscular dysplasia), pathological tortuosity, and dissection of the arterial wall. Identification of the local hemodynamic difference in flow velocity in the artery is of fundamental importance.
Predisposing factors for dissection include neck injuries and infections, however, apparently, local disruption of the properties of the vessel wall is also important in the development of this pathology. When clarifying the circumstances of the occurrence of dizziness, information may be important not only about the effects on the cervical-occipital region (pulsation techniques of manual therapy), but also about the patient’s long stay in a position with a fixed neck, as in dental or ophthalmological treatments.
Dopplerographic dissection of the wall of the cervical artery is manifested by a pattern of stenotic blood flow in the area of interest, which is caused by a narrowing of the lumen of the artery at the level of pathology: an increase in BFV, an expansion of the spectrum due to high frequencies, a difference in peripheral resistance parameters between the pre- and poststenotic segments. Sometimes a “double” spectrum can be insonated due to the superposition of the sound of the flow in the main channel and in the hematoma channel. With angioscanning in the dissection area, it is possible to visualize thickening of the arterial wall with a wide anechoic layer and narrowing of the arterial lumen in the absence of intraluminal formations. If the course of the process is unfavorable, thrombosis may develop in the narrowing zone.
Angioscanning also allows you to evaluate the diameter and shape of the lumen of the internal jugular veins, the speed of blood flow in the jugular and vertebral veins. Exceeding standard values may indicate difficulty in venous outflow from the cranial cavity, which often correlates with the presence of labyrinthine hydrops.
Neuroimaging techniques
MRI or MSCT of the head is indicated for the patient when a central type of lesion of the vestibular analyzer is detected. MRI in standard magnetic sequences (T1, T2, FLAER) allows you to identify infarct and post-hemorrhagic lesions in the brain, signs of leukoaraiosis and hydrocephalus, space-occupying formations, incl. neoplasms of the cerebellopontine angle.
Magnetic resonance angiography (MRA) in the first (arterial) phase allows to identify abnormalities in the structure of the arteries (aneurysms, arteriovenous malformations), as well as significant stenoses of the intracranial arteries. In the second (venous) phase, anomalies in the structure of the veins and sinuses of the dura mater can be assessed.
MSCT of brain vessels is a study that is more sensitive than MRA and is carried out with a bolus injection of intravenous contrast. This technique also allows you to evaluate separately the arteries and veins of the brain.
In some cases, three-dimensional reconstruction of the arterial and venous beds, which is possible with modern tomographic devices, brings great diagnostic benefit.
To identify the neurovascular conflict of the VIII cranial nerve and the arteries of the SMV, special MRI programs (usually on high-tensile installations - 3T) 3D-SPGR and 3D-FIESTA are used.
List of abbreviations
- PCA – posterior cerebral artery
- MP – pendulum test
- MRA – magnetic resonance angiography;
- MRI – magnetic resonance imaging
- MSCT – multislice computed tomography
- OA – main artery
- VA – vertebral artery
- SMS – vertebral motion segment
- ACA – anterior cerebral artery
- MCA – middle cerebral artery
Manifestations of vertebral artery syndrome
Thus, the main symptoms of vertebral artery syndrome are:
- headaches, mainly concentrated in the back of the head and forehead;
- pain in the neck that occurs and intensifies when moving the head or maintaining a certain position for a long time;
- dizziness, which may be accompanied by disturbances in balance and coordination of movements;
- hearing and vision impairments;
- ischemic attacks with the occurrence of speech, sensory, motor and other disorders.
Which signs of vertebral artery syndrome will be more pronounced and which will be weaker depend on the form of the vertebral artery syndrome. There may also be additional symptoms of concomitant diseases, which complicates the diagnosis.
Causes of the disease
As mentioned above, an intervertebral hernia can lead to extravasal compression of the right, left, or simultaneously two vertebral arteries. In turn, a hernia can occur due to developed osteochondrosis or physical overload. Other provoking factors may be:
- benign or malignant tumors in the neck;
- incorrect, abnormal structure of the spine, its curvature (congenital, acquired, traumatic).
Diagnostics
Diagnosis of SPA is carried out by a neurologist. The specialist needs to be able to identify the patient’s main complaints and compare them with the characteristics of each form of the disease. If the existing symptoms correspond to the clinical form of SPA, it is important to diagnose the causes of its development, i.e., to detect which vascular or spinal pathologies led to impaired blood flow through the vertebral arteries.
To this end, the doctor initially conducts a thorough examination and neurological tests, which allow one to suspect what could have caused the SPA. To confirm guesses, obtain more accurate information and detect possible concomitant diseases, the patient is prescribed:
- X-ray or CT scan of the cervical spine;
- MRI of the cervical spine;
- Ultrasound of neck vessels with Doppler sonography;
- stabilometry;
- general and biochemical blood test;
- audiometry, etc.
In our clinic, you can also learn in more detail about the composition of your body and the state of the vascular system, which is involved in the blood supply to internal organs, skeletal muscles, and the brain. Our experienced doctors will explain the data obtained to you in detail. Bioimpendansometry calculates the ratio of fat, muscle, bone and skeletal mass, total fluid in the body, and basal metabolic rate. The intensity of recommended physical activity depends on the state of muscle mass. Metabolic processes, in turn, affect the body's ability to recover. Based on the indicators of active cell mass, one can judge the level of physical activity and nutritional balance. This simple and quick test helps us identify disturbances in the endocrine system and take the necessary measures. In addition, it is also very important for us to know the condition of blood vessels for the prevention of diseases such as heart attacks, hypertension, heart failure, diabetes and much more. Angioscan allows you to determine such important indicators as the biological age of blood vessels, their stiffness, stress index (which indicates heart rate), and blood oxygen saturation. Such screening will be useful for men and women over 30, athletes, those undergoing long-term and severe treatment, as well as everyone who monitors their health.
Often, for the correct diagnosis of vertebral artery syndrome and the causes of its development, consultations with other specialized specialists, including cardiologists, ENT specialists, ophthalmologists, etc. are required.
Today, SPA is often falsely diagnosed, which is due to the insufficient completeness of the examination.
How to treat?
Treatment of extravasal compression of both vertebral arteries is primarily to eliminate the main factor in its occurrence. That is, treatment of compression occurs in parallel and simultaneously with the treatment of intervertebral disc herniation, tumor, compression fracture, and so on.
Treatment may be medication. Patients are often prescribed painkillers and anti-inflammatory drugs to relieve pain and restore normal well-being. Drugs aimed at restoring blood flow and oxygen supply to the blood may also be prescribed. All medications should be prescribed only by your doctor. The dosage and frequency of use are very important. Self-medication can only harm and worsen the situation.
Treatment of compression can take place in other directions:
- physiotherapy;
- massage and manual therapy;
- physical therapy and special gymnastics.
When all of the above treatment methods do not produce an effect for a long time, the doctor considers the possibility and advisability of surgery. Surgeons, by making small incisions, can remove discs and tumors that are compressing the arteries. Treatment of compression should be carried out by doctors of several specializations: surgeons, therapists, neurologists, oncologists and others. You will find specialists in these and other areas at the Energo clinic. Our team consists of experienced professionals who, in their practice, have encountered various cases of compression of the vertebral artery and have positive experience in eliminating it.
Treatment of vertebral artery syndrome
After confirming the presence of RAS and determining the reasons for its development, a treatment regimen is individually developed for each patient, taking into account the variant of the course of the disease. The main goals of therapy are to improve blood flow through the vertebral arteries and eliminate factors predisposing to its deterioration.
In most cases, treatment of vertebral artery syndrome is carried out at home. Only with frequent ischemic attacks is hospitalization recommended for patients, since in such cases there is a high risk of stroke.
Patients are prescribed:
- drug therapy;
- manual therapy;
- physiotherapy;
- Exercise therapy.
Sometimes surgical intervention is required to effectively eliminate factors compressing the vertebral arteries. But modern treatment methods in most cases make it possible to achieve stable remission of the disease, eliminate all its manifestations and normalize the patient’s quality of life. But this is only possible with timely diagnosis of the causes of the development of SPA and competent influence on them in compliance with all recommendations received from the doctor.
Drug therapy
Patients are prescribed a whole range of drugs that help normalize blood flow in the vertebrobasilar region.
- drugs that improve blood flow;
- NSAIDs;
- purine derivatives;
- α-blockers;
- calcium antagonists;
- cholinergics;
- neuroprotectors;
- cardiac drugs;
- muscle relaxants;
- antispasmodics;
- antimigraine drugs;
- vitamins.
Treatment of atherosclerosis, thrombosis, osteochondrosis and other detected concomitant diseases is also mandatory.
Manual therapy
Manual therapy is very effective in the treatment of spas. With the help of special soft techniques, stretching the neck muscles and restoring the correct position of the vertebrae, in some cases it is possible to completely eliminate the causes of compression of the vertebral arteries and normalize the blood flow in them.
Using the Gritsenko method to combat the manifestations of vertebral artery stenosis also allows you to normalize muscle tone and achieve effective restoration of intervertebral discs, as well as activate the body’s natural recovery processes.
Using special techniques, compression of the spinal roots and nerve fibers is eliminated, which quickly leads to the elimination of pain and neurological disorders in the form of disorders of sensitivity, mobility, etc. Moreover, the method is almost completely free of contraindications and the risk of side effects. Therefore, it can be used to treat patients even from special categories such as pregnant women and the elderly.
Physiotherapy
Physiotherapeutic treatment is also widely prescribed for SPA. It is used to normalize vascular tone, activate blood circulation and metabolism, and also have a positive effect on the central nervous system.
For vertebral artery syndrome, the following physiotherapeutic procedures are indicated:
- magnetic therapy;
- electrophoresis;
- UHF;
- ultraphonophoresis;
- Diadynamic therapy.
Exercise therapy
An individually selected set of exercises will help normalize blood flow, as well as relieve muscle spasms and strengthen weakened neck muscles. But in no case should you choose a complex of physical therapy on your own, since with certain features of vertebral artery stenosis, performing a series of head movements can lead to a sharp shortage of blood in the brain. All exercises recommended by a specialist should be performed smoothly, without sudden movements and with a large amplitude.
Thus, the development of vertebral artery syndrome should be regarded as an important signal from the body, signaling the occurrence of serious disturbances in its functioning. Therefore, when symptoms of SPA appear, it is necessary to make an appointment with a neurologist as soon as possible and undergo a comprehensive examination in order to detect the causes of its development. This will help to detect emerging diseases in a timely manner and carry out treatment appropriate to the situation, which will prevent the progression of existing pathologies and the occurrence of dangerous complications of vertebral artery syndrome in the form of stroke and death.
5 3 votes
Article rating
Prevention measures
Unfortunately, this diagnosis is made quite often not only to older people, but also to young people. In order to prevent the occurrence of this disease, certain preventive measures should be taken to prevent the disease from progressing.
Among these manipulations, the following techniques should be highlighted:
- physical therapy to strengthen the muscle corset,
- special exercises to relieve muscle tone,
- blood flow stimulating massage.
Comprehensive actions will benefit not only those at risk, but also those who suffer from osteochondrosis and hernias.
If a person is prone to developing this pathology, he is registered with a medical institution. This involves undergoing a systematic examination. At the discretion of the specialist, diagnostics of cerebral vessels may also be included. Often, the patient is recommended to take prophylactic medications.