Vertebral artery syndrome (or posterior cervical sympathetic syndrome ) is a complex of symptoms caused by compression (i.e. pressure) on the vertebral artery and the surrounding sympathetic nerve plexus.
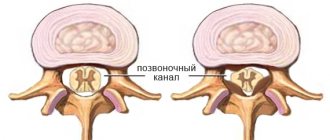
The figure shows cases of compression of the vertebral artery after exiting the bone canal:
a) arthrosis of the intervertebral joint C1 - C2;
b) Kimmerly anomaly;
c) high standing of the odontoid process of the second cervical vertebra;
d) spasmodic oblique muscle of the neck.
Features of the anatomy of the vertebral arteries
The vertebral artery is a paired blood vessel that originates from the subclavian arteries. Subsequently, both vertebral arteries (right and left) enter the foramen of the transverse process of the sixth cervical vertebra (each on its own side) and run in the bone canal formed by the transverse processes of the cervical vertebrae. Turning and tilting the head impede blood flow through the vertebral arteries, but these changes are invisible to patients with normal vascular function and the absence of additional compression factors.
In the cranial cavity, both vertebral arteries merge to form the larger basilar artery . The vertebral and basilar arteries belong to the vertebrobasilar blood supply to the brain and supply blood to the brainstem, cerebellum, cranial nerves and inner ear. Accordingly, with a decrease in the speed of blood flow through the above vessels, cerebrovascular accident syndrome in the vertebrobasilar region (VBB) may develop.
The most common causes of compression (squeezing) of the vertebral arteries
1. Manifestations of degenerative-dystrophic lesions (osteochondrosis) of the cervical spine: bone growths (osteophytes), arthrosis of uncovertebral joints, medial herniated intervertebral discs.
2. The presence of an atypical variant of the origin of the vertebral artery from the subclavian artery.
3. The presence of anomalies (structural features) of the cranio-vertebral junction (Kimmerly's anomaly, accessory cervical rib).
4. Severe spasm of the neck muscles (including the inferior oblique muscle of the head, covering the vertebral artery in the suboccipital area).
Main clinical manifestations of vertebral artery syndrome
1. Pain syndrome.
Characterized by the presence of a headache of a “pulsating” or “burning” nature, spreading from the back of the head to the temple, crown and superciliary area on one side. The pain is often constant in nature (less often paroxysmal), intensifies after sleeping in an uncomfortable position, when walking and riding in public transport.
Patients who have suffered traumatic brain injury, intoxication, or infectious lesions of the central nervous system in the past may also experience nausea, vomiting, and loss of consciousness.
2. Visual impairment.
The patient may experience pain in the eyes, decreased visual acuity, a feeling of “fog before the eyes” or “sand in the eyes.”
3. Auditory and vestibular disorders.
There may be unilateral hearing loss, dizziness, and noise in the ear.
4. Manifestations of the heart and coronary vessels.
It should be noted that in patients with a healthy heart, these disorders are most often absent, but in the presence of coronary heart disease of varying degrees, it is possible to provoke attacks of angina pectoris (acute “squeezing” or “pressing” pain in the heart area or behind the sternum), episodes of increased arterial pressure.
It is important to keep in mind that the clinical manifestations of vertebral artery syndrome may resemble the symptoms of acute cerebrovascular accident (stroke) in the vertebrobasilar region (VBB). So, the patient should immediately consult a doctor (preferably a neurologist) if he suddenly develops the following symptoms:
- severe dizziness accompanied by nausea, vomiting or imbalance of the body;
- unsteadiness when walking, awkwardness when moving the hand, changes in handwriting;
- doubling of objects;
- blurred speech (difficulty pronouncing sounds);
- decreased visual acuity.
Category “Conversation with a specialist” Vertebral artery syndrome
This article was jointly prepared by neurologists of the Academy of Health LLC, Tatyana Valerievna Solovyova and Alexandra Vladimirovna Ananina.
Vertebral artery syndrome (VAS) is a complex of symptoms resulting from disruption of blood flow in the vertebral (or vertebral) arteries. In recent decades, this pathology has become quite widespread, which is probably due to the increase in the number of office workers and people leading a sedentary lifestyle who spend a lot of time at the computer. If previously the diagnosis of SPA was made mainly to elderly people, today the disease is diagnosed even in twenty-year-old patients. Since any disease is easier to prevent than to treat, it is important for everyone to know for what reasons vertebral artery syndrome occurs, what symptoms are manifested and how this pathology is diagnosed. We will talk about this, as well as the principles of SPA treatment, in our article.
Basic anatomy and physiology Blood enters the brain through four large arteries: the left and right common carotid and the left and right vertebral. It is worth noting that 70-85% of the blood passes through the carotid arteries, so disruption of blood flow in them often leads to acute cerebrovascular accidents, that is, ischemic strokes.
The vertebral arteries supply the brain with only 15-30% of blood. Violation of blood flow in them, as a rule, does not cause acute, life-threatening problems - chronic disorders occur, which, however, significantly reduce the patient’s quality of life and even lead to disability.
The vertebral artery is a paired formation originating from the subclavian artery, which in turn arises on the left - from the aorta, and on the right - from the brachiocephalic trunk. The vertebral artery goes upward and slightly backward, passing behind the common carotid artery, enters the opening of the transverse process of the sixth cervical vertebra, rises vertically through similar openings of all overlying vertebrae, through the foramen magnum enters the cranial cavity and follows to the brain, supplying blood to the posterior parts of the brain : cerebellum, hypothalamus, corpus callosum, midbrain, partially temporal, parietal, occipital lobes, as well as the dura mater of the posterior cranial fossa. Before entering the cranial cavity, branches depart from the vertebral artery, carrying blood to the spinal cord and its membranes. Consequently, when blood flow in the vertebral artery is disrupted, symptoms arise that indicate hypoxia (oxygen starvation) of the areas of the brain that it supplies.
Causes and mechanisms of development of vertebral artery syndrome Along its length, the vertebral artery comes into contact with both the hard structures of the spinal column and the soft tissues surrounding it. Pathological changes that occur in these tissues are the prerequisites for the development of SPA. In addition, the cause may be congenital characteristics and acquired diseases of the arteries themselves.
So, there are 3 groups of causative factors of vertebral artery syndrome:
Congenital structural features of the artery: pathological tortuosity, course anomalies, kinks. Diseases that result in a decrease in the lumen of the artery: atherosclerosis, all kinds of arteritis (inflammation of the artery walls), thrombosis and embolism. Compression of the artery from the outside: osteochondrosis of the cervical spine, abnormalities of bone structure, trauma, scoliosis (these are vertebrogenic, that is, associated with the spine, causes), as well as tumors of the neck tissue, their scar changes, spasm of the neck muscles (these are non-vertebrogenic causes). Often, SPA occurs under the influence of several causative factors.
It is worth noting that RAS develops more often on the left, which is explained by the anatomical features of the left vertebral artery: it arises from the aortic arch, which often has atherosclerotic changes. The second leading cause, along with atherosclerosis, is degenerative diseases, that is, osteochondrosis. The bone canal in which the artery passes is quite narrow, and at the same time mobile. If there are osteophytes in the area of the transverse vertebrae, they compress the vessel, disrupting blood flow to the brain.
In the presence of one or more of the above reasons, factors predisposing to the deterioration of the patient’s well-being and the appearance of complaints are sudden turns or tilts of the head.
Symptoms of vertebral artery syndrome The pathological process in SPA goes through 2 stages: functional disorders, or dystonic, and organic (ischemic).
Stage of functional disorders (dystonic) The main symptom at this stage is headache: constant, intensifying during head movements or with prolonged forced positioning, burning, aching or pulsating in nature, covering the back of the head, temples and moving forward to the forehead.
Also at the dystonic stage, patients complain of dizziness of varying intensity: from a feeling of slight instability to a feeling of rapid rotation, tilting, and falling of one’s own body. In addition to dizziness, patients are often bothered by tinnitus and hearing impairment.
Various visual disturbances may also occur: sand, sparks, flashes, darkening of the eyes, and when examining the fundus, a decrease in the tone of its blood vessels.
If at the dystonic stage the causative factor is not eliminated for a long time, the disease progresses and the next, ischemic stage occurs.
Ischemic, or organic, stage At this stage, the patient is diagnosed with transient disorders of cerebral circulation: transient ischemic attacks. They are sudden attacks of severe dizziness, impaired coordination of movements, nausea and vomiting, and speech disorders. As mentioned above, these symptoms are often provoked by a sharp turn or tilt of the head. If, with such symptoms, the patient takes a horizontal position, there is a high probability of their regression (disappearance). After an attack, the patient feels tired, weak, tinnitus, sparks or flashes before the eyes, and headache.
Clinical variants of vertebral artery syndrome These are:
drop attacks (the patient suddenly falls, his head is thrown back, he cannot move or stand up during the attack; consciousness is not impaired; within a few minutes, motor function is restored; this condition occurs due to insufficient blood supply to the cerebellum and caudal parts of the brain stem); syncopal vertebral syndrome, or Unterharnsteidt syndrome (with a sharp turn or tilt of the head, as well as in the case of a prolonged stay in a forced position, the patient loses consciousness for a short time; the cause of this condition is ischemia of the region of the reticular formation of the brain); posterior cervical sympathetic syndrome, or Bare-Lieu syndrome (its main symptom is constant intense headaches of the “removing the helmet” type - localized in the occipital region and spreading to the front of the head; pain intensifies after sleeping on an uncomfortable pillow, when turning or tilting head; the nature of the pain is pulsating or shooting; may be accompanied by other symptoms characteristic of SPA); vestibulo-atactic syndrome (the main symptoms in this case are dizziness, a feeling of instability, imbalance, darkening of the eyes, nausea, vomiting, as well as disorders of the cardiovascular system (shortness of breath, pain in the heart, etc.); basilar migraine ( the attack is preceded by visual disturbances in both eyes, dizziness, unsteadiness of gait, tinnitus and blurred speech, after which intense headache occurs in the back of the head, vomiting, and then the patient loses consciousness); ophthalmic syndrome (complaints from the organ of vision come to the fore : pain, feeling of sand in the eyes, lacrimation, redness of the conjunctiva; the patient sees flashes and sparks before the eyes; visual acuity decreases, which is especially noticeable with eye strain; visual fields partially or completely disappear); cochleo-vestibular syndrome (the patient complains of decreased hearing acuity (perception of whispered speech is especially difficult), tinnitus, feeling of swaying, body instability or rotation of objects around the patient; the nature of the complaints changes - they directly depend on the position of the patient’s body); syndrome of autonomic disorders (the patient is concerned about the following symptoms: chills or a feeling of heat, sweating, constantly wet cold palms and feet, stabbing pain in the heart, headaches, and so on; often this syndrome does not occur on its own, but is combined with one or more others ); transient ischemic attacks, or TIA (the patient notes periodically occurring transient sensory or motor disturbances, disturbances in the organ of vision and/or speech, unsteadiness and dizziness, nausea, vomiting, double vision, difficulty swallowing). Diagnosis of vertebral artery syndrome Based on the patient’s complaints, the doctor will determine the presence of one or more of the above syndromes and, depending on this, will prescribe additional research methods:
X-ray of the cervical spine; magnetic resonance or computed tomography of the cervical spine; duplex scanning of the vertebral arteries; vertebral Dopplerography with functional loads (flexion/extension/rotation of the head). If the diagnosis of SPA is confirmed during further examination, the specialist will prescribe appropriate treatment.
Treatment of vertebral artery syndrome The effectiveness of treatment for this condition directly depends on the timeliness of its diagnosis: the earlier the diagnosis is made, the less thorny the path to recovery will be. Complex spa treatment should be carried out simultaneously in three directions:
therapy for pathology of the cervical spine; restoration of the lumen of the vertebral artery; additional treatment methods. First of all, the patient will be prescribed anti-inflammatory and decongestant drugs, namely non-steroidal anti-inflammatory drugs (meloxicam, nimesulide, celecoxib), angioprotectors (diosmin) and venotonics (troxerutin).
In order to improve blood flow through the vertebral artery, agapurine, vinpocetine, cinnarizine, nicergoline, instenon and other similar drugs are used.
To improve the metabolism (metabolism) of neurons, use citicoline, gliatilin, cerebrolysin, actovegin, mexidol and piracetam.
To improve metabolism not only in nerves, but also in other organs and tissues (vessels, muscles), the patient takes mildronate, trimetazidine or thiotriazoline.
In order to relax the spasmodic striated muscles, mydocalm or toldel will be used, vascular smooth muscles - drotaverine, better known to patients as No-shpa.
For migraine attacks, antimigraine drugs, such as sumatriptan, are used.
To improve the nutrition of nerve cells - B vitamins (Milgamma, Neurobion, Neurovitan and others).
To eliminate mechanical factors compressing the vertebral artery, the patient may be prescribed physical treatment (manual therapy, post-isometric muscle relaxation) or surgical intervention.
During the recovery period, neck massage, physical therapy, acupuncture, and sanatorium-resort treatment are widely used.
Prevention of vertebral artery syndrome The main preventive measures in this case are an active lifestyle and healthy sleep on comfortable bedding (it is highly desirable that they be classified as orthopedic). If your work involves keeping your head and neck in one position for a long time (for example, working at a computer or activities associated with continuous writing), it is strongly recommended to take breaks from it, during which you perform gymnastics for the cervical spine. If the complaints mentioned above appear, you should not wait for their progression: the right decision would be to consult a doctor as soon as possible.
You can make an appointment with a neurologist by calling: 8(3435)230-500
We care about you!
Always yours, Medical
Diagnosis of vertebral artery syndrome
1. Analysis of the clinical picture of the disease , neurological examination (symptoms of tension in the neck muscles, limitation of movements in the cervical spine, focal neurological symptoms may be identified). Pain often appears when palpating the point of the vertebral artery, located in the suboccipital zone between the transverse processes of the first and second cervical vertebrae.
2. X-ray of the cervical spine in standard projections (direct and lateral) and an additional projection to assess the condition of the atlanto-occipital joint (identification of risk factors for compression of the vertebral artery).
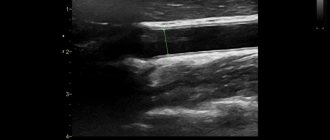
3. Dopplerography (or duplex scanning) of the vessels of the neck and brain (detection of decreased blood flow through the vertebral artery).
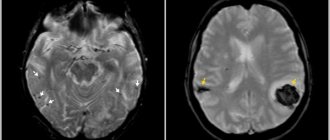
4. If there is a suspicion of an acute cerebral circulatory disorder in the vertebrobasilar region, an urgent magnetic resonance imaging (MRI) of the brain and emergency hospitalization of the patient in a neurological (neurosurgical) hospital is necessary.
5. If there is a high probability of detecting herniated intervertebral discs in the cervical spine, it is recommended to perform magnetic resonance imaging (MRI) of this part of the spine.
Patient's office
Request a call
Symptoms and treatment of vertebral artery syndrome
From this article you will learn: what is vertebral artery syndrome. What diseases lead to the occurrence of pathology. Manifestations of this syndrome and examination methods to establish a diagnosis. Methods for correcting any violations that have arisen.
Vertebral artery syndrome (abbreviated as VAS) is a combination of symptoms from the brain, vascular and autonomic systems that arise against the background of damage to the nerve plexus of the artery itself, deformation of its wall or narrowing of the lumen.
In the medical community, such pathology is usually associated with diseases of the cervical spine, but predisposing factors in some patients are the anatomical features of the artery itself or concomitant vascular diseases, leading to changes in the elasticity of their walls and (or) narrowing of the lumen.
Regardless of the cause, the clinical manifestations of the syndrome are associated with two mechanisms that often combine to worsen the course of the disease:
1. Squeezing, or compression, of the artery leads to disruption of blood flow to part of the brain. 2. Irritation, or irritation, of the nerve fibers that surround the vessel leads to the activation of substances that cause narrowing of the arterial wall. This further disrupts the flow of blood to the structures of the central nervous system.
Negative manifestations of SPA include:
1. increased risk of developing an acute disruption of the blood supply to the brain of a temporary or permanent nature (transient ischemic attack, stroke); 2. decreased ability to work due to the need for a number of restrictions on movement and environmental conditions; 3. significant psychological discomfort against the background of clinical manifestations, especially in young patients.
Carrying out the necessary treatment significantly reduces the manifestations of the syndrome, but does not eliminate it completely.
Even after surgical correction methods, there are often residual effects of the disease, and the need for a restrictive regime of work and rest remains. Therapy significantly reduces the risk of acute vascular manifestations in the brain and the risk of fatal disruption of blood flow. Neurologists and neurosurgeons deal with the problem of diagnosis, choice of tactics for management and treatment of patients with SPA.
Factors that increase the risk of developing
| Group | Immediate factors |
| Features of artery anatomy | Deformation Tortuosity Kink Disturbance of the wall structure Incorrect movement |
| Diseases leading to a decrease in the lumen of the vessel | Atherosclerosis Hypertension Arteritis (inflammation of the wall) Thrombosis and embolism |
Vertebral artery syndrome occurs with the following diseases that cause compression of the vessel:
Osteochondrosis
– pathological destructive changes in the disc between two vertebrae, which begin in the central part (core), progressively spreading to the entire motor part of the vertebra.
Spondylosis deformans
– changes are associated with the aging process of the body, when, against the background of decreased blood flow in the capillaries, the nutrition of the intervertebral discs is disrupted, they lose their elasticity and decrease in size. This leads to the formation of bone spurs (osteophytes) on the front and side of the vertebra.
Spondyloarthrosis deformans
is
a pathology of intervertebral joints that occurs due to occupational hazards or peculiarities of the formation of the musculoskeletal system.
Deforming osteoarthritis of the spine
– one of the elements of systemic destructive damage to the joints of osteoarthritis. Affects two or more motor segments of the vertebrae.
Ligamentosis ossificans (Forestier disease)
– systemic damage to the ligamentous apparatus of the human skeleton, characterized by the deposition of calcium in the ligaments, which progressively reduces their extensibility and mobility.
Kimmerly Anomaly
– pathological structure of the first cervical vertebra.
Basilar impression
– violation of the location of the occipital bone, it is pressed into the cavity of the skull, compressing the spine.
Cervical spine injuries
associated with sudden hyperextension. Compression of the artery by the neck muscles in certain head positions.
Destructive changes in cervical localization of osteochondrosis lead to the development of RAS in 42.5–50% of patients.
Classification
Vertebral artery syndrome is classified according to the main causative mechanism, but in most cases the disease is of a mixed nature.
| Mechanism of occurrence | Its features |
| Compression | Compression of the lumen of the vessel from the outside |
| Irritative | Irritation of the nerve fibers of the perivascular plexus |
| Angiospastic | Reflex narrowing of the artery lumen in response to mechanical activation of receptors in the wall |
| Mixed | Any combination of the above options |
Manifestations of the syndrome
Patients with SPA experience constant difficulties in performing any tasks. Every wrong movement can cause clinical manifestations, forcing the patient to limit himself in work and everyday activities. The symptoms themselves are quite painful and disturb the psychological peace of the sick, forcing them to consult doctors to correct it.
In the clinical course of the syndrome, two phases of development are distinguished:
| Phase | Her characteristics |
| 1. Functional or dystonic | Symptoms are not persistent Good response to treatment Low risk of stroke |
| 2. Organic, or ischemic | The appearance of a focus of persistent disturbance of blood flow High risk of developing acute posterior cerebral stroke The effect of treatment is reduced, residual effects on the brain are possible |
In vertebral artery syndrome, symptoms are highly variable and affect many functions:
| Clinical variant of the symptom | Its manifestations |
| Posterior cervical sympathetic syndrome (Barré-Lieu) | Pain in the neck and back of the head with reflection (irradiation) to the forehead Constant, pulsating pain Intensifies in the morning after sleep, with movement and shaking, sudden turns of the head Noise in the ears Decreased hearing Flashes before the eyes |
| Basilar migraine | The attack begins with changes in vision (sparks, loss of part of the image) Severe dizziness and gait disturbance Incoherent speech Tinnitus Pain in the back of the head |
| Vestibulo-atactic syndrome | Impaired gait and balance Nausea and vomiting Dizziness Darkness in the eyes Rapid pulse Increased blood pressure |
| Cochleovestibular syndrome | Hearing loss Tinnitus that changes when you turn your head Unsteadiness when walking Swaying |
| Visual or ophthalmic syndrome | Flashes, flickering before the eyes Deterioration of vision Tearing Rapid eye fatigue Redness of the eyes Feeling like “sand has been poured into the eyes” Periodically loss of part of the visible image |
| Autonomic dysfunction syndrome | Feeling hot or cold Increased sweating Cold feet and hands Difficulty swallowing Voice problems Insomnia or drowsiness |
| Vertebral syncope (Unterharnscheidt) syndrome | A short attack of loss of consciousness during certain movements of the neck or prolonged stay in an uncomfortable position |
| Transient ischemic attack | Impaired active movement of the limbs Changes in skin sensitivity Loss of vision Loss of balance when walking Dizziness with nausea and vomiting Double vision Inability to speak and swallow |
| Drop attack attacks | Sudden paralysis of the whole body with a fall after throwing back the head. The duration of the attack is from several seconds to a minute |
| Mental changes | Unpleasant sensations of foreign material in the upper half of the body Refusal to eat Decreased all types of activity Thoughts about a fatal disease and the inability to recover from it |
The disease can manifest itself in only one of the listed options or a combination of them.
Diagnostics
Vertebral artery syndrome is a multifaceted disease that often imitates various pathologies of the organs of vision, hearing, neck, and brain.
Therefore, the main method of establishing the correct diagnosis is a thorough interview of the patient to identify the prevailing syndrome of the disease. To clarify the cause of the pathology, a number of additional procedures are required:
| Study | Target |
| X-ray of the cervical spine and skull bones with functional loads | Primary assessment of bone elements Identification of gross skeletal pathology |
| Ultrasound scanning of the vessels of the neck and head | Inspection of the artery itself for anatomical changes, pathology of the wall and lumen, identification of compression and kinks of the vessel |
| Multislice computed tomography | Assessment of all bone structures, identification of pathology associated with the destruction of elements of the spinal column |
| Magnetic tomography of the cervical spine and blood vessels of the head and neck | Assessment of “soft” skeletal elements (discs, ligaments), identification of pathology from the artery itself and its branches |
| Angiography | A clarifying method in complex diagnostic situations. Indicated for suspected blockage of an artery by a blood clot to select subsequent treatment. |
Treatment
Treatment of vertebral artery syndrome includes both medicinal effects on the vessels and surrounding tissues, and surgical methods for correcting compression by the bone structures of the vertebrae. There is no complete cure for the disease, since pathological processes in the elements of the spinal column are irreversible .
But a complex effect on all elements of the mechanism of occurrence makes it possible to slow down and (or) stop changes, as well as reduce the clinical manifestations of the syndrome.
Medicinal methods of correction
1. Drugs to relieve swelling and inflammation
When the lumen of the bone canal decreases, the venous vessels are the first to be compressed, and against the background of impaired blood outflow from the brain, increased compression of the vertebral artery occurs. Any prolonged compression leads to a local inflammatory reaction. Therefore, spa treatment begins with these medications:
— Troxerutin; — Diosmin; — Nimesulide; — Celecoxib; - Lornoxicam.2. Medicines that normalize blood flow in the arteries Against the background of disruption of the normal blood supply to brain structures, the risk of stroke and transient attacks increases. To prevent complications use: - Pentoxifylline; — Vinpocetine; — Cinnarizine; — Nicergoline; - Instenon. 3. Drugs to protect nerve cells Under conditions of lack of blood flow, neurons are exposed to free radicals and suffer from a lack of oxygen. Medicines from this group are indicated in the phase of organic disorders in SPA in order to prevent the development of persistent impairment of brain function. — Citicoline; — Gliatilin; — Actovegin; - Cerebrolysin; — Piracetam; — Mexidol; - Mildronate; - Sumatriptan; — B vitamins; - Antispasmodics. 4. Non-medicinal treatment is aimed at relieving spasm of the muscles surrounding the spine and improving blood flow in this area - massage; - acupuncture; - PRP therapy; - physiotherapy (UHF, shock wave, HILL laser, magnet, amplipulse); — therapeutic exercises and physical education; - sanatorium treatment.
Surgical correction
To relieve pressure on the artery, a number of techniques are used to normalize the supporting function of the spinal column:
1. Percutaneous spinal fusion
– fixation of two adjacent vertebrae relative to each other
2. Fenestration of discs between vertebrae
– creation of artificial defects in them for the growth of connective tissue
3. Autodermoplasty of discs
– replacement of the intervertebral disc with one’s own tissues
4. Replacement of the disc
with a titanium-nickel explant
Forecast
Prognosis Vertebral artery syndrome cannot be completely cured. This is due to causal pathological factors - changes in the osteoarticular component of the spinal column do not undergo reverse development. Any surgical techniques provide a temporary or incomplete therapeutic effect. Drug correction is aimed at reducing the clinical manifestations of the disease, but has virtually no effect on the primary cause of the pathological process. Despite this, all treatment methods significantly alleviate the course of the disease and stop its progression.
Treatment of vertebral artery syndrome