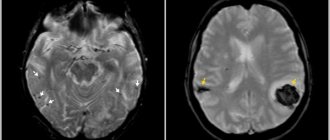
Every fourth stroke develops in the posterior parts of the brain in the area of responsibility of the vertebral arteries. Atherosclerosis and narrowing of the vertebral artery
can occur in any part of it and can cause ischemic stroke. Unlike narrowing of the carotid arteries, the role of which in the development of stroke has been known for a long time and methods for their treatment have been developed, the pathology of the vertebral arteries has not yet been sufficiently studied. However, modern technologies for diagnostic testing and endovascular treatment methods have opened up new opportunities for intervention in this disease.
Vertebral artery syndrome is a condition associated with obstruction of the patency manifested by symptoms of cerebrovascular insufficiency in the posterior part of the brain.
The causes of impaired patency can be very different, so the main task in the management of patients is an accurate diagnosis, so that as soon as the identification of the exact cause will allow it to be eliminated and the symptoms that are painful for patients to be removed. Every year the disease becomes younger, which is associated with an increase in the number of young people who sit for long periods at computers and have a sedentary lifestyle.
Timely diagnosis guarantees a favorable result of treatment of vertebral artery syndrome in our clinic.
Causes of vertebral artery syndrome
The most common cause of vertebral artery circulatory disorders is atherosclerotic plaque. Less common are stratification (dissection) of the artery, compression of it in the neck or at the entrance to the skull, and inflammatory diseases (vasculitis). It is quite difficult to accurately determine the likelihood of developing a stroke with such a localized lesion. According to anatomical studies, damage to the vertebral arteries during death from ischemic stroke was observed in 12% of cases.
Damage to the intracerebral parts of the vertebrobasilar system more often leads to ischemic strokes than narrowing of the artery in the neck. The risk of developing ischemic events with such lesions is about 7% per year. Symptoms of vertebral artery syndrome are being diagnosed more and more often. Many factors influence the development of the syndrome. It usually represents a combination of cerebrovascular arteriosclerosis and cervical spondylosis (degenerative changes in intervertebral disc tissue) as the main clinicopathological components.
Material and methods
The study included 1500 patients with complaints of headache (950 women and 550 men, average age 42 ± 7.4 years) who were treated in the departments of neurology and therapy of the Clinical Hospital. S.R. Mirotvortsev SSMU in the period from October 2013 to May 2021.
Triplex scanning of the brachiocephalic arteries (TS BCA) according to the standard method was carried out on a stationary expert-class device Philips HD11 XE with linear (3–12 MHz) and convex (2–5 MHz) sensors on the basis of the department of ultrasound and functional diagnostics.
The diameters of the PA in the 2nd segment were assessed. Blood flow indicators in hypoplastic VAs were analyzed in segments 1–2. A hypoplastic VA was considered to be less than 2.0 mm in diameter. A PA diameter in the range between 2.0 and 2.5 mm was considered small.
Forecast
With atherosclerosis of the vertebral artery, it is quite difficult to give a prognosis for the life and health of the patient. With large narrowings, blood flow is compensated by the second vertebral artery; in addition, there is collateral blood flow. There have not yet been large studies assessing the risk of stroke with damage to the vertebral arteries. However, the fact remains that strokes in the vertebrobasilar system account for at least 25% of all strokes and are much more severe than strokes associated with the carotid artery. Therefore, the identification of significant narrowing of the vertebral artery should be a reason to eliminate this risky condition.
Without identifying and eliminating the causes of the development of vertebral artery syndrome, the prognosis for recovery is unfavorable. Most often, the patient's condition gradually worsens, which negatively affects the quality of life.
The most difficult thing is to identify the exact cause. Knowing the cause will allow it to be eliminated surgically or endovascularly and relieve the patient from painful symptoms.
A fascinating “walk” through the veins and arteries
I bring to your attention an article about a medical diagnostic procedure - duplex scanning of blood vessels.
Duplex scanning of blood vessels, otherwise known as vascular Doppler ultrasound (USDG), is essentially an ordinary, familiar, well-known ultrasound scan.
Many patients undergoing medical examination are prescribed an ultrasound examination of the brachiocephalic vessels. I will try to talk about the essence of this study, what information it gives to your attending physician, and why this study was included in the list of diagnostic measures for medical examination of the adult population.
So, as a “tour guide,” I invite you to a short and, I hope, educational journey through the veins and arteries. The study is called duplex because it combines two modes - a two-dimensional image and a Doppler mode - a study based on measuring blood flow velocity. The 2D image looks like this.
This is a familiar black and white image, or rather gray, in which the manufacturers of modern ultrasound scanners promise not just 50, but as many as 256 shades! Doppler is a mode for studying blood flows, their speed and direction. It is the inclusion of the Doppler that is accompanied by the appearance of somewhat unusual sounds during the examination, sometimes slightly frightening to patients. These sounds are a kind of interpretation of the characteristics of blood flow. Each artery has its own “melody”. The external sleepy one is harsh and rough, the internal sleepy one is softer and more pleasant. And the veins generally “sound” like a light breeze.
This is what duplex scanning looks like on the monitor.
There is a color doppler that adds bright colors to a boring black and white picture. Patients, having seen the image, are usually interested in what is “red” and “blue” there?
Both “red” and “blue” are blood. The color depends only on the direction of blood flow relative to the sensor. What moves towards the sensor is colored red, what moves away from the sensor is colored blue.
This is no longer a duplex, but a triplex study. Actually, any modern ultrasound examination is triplex, but the name “duplex” has been preserved as more familiar.
Vascular examination is harmless to the patient, non-invasive (no penetration into the body) and does not require prior preparation. And now a little about the study of the brachiocephalic arteries (BCA), the same study that is included in the list of studies under the clinical examination program.
Brachiocephalic arteries is a definition that includes the carotid and vertebral arteries. The carotid arteries have nothing to do with the quality of sleep. They owe their unusual name to a small anatomical formation on the internal carotid artery. This formation, or rather the expansion of the artery, is called the carotid or carotid sinus. If you squeeze the neck in the area of this sinus, the number of heart contractions decreases, the person seems to fall asleep and may even lose consciousness. This is where the name carotid arteries comes from.
The examination is performed with the patient lying on his back, sometimes with a cushion under the neck for better vision of the arteries with the sensor.
This is what the common carotid artery looks like on an ultrasound scanner.
The carotid arteries can tell a lot of interesting things about a person. First of all, we are interested in the diameter and shape of the arteries, as well as the presence of atherosclerotic plaques that are dangerous to human health. The presence of atherosclerotic plaques or the predisposition of blood vessels to their appearance is indicated by such an indicator as the thickness of the “intima-media” complex or, in other words, the thickness of the inner layer of the vascular wall.
IMM thickness is an indicator of the severity of the atherosclerotic process in the body. Normally, it should be no more than 1.0 mm. The intima is a thin white stripe, the media is a thin black stripe following the intima, and the dark inside is the lumen of the artery.
The following image shows a vessel that is not affected by atherosclerosis. The thickness of the intima-media complex is 0.6 mm. The blue line is drawn along the inner layer of the vascular wall - the intima.
But in the next image, the intima-media complex, in other words, the vessel wall, is already thickened (1.4 mm) - these are already manifestations of atherosclerosis.
As atherosclerosis progresses, the intima-media complex not only thickens, but atherosclerotic plaques form, which cause narrowing (stenosis) of the vessel. The degree of stenosis is expressed as a percentage. Atherosclerotic plaques look something like this. This is the site of bifurcation (branching) of the common carotid artery (CCA) into its two branches - the internal carotid artery (ICA) and the external carotid artery (ECA). Arterial branching sites are favorite sites for the appearance of atherosclerotic plaques. I outlined the contours of the vessel itself in blue, and the atherosclerotic plaque in red. The degree of vasoconstriction in this patient is about 30%.
And in the next two pictures the process is already more advanced, the degree of narrowing of the vessel is 68%. The blue outline shows the vessel itself, and the red outline shows what the lumen of the vessel has become, changed due to atherosclerosis.
Atherosclerotic plaques can be extremely dangerous. Increasing in size, the plaque impairs blood flow in the vessel, up to its complete blockage. In addition, sometimes a fragment of atherosclerotic plaque can break off and block a smaller blood vessel, thus causing a stroke or heart attack.
If complicated plaques are detected and with a pronounced degree of narrowing of the vessel, a consultation with a vascular surgeon is indicated to decide on surgical treatment. If the process is moderate, the doctor prescribes treatment with statins - drugs that strengthen the surface of the plaque and prevent its destruction. It is also necessary to control your blood cholesterol levels, correct your diet and get rid of bad habits.
It is generally accepted that if atherosclerotic plaques are detected in the carotid arteries, then in the coronary arteries - those that feed the heart, there is almost one hundred percent probability that they are also present. We cannot easily and simply look into the arteries of the heart. Coronary angiography, the study of the blood vessels of the heart, is a complex study performed in a hospital setting. Therefore, ultrasound examination of brachiocephalic vessels (neck vessels) is a simple and informative method for diagnosing atherosclerosis. It is believed that atherosclerosis develops if a person has elevated levels of “bad” cholesterol - low-density lipoproteins.
To paraphrase popular wisdom, we can say that by the age of 50 every man should plant a tree, raise a son, build a house and... check his cholesterol level. It is advisable for a man who smokes to pay attention to his cholesterol by the age of forty. The same recommendations apply to representatives of the fair sex. In addition to the carotid arteries, vertebral arteries are also available for study. At the level of the sixth cervical vertebra, the vertebral arteries enter the bony canal formed by the transverse processes of the cervical vertebrae. Sometimes the artery enters the bone canal higher, at the level of the fourth or even third cervical vertebra.
The vertebral artery with a diameter of 3 mm is shown in the following image. Its walls are highlighted with blue lines. Dark vertical formations that interrupt the course of the artery are transverse processes of the cervical vertebrae. Ultrasound does not penetrate bone tissue, so the artery wall is not visible in these areas.
The vertebral arteries (VA) are smaller in diameter than the carotid arteries. The normal size is considered to be a diameter of 3 mm, if less than 3 but more than 2, this is called a “small” diameter, and less than 2 mm is already hypoplasia (underdevelopment) of the artery. This is a congenital condition, and it is impossible to influence the diameter of the arteries. When hypoplasia of the vertebral artery is detected on one side, the vertebral artery on the other side is usually increased in diameter. This ensures balance and ensures adequate blood supply to the brain. In addition to the diameter, we evaluate the shape of the arteries and the presence of tortuosity. The photo below shows an artery with a deformed course. It can be seen that the artery is curved, and this arc is painted in different colors.
Sometimes there are simply arteries curled into a ring! How can you avoid getting sick or dizzy with these? The vertebral vein runs parallel to the vertebral artery and above it in the bone canal. Blood in veins and arteries moves in different directions, so the vessels are painted in different colors.
Typically, the vertebral vein does not appear so bright and deep blue on an ultrasound. As a rule, it is slightly stained. Such brightness and expressiveness is already a bit of a pathology, which in conclusion is reflected in the phrase “difficulty of venous outflow.” This is not a disease yet, but rather a feature of the patient’s venous tone. But this condition already requires treatment, since it often manifests itself as tedious headaches and heaviness in the head. Remember what the doctor said from the movie “Formula of Love”? “The head is a dark object and cannot be examined.” A hundred years ago, maybe it was like that. Well, now it is very possible, and ultrasound examination of the brachiocephalic vessels (neck vessels) is an informative and safe diagnostic method that allows one to obtain important information about the blood supply to the brain.
It is enough just to do the research during medical examination. An ultrasound examination of the carotid and vertebral arteries at the second stage of clinical examination is prescribed to everyone who has elevated cholesterol levels or has complaints as prescribed by a neurologist.
Davidenko Yulia Gennadievna, head of the functional diagnostics office of the polyclinic of OKB No. 3.
Advantages and disadvantages of the procedure
Today, almost every medical institution has the necessary equipment to conduct ultrasound of the neck vessels. Let's consider the advantages of this technique:
- This method is absolutely safe;
- The procedure can be performed at any age;
- She has no direct contraindications;
- The process is absolutely painless and does not cause discomfort.
- The only disadvantage we can note is the lack of information content - this is not the main method of diagnosing diseases, but only an auxiliary one.
Symptoms of the disease
Hypoplasia of the left vertebral artery is not as common as the right one. Therefore, when discussing the clinical manifestations of their damage, attention is primarily focused on damage to the right vertebral artery. Manifestations of decompensated disturbance of blood flow through this vessel are reflected in the table.
| General cerebral symptoms |
|
| Focal symptoms of vascular disorders in the cerebral hemispheres |
|
| Focal symptoms of damage to the occipital lobe of the brain |
|
| Stem and autonomic reactions | Instability of blood pressure with its strong changes. |
| Cerebellar disorders |
|
Typically, manifestations of hypoplasia of the right vertebral artery develop gradually. These do not have to be all the symptoms listed in the table. The patient can note only some of them, which depends on which part of the brain at a particular moment feels the greatest circulatory deficiency. Symptoms are transient, periodically exacerbating and then subside. This intermittent course masks the true problem under the guise of any other diseases (neurocirculatory dystonia, dyscirculatory encephalopathy, etc.). In case of prolonged uncorrected progression of brain damage symptoms, there is a high risk of developing pre-stroke conditions or even stroke. Therefore, it is extremely important to detect the true problem in time.
Symptoms of hypoplasia of the right vertebral artery are not specific and can be observed in any disease that leads to disruption of normal blood supply and brain function. The diagnosis can only be established using special diagnostic methods.
Diagnostics
It is carried out under the supervision of a neurologist; if necessary, a specialized surgeon is involved.
The examination is quite simple, gives high-quality results immediately, not counting difficult situations.
Among the events:
- Oral interview with the patient. To record complaints, make a list of symptoms and put forward hypotheses.
- Anamnesis collection. Doctors are especially interested in the course of pregnancy in the mother, if such data is available. To a lesser extent, lifestyle, habits, hereditary factor.
- Dopplerography of the vessels of the neck and brain. Also duplex scanning. Studies aimed at visualizing tissues, assessing the speed of blood flow and its quality. Determination of violations, their severity, localization. Can be carried out with functional tests. Turning the head, etc. This gives a more complete picture.
- Angiography. Of necessity. For visualization of blood vessels.
- The same effect is achieved through MRI, only the level of detail is many times higher. Appointed in controversial cases.
- General blood test and biochemistry with an expanded picture of the lipid spectrum. As part of the diagnosis of atherosclerosis. Allows you to detect excess cholesterol and other fatty compounds. Which can become the culprit of the disease.
It's enough. If necessary, consultations with other specialists are indicated, but these are speculative individual cases. Other scenarios are unlikely.
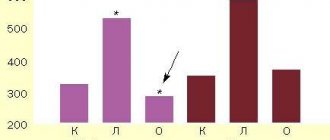
results
VA hypoplasia was detected in 44 (2.9%) patients (min diameter – 0.9 mm; max – 1.95 mm; mean diameter – 1.71 mm). In one of the cases, a 19-year-old patient was found to have hypoplasia of both VAs. On the left side, VA hypoplasia was more common (31 patients, 2.1%) than on the right (13 patients, 0.8%).
In 43 cases, the diameter of the contralateral VA was several times greater than the diameter of the hypoplastic VA (min – 3.2 mm; max – 6.3 mm; average diameter – 4.8 mm). There was no correlation between the detection of hypoplastic PA and gender.
Peak systolic velocity (PSV) of blood flow at the level of segments 1–2 in hypoplastic VAs did not exceed 43 cm/s (min – 9 cm/s; average PSV – 31.5 cm/s). It should be noted that only 7 (16% of the total number of cases with hypoplastic VA) patients with hypoplastic VA had a complaint of dizziness. There was no correlation between VA hypoplasia and headache complaints. Small VA diameter was found in 290 (19.3%) patients (average diameter 2.38 mm). The average PSC in a small-diameter PA is 40.5 cm/s.
What is the essence of the disease
It is impossible to understand pathology without knowing the norm. The brain receives blood from two large vascular systems: the internal carotid and vertebral arteries. Each of these vessels is paired and brings blood to a specific area of the right or left hemisphere of the brain. The junction of the terminal branches of these two arteries is called the Circle of Velisius. This is a very important anatomical formation that provides compensation for blood flow if one of the main vessels is blocked for some reason. Thus, the brain has the ability to self-regulate its blood flow, protecting itself from oxygen starvation and damage.
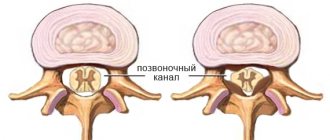
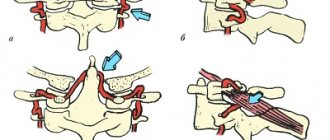
The right vertebral artery, as one of the powerful components of the circle of Velisius, departing from the subclavian artery, enters the spinal canal of the transverse processes of the cervical vertebrae and is directed along it into the cranial cavity. At the same time, it makes several strong bends, passing through narrow, inert holes. The area of its branching and blood supply is represented by the structures of the posterior cranial fossa of the corresponding side (cerebellum, medulla oblongata, occipital lobe of the hemispheres).
When talking about hypoplasia of the right vertebral artery, we mean its congenital underdevelopment and narrowing of the diameter. Naturally, under such conditions, the corresponding areas of the brain will be deprived of normal blood supply. If such a pathology is combined with an open circle of Velisium, there is an extremely high risk of severe ischemic (stroke) brain damage.
Main causes and symptoms
The causes of the disease are related to the intrauterine development of the child:
- bruise and injuries to the expectant mother,
- excessive use of alcohol, drugs,
- nicotine addiction;
- irradiation with certain types of gamma rays, with prolonged overheating;
- infectious diseases: influenza, rubella, toxoplasmosis.
Hypoplasia of the left or right vertebral artery leads to the gradual onset of symptoms, making it very difficult to diagnose.
Among the main signs of the disease are:
- frequent dizziness;
- causeless pain in the head;
- decreased sensitivity of individual parts of the body;
- deterioration of movement coordination;
- decreased vision and hearing;
- deterioration of attention, memory and concentration.
All of these symptoms occur with varying frequency. They are characteristic of pathology of the left or right vertebral artery of prolonged development. At the same time, patients often experience sudden changes in mood, depression, severe weakness and fatigue. Weather dependence may also appear when a person begins to feel unwell due to temperature changes and changes in atmospheric pressure. In addition, sleep disturbance may occur.
With the development of this disease, a significant narrowing of the vascular lumen occurs in the area where it enters the bone canal leading into the cranial cavity. As a result, insufficient blood begins to flow into the brain. This factor explains hemodynamic abnormalities in VA underdevelopment.
Any symptoms that arise in the presence of pathology are caused by the fact that the vertebral arteries supply the brain with nutrients and nourishment, and even minor disturbances in their work are manifestations of deterioration in cerebral blood flow. Over the years, the symptoms intensify, and this is not surprising: the vessels begin to lose elasticity and become “clogged.” Therefore, the lumen narrows even more.
The small diameter of the PA can be on the right side or on the left. Hypoplasia of the right vertebral artery is observed in almost 10% of citizens. Diseases of the left VA are much less common.
Treatment
Treatment is carried out using two methods:
- Conservative. It involves the introduction of drugs that improve blood properties, blood supply to the brain and metabolic processes in it. Such methods do not completely eliminate the disease, but only provide protection to the brain from ischemic abnormalities. For this purpose, various medications are used, in particular blood thinners.
- Surgical. Used in situations where it is impossible to compensate for cerebral circulation in other ways. Experienced surgeons perform endovascular surgery, the meaning of which is to insert a stent into the lumen of a narrowed vessel. This is a special dilator that increases the diameter of the artery, normalizing blood flow.