General information
What is vertebral artery hypoplasia?
Hypoplasia of the right vertebral artery and hypoplasia of the left vertebral artery are an abnormal decrease in the lumen of these arteries (approximately to a diameter of less than 2 mm).
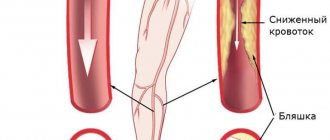
But there is no single criterion for narrowing the diameter of the vessel, and a number of authors include a decrease in the diameter of the vessel of less than 3 mm as signs of VA hypoplasia. The right vertebral artery is a branch of the right subclavian artery, which arises from the brachiocephalic trunk, and the left one arises from the left subclavian artery, which originates from the aortic arch. Next, both vertebral arteries (VA) rise in the bone canal to the brain and merge in the cranial cavity, forming the basilar artery. The vertebral arteries supply 15–30% of blood to the structures of the brain stem, the temporal/occipital lobes, the cerebellum, the hypothalamic region, and segments of the spinal cord, that is, they play a significant role in ensuring blood flow to the brain structures. Below is a picture of hypoplasia of the right/left VA.
Hypoplasia is one of the most common pathologies of the vertebral arteries. Its occurrence in the population, according to various sources, varies widely between 2.34% and 26.5% and is predominantly congenital in nature. Hypoplasia of one of the arteries occurs predominantly; cases of bilateral hypoplasia of the VA are relatively rare. The main place of narrowing of the lumen of the vertebral arteries is the place of entry into the bone canal (in the cranial cavity), which leads to a significant decrease in blood flow mainly to the posterior parts of the brain with the gradual development of non-vertebrogenic PA syndrome .
Hypoplasia of the vertebral artery is a factor in a significant reduction in blood circulation in the vertebrobasilar region, which disrupts the hemodynamics of the brain as a whole, increasing the risk of developing ischemic stroke (acute cerebrovascular accident). The situation is sharply worsening against the backdrop of the development of cerebral atherosclerosis , which is extremely common in the population due to poor lifestyle and especially dietary habits.
Variations in the development of cerebral arteries and epilepsy
The prevailing ideas about the mechanisms of development of cerebral ischemia imply the occurrence of a discrepancy between the available blood supply and the needs of brain tissue. The most important achievements in the field of clinical angioneurology include the modern concept of heterogeneity of ischemic stroke, which is based on the idea of the diversity of causes and mechanisms of development of acute focal ischemic brain damage. The amount of reversible and irreversible brain damage largely depends on the state of the hemodynamic, collateral, perfusion and metabolic reserves of the brain. Pathological tortuosity of the main arteries of the head - a hereditarily determined functional inferiority of connective tissue - occurs in at least 10% of the population. Among the main forms of lesions of intracranial arteries, kinks and loop formations, aneurysmal dilatations of arteries, and arteriovenous aneurysms are distinguished. Excessive tortuosity of blood vessels contributes to the formation of blood clots in them. In 71% of patients with arterial occlusion, a tortuous course of vessels was noted. Underdevelopment of the cerebral arteries in the form of hypoplasia or stenosis of the posterior inferior cerebellar artery and/or basilar artery, rarely the inferior anterior cerebellar artery and tortuosity of the vertebral artery are causes of hearing loss and deafness. Weak cerebral artery anastomoses cause cerebral ischemia after cervical discectomy. In Parkinson's and Alzheimer's diseases, neuroimaging and pathological studies have detected cerebrovascular lesions in 20-30% of cases, and vascular disease of the brain may be the basis of dementia. Structural changes in cerebral vessels, a decrease in blood flow velocity and the presence of 30% stenosis in the middle cerebral artery can be prerequisites for the development of stroke in patients with sleep apnea syndrome.
In case of Kimmerle anomaly, it is necessary to take into account the presence of congenital changes in the vertebral arteries. Dysplastic disorders in the area of the craniovertebral junction are 2 times more often noted with pathological tortuosity of the vertebral arteries, to a lesser extent due to hypoplasia of the vertebral arteries. Up to 51.9% of patients with Chiari malformation and syringomyelia have structural features of the cerebral arterial circle. Tortuosity, asymmetry and hypoplasia of the vertebral arteries with signs of impaired blood flow are characteristic of vertebrobasilar insufficiency due to cervical dorsopathy and were noted in 76.6% of cases with central vestibulocochlear syndrome.
The arterial bed of the brain is also affected in such systemic diseases of the body as rheumatoid arthritis, polyarteritis nodosa, Takayasu's disease, Henoch-Schönlein disease. When performing dental procedures in patients with Sturge-Weber disease or Recklinghausen disease, as typical neurofibromatosis, the development of threatening bleeding is possible. Primary damage to the cerebral arteries in the form of vasculitis and endarteritis underlies the development of neurosyphilis and leads to secondary damage to the nervous tissue and the occurrence of infarctions in the brain. Cerebral vasculitis and herpetic cerebral vasculitis can develop against the background of herpetic infection. With ischemic strokes, in 70% of cases in the brain tissue, along with changes caused by acute cerebrovascular accident, focal lesions are observed, similar to changes in meningoencephalitis caused by herpes zoster and herpes simplex.
Changes in the structure of the cerebral arteries must be taken into account when assessing cancer metastases, as well as in 40% of patients with severe traumatic brain injury when identifying traumatic subarachnoid hemorrhages and concomitant angiographic vasospasm.
In the course of carrying out research to study the relationship between variants of human cerebral arteries and cerebrovascular disorders within the framework of acute cerebrovascular accidents and chronic cerebral ischemia, we have developed observations about the relationship between variants of the structure and topography of human cerebral arteries with a number of other nosological units. In this regard, we present the results of our own research on the development of cerebral arteries in humans with various types of epilepsy.
We analyzed the state of the arterial bed of the brain in 748 outpatient and inpatient patients from 22 years to 81 years old, who were examined and treated in the neurological and neurosurgical departments of OKB No. 2 named after. Professor I.N. Alamdarov, Astrakhan in the period 1983-1998, the neurological departments of City Hospital No. 3 and City Hospital No. 4 of Tambov, the neurosurgical department of the Tambov Regional Hospital, the rehabilitation and health complex of the family “B. Lipovitsa", neurological offices and in day hospitals of City Hospital No. 4, Nodal Clinic at the station. Tambov JSC "Russian Railways" and the Central House of Children's Hospital "Tambovmedservice" LLC, as well as in the outpatient clinic "Home Doctor" (Tambov) during 1998-2009.
All patients underwent a comprehensive clinical and instrumental study, including data from a clinical examination by a neurologist, therapist and ophthalmologist, standard laboratory data, electrocardiography, fluorography or plain radiography of the chest organs. According to indications, consultations and examinations were carried out with a neurosurgeon, gynecologist, otolaryngologist, cardiologist, endocrinologist and psychotherapist; a study of the cognitive sphere using a brief mental status assessment scale or a mini-mental status study, transcranial Doppler sonography, electroencephalography. All patients underwent magnetic resonance imaging (MRI) and magnetic resonance angiography (MRA).
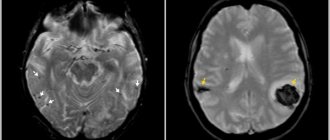
According to the data obtained, variants of the structure and topography of the arterial circle of the cerebrum were verified in only 27 cases (61.4% of observations) out of 44 patients with epilepsy or encephalopathies with leading epileptiform syndromes. Among the analyzed group of patients with various types of epilepsy, the following variants of the structure and topography of the arterial circle of the cerebrum were identified: 1) bending of both anterior cerebral arteries in 1 (3.7%) patient; 2) hypoplasia of the left vertebral artery in 2 (7.4%) patients; 3) posterior trifurcation of both internal carotid arteries and anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 3 (11.1%) patients; 4) anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 6 (22.2%) patients (Fig. 1); 5) hypoplasia of the right vertebral artery, aplasia of the posterior communicating artery on the right in 4 (14.8%) patients; 6) hypoplasia of the right vertebral artery, hypoplasia of the basilar artery in 5 (18.5%) patients (Fig. 2); 7) anterior trifurcation of the left internal carotid artery, hypoplasia of the posterior communicating artery, hypoplasia of the right posterior cerebral artery in 3 (11.1%) patients; tortuosity of both vertebral arteries in 2 (7.4%) patients; 9) hypoplasia and tortuosity of both vertebral arteries in 1 (3.7%) patient. Below are quite indicative clinical observations from the totality of our own studies.
Among the analyzed group of patients with various types of epilepsy, the following variants of the structure and topography of the arterial circle of the cerebrum were identified: 1) bending of both anterior cerebral arteries in 1 (3.7%) patient; 2) hypoplasia of the left vertebral artery in 2 (7.4%) patients; 3) posterior trifurcation of both internal carotid arteries and anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 3 (11.1%) patients; 4) anterior trifurcation of the left internal carotid artery, hypoplasia of the basilar artery in 6 (22.2%) patients (Fig. 1); 5) hypoplasia of the right vertebral artery, aplasia of the posterior communicating artery on the right in 4 (14.8%) patients; 6) hypoplasia of the right vertebral artery, hypoplasia of the basilar artery in 5 (18.5%) patients (Fig. 2); 7) anterior trifurcation of the left internal carotid artery, hypoplasia of the posterior communicating artery, hypoplasia of the right posterior cerebral artery in 3 (11.1%) patients; tortuosity of both vertebral arteries in 2 (7.4%) patients; 9) hypoplasia and tortuosity of both vertebral arteries in 1 (3.7%) patient. Below are quite indicative clinical observations from the totality of our own studies.
Example 1. Patient N., 54 years old, is observed in the Nodal clinic at the station. Tambov JSC "Russian Railways" with a diagnosis of encephalopathy as unspecified (epileptic and dyscirculatory) with polymorphic paroxysms (like Todd's palsy) against the background of abnormalities in the structure of the cerebral arteries. Complaints of noise in the head, unsteadiness when walking, attacks of weakness in the right limbs and loss of consciousness. Neurologically: there are no meningeal signs in consciousness, cognitive functions are reduced, emotionally labile, pupils d = s, convergence is weakened, slight weakness of the facial muscles on the right, paresis of the right hand up to 4 points, no sensory disorders, tendon reflexes are increased d > s, staggering in the Romberg position , coordination tests are performed with DetS missing, eyelid tremor. Ophthalmologist: hypertensive angiosclerosis of the retinal vessels of both eyes. Therapist: stage II hypertension, severity of arterial hypertension II, risk category 3. BAC: cholesterol - 4.5 mmol/l, β-lipoproteins - 3.5 g/l, creatinine - 69 µmol/l, urea - 7, 9 mmol/l. Prothrombin - 88%, fibrinogen - 4.25 g/l. ECG: syn, rhythm 80 per minute, normal position of the EOS. MRI and MRA: shown in Figure 1. Outpatient treatment: piracetam, glycine, Cavinton, cinnarizine, aminalon, Enap, Prestarium, indopamine. She underwent a course of treatment in a day hospital: Mexidol, magnesium sulfate, Prestarium, indopamide, mildronate, enalapril. The complaints remain the same. Neurologically - there are no meningeal signs in consciousness, cognitive functions are reduced, cranial nerves without dynamics, paresis of the right hand up to 4.5 points, staggering in the Romberg test, coordination tests with intention on both sides. Consulted at the Tambov psychiatric hospital, where a diagnosis was made: consequences of organic damage to the central nervous system of complex origin with polymorphic paroxysms. EEG: pronounced cerebral changes in biological and bioelectrical activity, practically no α-activity. In all regions the polyri is less than 5 μm. There is no regionality, no activation reaction, no assimilation. Persistent disorganization of the activities of central structures. Interest in the left temporal region, where a focus of slow-wave irritation was identified. Low functional state of the cortex with high sensitivity to hypoxia, with a decrease in the threshold of excitability of the trunk. Single discharges of the posterior trunk sections. Vascular influences are pronounced. Follow-up: while taking Depakine-Chrono, complaints decreased significantly, no attacks were noted.
Example 2. Patient VN., 21 years old, is observed in the Nodal clinic at the station. Tambov JSC Russian Railways with a diagnosis of epilepsy with polymorphic cerebral paroxysms and cognitive impairment. Observed since childhood - complaints of attacks with loss of consciousness. After starting treatment at the age of 14 in the neurological department of the Tambov Regional Children's Hospital, he was registered with a diagnosis of epilepsy, partial seizures with secondary generalization. EEG (Psychiatry and Narcology, 04/17/02): no paroxysmal activity was detected, unstable α-rhythm. Dysfunction of the diencephalic region. Vascular influences with increased autonomic excitability (06/15/04): AMI is moderate, but persistent, with low-amplitude dysrhythmia. Regionality is unclear. The activation reaction is reduced, there is no assimilation. No gross slow-wave or paroxysmal activity was detected. Reduced reactivity of the cortex. High vegetative excitability. Vascular influences 02.22.05: compared to 06.15.04, positive dynamics. General cerebral changes are moderate and of a regulatory nature. Moderate dysfunction of the diencephalic region with increased activity. An unstable α-rhythm appeared, fragmented. The reactivity of the cortex has improved. The sensitivity of the cortex to RFS has increased somewhat, which leads to a decrease in the threshold of excitability of the posterior brainstem structures. There are no paroxysmal tendencies of the cortex. Increased autonomic excitability. MRI and MRA: shown in Figure 2. Neurologically: there are no meningeal signs in consciousness, cognitive functions are slightly reduced, emotionally labile, distal hyperhidrosis, tremor of the eyelids and outstretched fingers, pupils d = s, converges, weakness of facial muscles on the right, in the Romberg position lung staggering, performs coordination tests, paresis, no sensory disorders, tendon reflexes d = s, Babinski's symptom is weakly positive on both sides, Epileptologist: cognitive disorders due to epilepsy. He constantly receives finlepsin (attacks are associated with irregular use of the drug).
Thus, we consider it necessary to draw the following conclusions. 1. Variations in the structure and topography of the arterial circle of the cerebrum can be considered as predictors of epileptiform phenomena in brain structures. 2. For various cerebral paroxysms, it is obviously advisable to study the arterial circle of the cerebrum. 3. Variants of the structure and topography of the arterial circle of the cerebrum in each specific case should be considered from the point of view of minor developmental anomalies.
Pathogenesis
Currently, hypoplasia of the vertebral arteries is considered as one of the manifestations (during the formation of the fetal vascular system) of undifferentiated connective tissue dysplasia. Also in the pathogenesis of clinical manifestations, the development of vasospastic reflex reactions caused by irritation of the sympathetic plexus of the vertebral arteries is of significant importance. The resulting flow of afferent impulses irritates the overlying centers of vascular-motor regulation, which is manifested by local/diffuse reactions that predominantly affect the vessels of the vertebrobasilar system.
Right vertebral artery
According to statistics, hypoplasia of the right vertebral artery occurs once in every tenth person, that is, it affects 10 people out of 100.
Narrowing of the right VA in most cases is also a congenital pathology. This form of the pathological process is also accompanied by impaired blood supply, however, ischemia and blood stagnation in this case occur less frequently.
Doctors call concomitant diseases of the circulatory system and blood vessels the main danger factor for PPA hypoplasia. If hypoplasia of the vertebral artery on the right is accompanied, for example, by vascular atherosclerosis, the development of the second disease and associated degenerative changes in the head will proceed many times faster than if the disease developed independently.
The severity of the pathological process largely depends on how extensive it is. The disease can affect the posterior communicating artery, cover all 4 segments (segments of the artery are not involved in the pathological process immediately, but one at a time), etc. In cases where the pathology takes on a severe course, is complicated by other diseases, affects the vertebrobasilar system and concerns vertebral artery, the patient may experience decreased sensitivity in certain areas of the body. This is a clear sign of circulatory problems in the corresponding area of the brain; in such situations, immediately consult a doctor and undergo an examination.
Causes
Hypoplasia is predominantly congenital in nature, the development of which can be caused by both chromosomal mutations and factors with an adverse effect on the mother’s body during pregnancy. These factors include:
- Bruises/injuries during pregnancy .
- Infectious diseases that have a negative impact on the fetus, especially in the early stages of development ( influenza , rubella ).
- Bad habits (smoking, alcoholism, drug addiction).
- Prolonged contact with harmful substances (work in hazardous industries, toxic chemicals, radiation).
- Drug abuse.
Symptoms
The initial signs of VA hypoplasia are nonspecific, and they can be mistaken for manifestations of encephalopathy , cervical osteochondrosis or vegetative-vascular dystonia . PA hypoplasia syndrome is clinically manifested by three groups of symptoms:
- A group of vertebral symptoms (pain in the cervical spine/occipital region).
- Local symptoms - pain in the vertebral artery/structures of the corresponding vertebral segment (during palpation) with pronounced irradiation to the head.
- Symptoms at a distance from the vascularization zone of the VA, as well as due to irritation of the sympathetic plexus of the vertebral artery (increased blood pressure, migraine -type pain , body instability when walking).
The specificity of the clinical manifestations of VA hypoplasia is determined by a number of factors: the localization/extension of the lesion, the functional state of the arterial-venous system of the brain - the presence of anastomoses, collaterals, the state of the vascular wall.
Standard patient complaints include frequent, severe headaches ; dizziness ; surges in blood pressure ; inability to concentrate; memory loss; increased weather sensitivity ; deterioration of vision/appearance of “spots” in the field of vision; unsteady gait, decreased performance; difficulty making sudden movements/turns.
The presence of neurological complaints is traditionally considered to be indirect signs of stenosis . The symptoms of left-sided and right-sided VA hypoplasia are generally similar, however, the pathology of the vertebral artery on the right is often localized higher (in the intracranial area), which causes a more rapid development of symptoms and their more pronounced manifestation (a sharp drop in vision, loss of consciousness, severe coordination disorder).
The left vertebral artery initially has a larger working diameter, so symptoms do not appear so sharply and later. With left-sided hypoplasia, the characteristic symptoms are sharp, throbbing occipital pain; shots to the head; pain on palpation of the 1st and 2nd vertebrae of the neck; feeling of sand/double vision; tinnitus/hearing impairment. With bilateral VA hypoplasia, due to the lack of a compensatory effect, symptoms develop quickly, and there is a high risk of developing serious complications.
Diagnostics
It is not easy to diagnose hypoplasia precisely because of the mild symptoms. The treatment of pathology is carried out by a neurologist, to whom you need to come for an appointment. Typically, treatment occurs after the first signs appear - it is better not to delay, since the brain is clearly experiencing problems with blood supply, otherwise there would be no symptoms.
Diagnostic features
First, the doctor interviews the patient, finds out what he is complaining about, and then examines the patient. Next, you will need to undergo a series of tests and undergo some studies in order to be able to make an accurate diagnosis.
Doctors use the following research methods to confirm the diagnosis.
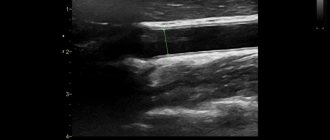
- Ultrasound of the vessels of the neck and head . Thanks to such a study, it is possible to clarify the diameter of the artery and the intensity of blood flow. If the artery has a diameter of less than 2 mm, then this is already considered a pathology. The normal diameter of the artery of the spinal column is 3.6-3.8 mm.
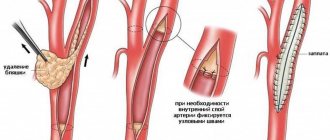
- Computed tomography of the brain and neck . The study makes it possible to assess the condition of blood vessels through the use of a special contrast agent.
- Angiography . This is a study using x-rays and special contrast agents. Makes it possible to detect anomalies in the structure of blood vessels.
MRI image
Consequences and complications
In general, VA hypoplasia significantly impairs quality of life. The most serious complications of VA hypoplasia primarily include a high risk of cerebrovascular accident/ stroke , which is caused by a decrease in blood supply to brain structures. In addition, frequent complications of the pathology of the vertebral arteries include neurological symptoms: headaches ( migraine ), irritability, depression, severe fatigue, disorders of the autonomic nervous system, impaired auditory/visual function, weakened cognitive abilities, dementia, decreased ability to work, arterial thrombosis
Forecast
The prognosis is determined by many factors, in particular, unilateral/bilateral VA pathology, since with unilateral VA hypoplasia, blood flow compensation mechanisms develop, the functional state of the arterial-venous system of the brain, and the condition of the vascular wall (in particular, the presence of atherosclerotic plaques). After surgical treatment and drug rehabilitation, in most cases the lumen of the vertebral arteries can be normalized, and neurological symptoms regress.
conclusions
TS BCA is the leading available non-invasive method for visualizing VA hypoplasia. The technique makes it possible to assess with great accuracy the diameter, course and condition of the walls of the arteries, and also, unlike other imaging methods, to study the speed indicators of blood flow and objectively judge the signs of hypoperfusion in the vertebrobasilar region.
Among additional examination methods for detailed visualization of intracranial arteries, we consider CT with contrast to be the most appropriate.
- Views: 4833
- Comments:
Did you like the post? Do you find it useful or interesting? Support the author!
List of sources
- Shmidt E.V. Classification of vascular lesions of the brain and spinal cord // Journal. neuropathology and psychiatry named after. S.S. Korsakov. 1985. T. 85, No. 9. p. 1281-1288.
- Kurtusunov B. T. Variant anatomy of the vertebral arteries at the stages of human ontogenesis. Author's abstract. diss. Doctor of Medical Sciences Volgograd, 2011.
- Pizova N.V., Druzhinin D.S., Dmitriev A.N. Hypoplasia of the vertebral arteries and cerebrovascular accidents // Journal of Neurology and Psychiatry. 2010. No. 7. P. 56–58.
- Kometov A.V., Zhukova M.V. Variants of the structure of the vessels of the arterial circle of the cerebrum depending on the type of Kimmerle anomaly. Congress of Manual Therapists of Russia, 1st: Materials. M 1999; 32.
- Odinak M.M., Mikhailenko A.A., Ivanov Yu.S. and others. Vascular diseases of the brain. St. Petersburg: Hippocrates 1997.