An uninterrupted supply of blood to the brain, saturated with nutrients and oxygen, the main condition for its normal functioning, is ensured by the vascular system. No other cells stop functioning as quickly as nerve cells when there is a sharp decrease or cessation of blood supply. Even a short-term disruption of blood flow to the brain can lead to fainting. The reason for this sensitivity is the great need of nerve cells for oxygen and nutrients, mainly glucose.
The total cerebral blood flow in humans is about 50 ml of blood per minute per 100 g of brain tissue and is unchanged. In children, blood flow values are 50% higher than in adults, in old people they are 20% lower. Under normal conditions, unchanged blood flow through the brain as a whole is observed when mean arterial pressure fluctuates from 80 to 160 mm Hg. Art. Very sharp changes in the tension of oxygen and carbon dioxide in arterial blood affect the total cerebral blood flow. The constancy of total cerebral blood flow is maintained by a complex regulatory mechanism.
The blood supply to various parts of the brain depends on the degree of their activity. With increased activity of the cerebral cortex (for example, when reading, solving problems), blood flow in certain zones increases by 20–60% due to the expansion of cerebral vessels. With general excitement it increases by 1.5–2 times, and in a state of rage – by 3 times. During anesthesia or hypothermia, cortical blood flow is significantly reduced.
Blood supply system of the brain
Blood enters the brain through 4 large vessels: 2 internal carotid and 2 vertebral arteries. Blood flows from it through 2 internal jugular veins.
Internal carotid arteries The internal carotid arteries are branches of the common carotid arteries, the left one departs from the aortic arch. The left and right common carotid arteries are located in the lateral areas of the neck. The pulse vibrations of their walls can be easily felt through the skin by placing your fingers on the neck. Severe compression of the carotid arteries disrupts the blood supply to the brain. At the level of the upper edge of the larynx, the common carotid artery divides into the external and internal carotid arteries. The internal carotid artery penetrates the cranial cavity, where it takes part in the blood supply to the brain and eyeball, the external carotid artery nourishes the organs of the neck, face, and scalp.
Vertebral arteries The vertebral arteries arise from the subclavian arteries, are directed to the head through a chain of openings in the transverse processes of the cervical vertebrae and enter the cranial cavity through the foramen magnum.
Since the vessels supplying the brain extend from the branches of the aortic arch, the speed and pressure of the blood in them are high and have pulse fluctuations. To smooth them, at the entrance to the skull, the internal carotid and vertebral arteries form double bends (siphons). Having entered the cranial cavity, the arteries connect with each other, forming on the lower surface of the brain the so-called circle of Willis, or arterial circle of the cerebrum. It allows, if there is difficulty in delivering blood through any vessel, to redistribute it from other sources and prevent disruption of the blood supply to a part of the brain. However, under normal conditions, blood brought through different arteries does not mix in the vessels of the circle of Willis.
Cerebral arteries The anterior and middle cerebral arteries depart from the internal carotid artery, supplying the inner and outer surfaces of the cerebral hemispheres (frontal, parietal and temporal lobes) and the deep parts of the brain. The posterior cerebral arteries, which supply the occipital lobes of the hemispheres, and the arteries that supply blood to the brain stem and cerebellum, are branches of the vertebral arteries. The vessels supplying the spinal cord also depart from the vertebral arteries. Numerous thin arteries arise from the large cerebral arteries and plunge into the brain tissue. The diameter of these arteries varies widely; according to their length, they are divided into short ones, which supply the cerebral cortex, and long ones, which supply the white matter. The highest percentage of hemorrhages in the brain is observed with pathological changes in the walls of these particular arteries.
The branches of small arteries form a capillary network, unevenly distributed in the brain - the density of capillaries in the gray matter is 2-3 times higher than in the white matter. On average, there are 15´107 capillaries per 100 g of brain tissue, and their total cross-section is 20 square meters. cm.
The capillary wall does not come into contact with the surface of the nerve cells, and the transfer of oxygen and other substances from the blood to the nerve cell is carried out through the mediation of special cells - astrocytes.
Blood-brain barrier The regulation of the transport of substances from the blood capillary into the nervous tissue is called the blood-brain barrier. Normally, iodine compounds, salicylic acid salts, antibiotics, and immune bodies do not pass from the blood to the brain (are retained by a barrier). This means that drugs containing these substances, when introduced into the blood, do not affect the nervous system. Conversely, alcohol, chloroform, strychnine, morphine, tetanus toxin, etc. easily pass through the blood-brain barrier. This explains the rapid effect of these substances on the nervous system.
To avoid the blood-brain barrier, antibiotics and other chemicals used to treat brain infections are injected directly into the fluid surrounding the brain, the cerebrospinal fluid (CSF). This is done through a puncture in the lumbar spine or in the suboccipital region.
Internal jugular veins The outflow of blood from the brain occurs through veins that flow into the sinuses of the dura mater. They are slit-like channels in the dense connective tissue membrane of the brain, the lumen of which remains open under any conditions. Such a device ensures uninterrupted outflow of blood from the brain, which prevents stagnation. The sinuses leave a mark in the form of wide grooves on the inner surface of the skull. Through the sinus system, venous blood from the brain moves to the jugular foramen at the base of the skull, from where the internal jugular vein originates. Through the right and left internal jugular veins, blood from the brain flows into the superior vena cava system.
The sinuses of the dura mater communicate with the superficial (saphenous) veins of the head through special veins passing through the bones of the skull. This allows, under certain conditions, to “dump” part of the venous blood from the cranial cavity not into the internal jugular vein, but through the subcutaneous vessels into the external jugular vein.
The evolution of the brain has brought man to the top of the pyramid of living nature. The brain belongs to the central nervous system and performs the functions of regulation and coordination of the activities of all organs in the body, communicates them with the environment and adapts the body to the changes that occur.
Main arteries of the head
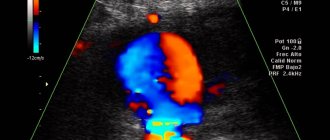
Angiography of the main arteries of the head
is an instrumental research method that allows you to literally “see” the vessels of the brain. To carry out the study, it is necessary to introduce a contrast agent into the corresponding vessel of the brain and the presence of an X-ray machine, with the help of which an image of the vessels filled with this contrast will be recorded. Angiography of cerebral vessels is not a routine diagnostic method; it has its own indications and contraindications, and, unfortunately, complications. Angiography in a broad sense is the acquisition of images of any blood vessels in the body using X-rays. Angiography of cerebral vessels is just one of the varieties of this extensive research method.
What is cerebral angiography?
The essence of this research method is as follows. The patient is injected into a specific cerebral artery (or the entire network of cerebral arteries) with an X-ray contrast agent, usually iodine-based (Optirey, Omnipaque, Ultravist and others). This is done so that an image of the vessel can be recorded using x-rays, since the vessels are poorly visualized with a regular image. The introduction of a radiopaque substance is possible by puncture of the corresponding artery through a catheter connected to the required vessel from the periphery (usually from the femoral artery). When the contrast agent appears in the vascular bed, a series of X-ray images are taken in two projections. The resulting images are evaluated by a doctor and conclusions are drawn about the presence or absence of a certain pathology of the cerebral vessels.
Indications for use
Angiography of the main arteries of the head is a specialized diagnostic method that should only be prescribed by a doctor. It is not performed at the request of the patient. The main indications are:
• suspicion of arterial aneurysm of cerebral vessels;
• suspicion of arteriovenous malformation;
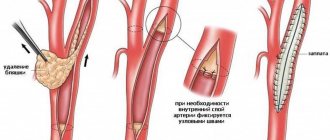
• determining the degree of stenosis (narrowing) or occlusion (blockage) of cerebral vessels, that is, establishing the lumen of the corresponding vessels. In this case, the severity of atherosclerotic changes in the vessels and the need for subsequent surgical intervention are established;
• establishing the relationship between the cerebral vessels and the adjacent tumor to plan surgical access;
• control of the location of clips applied to the vessels of the brain.
I would like to note that simply complaints of dizziness, headache, tinnitus, and the like are not in themselves an indication for angiography. Patients with such symptoms should be examined by a neurologist, and based on the results of the examination, as well as other research methods, the need for angiography is determined. This necessity is determined by the doctor!
Contraindications
The main contraindications are:
• allergic reaction (intolerance) to iodine preparations and other radiopaque substances;
• pregnancy (due to ionizing radiation during the procedure). In this case, MR angiography may be performed;
• mental illnesses that do not allow one to comply with all the conditions for the procedure (for example, a person will not be able to remain motionless during the image);
• acute infectious and inflammatory diseases (as the risk of complications increases);
• violation of blood coagulation system parameters (both downward and upward);
• the general condition of the patient, regarded as serious (this may be stage III heart failure, end-stage renal and liver failure, coma, and so on). Essentially, this subgroup of contraindications is relative.
Preparation for angiography
To obtain accurate results and reduce the risk of complications from the procedure, it is recommended:
• take general and biochemical blood tests, including determining the indicators of the coagulation system (the period of limitation of tests should not exceed 5 days). The blood type and Rh factor are also determined in case of possible complications;
• do an ECG and FG (FG, if one has not been performed within the last year);
• do not drink alcoholic beverages for 14 days;
• during the last week, do not take medications that affect blood clotting;
• perform an allergy test with a contrast agent. To do this, 0.1 ml of the corresponding drug is administered intravenously to the patient over 1-2 days and the reaction is assessed (the appearance of itching, rash, difficulty breathing, etc.). If a reaction occurs, the procedure is contraindicated!
• the day before, take antihistamines (anti-allergic) drugs and tranquilizers (if necessary and only as prescribed by a doctor!);
• do not eat for 8 hours and do not drink water 4 hours before the test;
• swim and shave (if necessary) the site of puncture or catheterization of the vessel;
• before the examination itself, remove all metal objects (hairpins, jewelry).
Research technique
At the very beginning, the patient signs consent to conduct this type of study. The patient is placed with an intravenous peripheral catheter to have immediate access to the circulatory system. Then premedication is carried out (approximately 20-30 minutes before the procedure): antihistamines, tranquilizers, painkillers are administered to minimize discomfort during the procedure and the risk of complications.
The patient is placed on the table and connected to devices (cardiomonitor, pulse oximeter). After treating the skin with local anesthetic and anesthesia, the corresponding vessel is punctured. A small skin incision is made and a puncture of the femoral artery is made, followed by immersion of the catheter and passing it through the vessels to the study site. Advancement of the catheter along the arterial bed is not accompanied by pain, since the inner wall of the vessels is devoid of pain receptors. The catheter's progress is monitored using x-rays. When the catheter is brought to the mouth of the required vessel, a contrast agent in a volume of 8-10 ml, preheated to body temperature, is injected through it. The administration of contrast may be accompanied by the appearance of a metallic taste in the mouth, a feeling of heat, and a rush of blood to the face. These sensations go away on their own within a few minutes. After the administration of contrast, X-ray images are taken in several projections almost every second several times (which allows you to see the arteries, the capillary phase, and veins). Then the catheter is removed, and a sterile pressure bandage is applied to the puncture site of the vessel. The patient should be monitored by medical personnel for at least 6-10 hours.
Complications
According to statistics, complications during this diagnostic method occur in 0.4-3% of cases, that is, not so often. Their occurrence may be associated both with the procedure itself (for example, bleeding from the puncture site of a vessel) and with the use of a contrast agent. It should be borne in mind that compliance with all conditions when preparing and performing angiography is the prevention of possible complications.
So, possible complications of cerebral angiography are:
• vomit;
• an allergic reaction to an iodine-containing drug: itching, swelling and redness at the injection site, followed by the appearance of shortness of breath (reflex breathing disorder), a drop in blood pressure, and heart rhythm disturbances. In severe cases, anaphylactic shock may develop, which is a life-threatening condition;
• spasm of cerebral vessels and, as a consequence, acute cerebrovascular accident (up to stroke);
• convulsive seizures;
• penetration of the contrast agent into the soft tissue in the area of the puncture of the vessel (outside the vascular bed). If the volume of the drug spilled into the tissue is up to 10 ml, then the consequences are minimal, but if more, then inflammation of the skin and subcutaneous fat develops;
Cerebrovascular disorders
Temporary disorders of cerebral circulation occur for various reasons. Due to osteochondrosis, the openings in the cervical vertebrae narrow, the vessels passing through them are compressed, and the blood supply to the brain becomes difficult - headaches, migraines, etc. appear. With increased blood pressure, severe anxiety or tension, headaches, dizziness, a feeling of heaviness in the head also appear, sometimes vomiting and short-term loss of consciousness.
Author: Olga Gurova, Candidate of Biological Sciences, Senior Researcher, Associate Professor of the Department of Human Anatomy of the RUDN University