Causes of obliterating atherosclerosis of the arteries
The disease causes severe circulatory failure in the legs, dooms patients to excruciating suffering and makes them unable to work. The process is localized mainly in large vessels (aorta, iliac arteries) or medium-sized arteries (femoral, popliteal arteries).
The most striking sign of ischemia of the lower extremities is intermittent claudication, characterized by the appearance of pain, a feeling of numbness and compression in the leg muscles when walking. This sensation forces the patient to stop, after which the pain and compression gradually disappear, but when the load is resumed, the pain returns. The affected leg is usually paler than the opposite leg and cold to the touch. Even minor injuries (scratches, bruises, abrasions) heal poorly and can cause ulcers. The feeling of numbness and pain at rest is often also caused by ischemia of the nerve trunks (ischemic neuritis). Prolonged course of the disease leads to the development of gangrene and inevitable amputation.
The degree of damage to the vascular bed is based on the walking distance. The pain forces the patient to stop, waiting for it to disappear. Without treatment, the disease continues to progress, which leads to a decrease in walking distance, limitation of the patient’s physical activity, and the inability to lead a normal lifestyle. Unfortunately, most often patients associate these pain sensations simply with muscle fatigue due to age, or with venous problems, defining the pain as a cramp, thus delaying seeking medical help and deepening the degree of damage to the arterial bed. In severe cases, the patient cannot walk 10 meters without stopping, but then it gets even worse: pain appears at rest, initially passing in an upright position, but after a short period of time the pain becomes constant, taking painkillers becomes ineffective. Gradually, the lumen of the artery narrows, leading to complete closure. Doctors are forced to admit that patients seek medical attention. help is late when the damage to the limbs is irreversible.
Risk factors:
- smoking;
- regular increase in blood pressure;
- high concentration of total cholesterol and its components in the blood;
- overweight (obesity);
- sedentary lifestyle (hypodynamia);
- diabetes;
- cardiovascular diseases in close relatives.
Damage to the vascular system of the lower extremities is a life-threatening condition, and ranks third in the structure of mortality from cardiovascular diseases. This figure is due to the development of such a severe complication as gangrene of the limb, which often leads to the need for amputation, and with high amputation, the mortality rate is 25%. Along with this, it should be noted that 50% of patients die within a year without amputation after the diagnosis of “critical ischemia”.
Symptoms of obliterating atherosclerosis of the arteries of the lower extremities
Pay attention to the following symptoms in yourself or your loved ones:
- fatigue in the calf muscles or thigh muscles when walking 500 meters or less,
- a feeling of leaden heaviness in the legs or muscle pain that makes you stop when walking,
- changes in the skin on the legs in the form of peeling, thinning, hair loss.
Important!
These are signs of atherosclerotic damage to the arteries of the lower extremities. An examination by a vascular surgeon is required in the near future. Do not be surprised if, when diagnosing lesions of the arteries of the lower extremities, your carotid arteries are checked and a cardiological examination is prescribed. Atherosclerosis is a systemic disease, and, as a rule, different groups of blood vessels are affected.
If sharp pain in the foot or lower leg occurs simultaneously with paleness and coldness of the skin, you must immediately call an ambulance, otherwise you may not have time to save the limb.
How does the disease manifest itself?
With atherosclerosis of the extremities, a person begins to experience sharp pain when walking and lameness appears. After walking short distances, the patient feels terrible fatigue, stiffness in movements, cramps, and his toes go numb. It seems that the leg suddenly became unbearably heavy, as if a weight had been put on it. Typically, one leg is affected by atherosclerosis of the lower extremities. After rest, the pain goes away, but not for long.
Cause of numbness in legs
Probably each of us remembers this unpleasant feeling when our legs go numb and you simply can’t feel them. This includes tingling throughout the body, a “chill,” and a feeling of temporary paralysis of the limbs. There are different reasons for this:
- uncomfortable sitting position, when nerve endings are compressed;
- diabetes mellitus;
- poor circulation in the legs,
- manifestation of osteochondrosis;
- lack of vitamins in the body;
- migraine;
- multiple sclerosis;
- inflammation of the nerves in various diseases: arthritis, etc.
Fortunately, numbness in the legs is not always a harbinger of serious illness. However, this is always a reason to immediately contact a vascular surgeon.
Risk factors for the development of atherosclerosis of the lower extremities:
- age 40 -50 years;
- male gender;
- large amounts of alcohol;
- smoking;
- high cholesterol levels;
- diabetes mellitus;
- hypertension;
- stress;
- sedentary and sedentary lifestyle.
The main methods for diagnosing obliterating atherosclerosis of the arteries of the lower extremities:
- measurement of the ankle-brachial index (the ankle-brachial index is a parameter that allows you to assess the adequacy of arterial blood flow in the lower extremities);
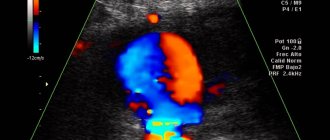
- duplex scanning of the arteries of the lower extremities is the “gold standard” for screening patients (detection and follow-up);
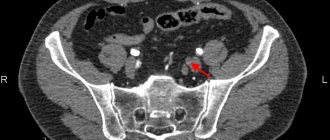
- MSCT angiography of the aorta and arteries of the lower extremities is the “gold standard” of preoperative examination and in cases where information from ultrasound scanning is insufficient;
- X-ray contrast angiography.
Diagnostics
To establish a diagnosis of “non-stenotic atherosclerosis,” the patient is prescribed instrumental diagnostic methods such as ultrasound and Doppler examination. They allow you to obtain as much information as possible about the vessels.
When examined using Doppler, the doctor can see the degree of narrowing of the arteries, the exact location of cholesterol plaques, and the condition of the vessel walls. This method also makes it possible to determine the speed of blood flow. All these indicators determine the patient’s further treatment plan.
In addition, the patient must undergo a blood test to determine cholesterol levels.
Treatment methods for obliterating atherosclerosis of the arteries of the lower extremities:
Conservative therapy
In the early stages of obliterating atherosclerosis of the arteries of the lower extremities, conservative treatment is indicated, which must be comprehensive, and all unfavorable factors causing vasospasm must be excluded. A necessary condition for successful treatment is quitting smoking(!). Physical activity is of paramount importance. Patients with intermittent claudication should walk daily for 30-45 minutes - this promotes the development of small arteries, leads to an increase in muscle strength and an increase in the distance traveled without pain.
If pain and compression appear in the leg muscles, the patient should stop, and after these sensations disappear, continue walking. Often, cycling or swimming are much better tolerated than walking (however, they do not replace it). Correction of increased blood pressure, normalization of blood cholesterol levels, blood glucose levels in patients with diabetes mellitus. Drugs are used that reduce the tone of small vessels, increase the flexibility of red blood cells and prevent the formation of blood clots in the vessels. Physiotherapeutic and balneological procedures, hyperbaric oxygenation are also used.
Surgical treatment of arteriosclerosis of the arteries of the lower arteries, vessels
Reconstructive operations:
- X-ray endovascular treatment methods.
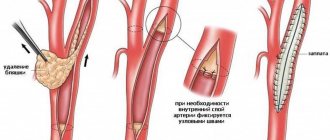
Under the control of X-rays using special long thin instruments, through a small puncture in the femoral artery (less often other arteries), we can reach the affected vessel (area of blood vessels) of the lower extremities. Modern technical capabilities make it possible to expand a section of the vessel from the inside with a special balloon and, if necessary, install a thin metal frame (stent) that prevents re-narrowing.
- Open surgical interventions.
For patients with blockage of a vessel lasting no more than 7-9 cm, the internal modified layer of the artery with atherosclerotic plaque and blood clots is removed (endarterectomy). With a more significant spread of the occlusive process, pronounced calcium deposition in the artery wall, a bypass of the blood flow (bypass) or resection of a section of the artery and its replacement with a synthetic prosthesis or biomaterial (prosthetics) is indicated.
Amputation
If, despite the treatment, ischemia of the affected limb increases and gangrene progresses, amputation is indicated: its level must be strictly individual and carried out taking into account the blood supply to the limb.
The many faces of atherosclerosis: abdominal ischemic disease - a symptom or a syndrome?
Atherosclerosis is the leading cause of mortality and disability in cardiovascular diseases (CVD). It is well known: the more areas affected by atherosclerosis, the worse the prognosis. If only coronary heart disease (IHD) is present, the mortality rate is 5%; if IHD is combined with damage to cerebral vessels, the mortality rate increases to 10%; when IHD is combined with peripheral atherosclerosis, it increases to 13%; and in the presence of atherosclerosis of all three localizations, mortality reaches 17%. The older a person is, the higher the risk of peripheral atherosclerosis; at 75-79 years old it is 20-30%.
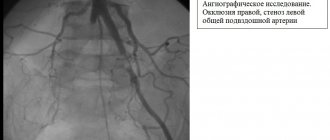
Thus, atherosclerosis of the abdominal aorta and its unpaired visceral branches, described more than 150 years ago by the German pathologist F. Tiedemann, is a severe ischemic disease of the digestive organs, being a manifestation of systemic atherosclerosis. In the general population of patients, during angiographic examination, atherosclerotic lesions of unpaired visceral branches are detected in 54% of patients, while isolated stenosis of the celiac trunk (CS) occurs in 25-45% of cases, the superior mesenteric artery (SMA) - in 30-80%, the inferior mesenteric artery - in 23%, with occlusion of the iliac and femoral arteries - in 25-69% of cases. The predominant localization of atherosclerotic stenosis is the mouth or initial part of the vessel from 0.5 to 2 cm. A more extensive lesion, reaching 8-10 cm, is observed in the superior mesenteric artery, and often the process is multifocal with a double or triple block in the lumen of the vessel. It should be emphasized that with this localization there is a discrepancy between pronounced morphological changes and the absence of clinical symptoms, since insufficiency of mesenteric circulation can be successfully compensated for a long time. The frequent asymptomatic course observed in 64.3% of patients with abdominal ischemia and the vague clinical picture make it difficult to diagnose this disease. In practice, we often have to deal with combined lesions of the emergency and SMA. This is due, on the one hand, to the severity of atherosclerosis, and on the other hand, to the late presentation of patients in whom, when arterial occlusion has developed, another vessel begins to be involved in the stenotic process, as a result of which the visceral blood flow becomes close to anatomical and functional decompensation. Inadequate oxygen supply to the digestive organs leads to the development of transient ischemic failure of the gastrointestinal tract (GIT). If ischemia is transient, it manifests itself as a pain syndrome—abdomialgia. With prolonged ischemia, focal disorders develop - visceropathy. Isolated damage to the stomach and duodenum (duodenum) is observed in 14.5%, pancreas (PG) in 26.3%, liver - in 20.5%, in 86.6% there is combined damage to the digestive organs, which often complicates early diagnosis of damage to a particular organ. Atherosclerosis of the abdominal vessels is quite common in individuals with such independent risk factors as coronary artery disease, arterial hypertension (AH), heart rhythm disturbances, smoking, and dyslipidemia.
Definition and classification
Abdominal ischemic disease (AID) is a disease of the digestive organs caused by a discrepancy between the abdominal blood flow and the oxygen needs of the digestive organs, leading to metabolic disorders with the development of ischemic visceropathy.
The non-specificity of the clinical picture with possible course options, on the one hand, the similarity with various chronic diseases of the gastrointestinal tract, on the other, creates diagnostic difficulties, which determined the need to develop a clinical classification of the disease.
We present our version of the clinical and pathogenetic classification of AIB:
1. Forms: celiac; mesenteric; celiac mesenteric.
2. Stages of flow: compensated; subcompensated; decompensated.
3. Etiopathogenetic risk factors: atherosclerotic stenosis or occlusion; Abdomenovascular risk factors: hyperlipidemia, hemorheological syndrome.
4. Clinical and morphological options:
1 - abdominal ischemic visceralgia:
a) stable;
b) progressive.
2 - abdominal ischemic visceropathy:
• ischemic gastroduodenopathy: atrophy; erosions (complete, incomplete); ulcers (stomach, duodenum);
• ischemic hepatopathy: hepatic cell failure with impaired protein synthetic function; with a violation of the absorption-excretory function;
• ischemic pancreatopathy: painful; latent with impaired exocrine or intrasecretory function;
• ischemic enterocolonopathy: proximal enteropathy; terminal colonopathy.
5. Anatomical and morphological features:
• Subatrophy or atrophy of the gastric mucosa, duodenum; erosion of the mucous membrane of the stomach, duodenum (complete, incomplete); stomach ulcers (lesser curvature, body, antrum), duodenal ulcer (bulb, body).
• Dystrophy (sclerosis), fibrosis of the liver parenchyma: focal, diffuse.
• Atrophy, lipomatosis, sclerosis (head and/or body and/or tail of the pancreas).
• Segmental fibrosis of the small and large intestine, colon dystrophy.
6. Complications:
• Gastric bleeding, perforation.
• Hepatocellular failure (portal hypertension, liver cirrhosis, hepatic coma).
• Pancreatic insufficiency, diabetes mellitus, pancreatic necrosis.
• Ischemic ulcer of the colon, ischemic ulcer of the small intestine, acute intestinal bleeding, acute intestinal obstruction, intestinal infarction, intestinal gangrene.
Clinical manifestations
The dynamics of clinical manifestations are different, but in approximately half of the patients the disease has a latent course or an erased form of the disease. The clinical picture of chronic abdominal ischemia (CAI) is very diverse, and the classic triad occurs only in 10-39% of patients in the form of epi- and mesogastric pain 10-15 minutes after eating, bloating, flatulence, weight loss. Symptoms of CAI occur after minimal load on the gastrointestinal tract, and sometimes persist in a state of functional rest of the abdominal organs. This indicates the presence of a constant deficiency in the blood supply to the digestive organs, clearly manifested by the syndrome of digestive insufficiency: abdominal pain, gastric and intestinal dyspepsia; progressive weight loss; anemization; asthenodepressive state.
Depending on the localization of the occlusive process, two clinical forms are distinguished: celiac - with a predominance of the pain symptom complex and mesenteric - with a predominance of intestinal dyspepsia due to a violation of the secretory, absorption, and evacuation functions of the intestine. When an emergency occurs, the organs of the upper floor of the abdominal cavity are predominantly affected: liver, pancreas, stomach, duodenum, spleen. Stenosis or occlusion of the SMA is manifested by various dysfunctions of the small intestine, and damage to the inferior mesenteric artery (IMA) causes ischemia of the large intestine. A well-developed collateral network between the visceral arteries promotes long-term functional compensation in conditions of impaired main blood flow, therefore, occlusive or stenotic lesions of the visceral branches of the abdominal aorta do not always lead to the manifestation of symptoms of CAI. The most striking clinical picture is observed when two or three visceral arteries are affected.
The clinical picture of abdominal circulatory disorders manifests itself in two main forms - acute and chronic. The acute form, leading to the development of intestinal infarction, has more or less distinct symptoms and in most cases is correctly diagnosed, while the clinical picture of CAI is more blurred, can occur under a “mask” and is similar to many gastrointestinal diseases. The nature and severity of the symptom complex that appears is determined by the severity of ischemia of the abdominal organs.
The first stage - the compensation stage (preclinical) - indicates a moderate degree of stenosis of the visceral vessels or a good possibility of collateral blood supply, replenishing the blood deficiency in the affected artery and thereby maintaining balance in the blood supply of all three highways. As the occlusive process progresses and the compensatory capabilities of collateral circulation decrease, the existing balance is disturbed. The first signs of CAI appear in the form of a feeling of heaviness in the epigastric region, bloating, a feeling of overeating after eating a small amount of food, stool irregularity in the form of causeless constipation, followed by diarrhea with minor violations of the usual eating regimen, and other manifestations of gastric and intestinal discomfort. This indicates the onset of a new stage in the disturbance of abdominal circulation - the stage of subcompensation. Further progression of the atherosclerotic process and a decrease in the compensatory capabilities of the collateral circulation causes an increase in circulatory disorders and the transition to the stage of decompensation.
In the initial stage, the pain is equivalent to a feeling of heaviness in the epigastric region, acquires an aching character, gradually increasing in intensity, occurring 10-20 minutes after eating and lasting up to 2-2.5 hours, and then subsiding on its own and becoming more frequent as it worsens circulatory disorders. The localization of pain varies. For circulatory disorders in the SMA basin, mesogastric pain (around the navel) with irradiation throughout the abdomen is more typical. When the emergency is affected, the pain is localized in the epigastric region and often radiates to the right hypochondrium. If the NBA is affected - in the left iliac region. The intensity of pain varies, becoming constant. In the initial stages, it is controlled by the use of heat, reducing the amount of food taken, taking anticholinergics or nitroglycerin; later these measures become ineffective.
The second common symptom of AIB is intestinal dysfunction, which is manifested by a violation of the secretory and absorption functions of the small intestine in the form of flatulence, unstable stool in the form of diarrhea, and if the evacuation function of the large intestine is impaired, persistent constipation.
The third most common symptom is progressive weight loss and anemia, often associated with the refusal of patients to eat due to pain, on the one hand, and a violation of the secretory and absorption functions of the small intestine, on the other, which is especially pronounced during decompensation.
The most common and reliable sign of stenosis of the SN and the presence of AIB is a vascular murmur heard 2-4 cm below the xiphoid process in the midline of the abdomen, or 2-4 cm above the umbilicus, or 2-3 cm to the right of the midline of the abdomen, carried out in a limited area, on average 1-2 cm from the point of maximum intensity. But it should be noted that if the presence of noise indicates damage to the visceral branches, then the absence of noise indicates the possibility of an occlusive process. It is necessary to take into account the fact that with atherosclerosis of the abdominal aorta and its branches, the process is systemic in nature, affecting other vascular systems (heart, brain, limbs, kidneys). Accordingly, the degree of changes in central hemodynamics correlates with the severity of damage in these organs, which also aggravates circulatory disorders in the digestive organs, and this is quite natural. According to our observations, severe atherosclerosis of the coronary arteries is diagnosed in 66.4% of patients. It seems that atherosclerosis of the celiac mesenteric and coronary vessels develops in parallel. Moreover, in patients with coronary artery disease with relative compensation of mesenteric blood circulation, the appearance of primary flatulence in the form of a feeling of fullness, heaviness after eating, belching should be considered as early signs of celiac insufficiency, similar to the symptoms of angina pectoris in atherosclerosis of the coronary arteries.
Ischemic gastroduodenopathy and erosive-ulcerative lesions
The degree and extent of gastric vascular damage determine the clinical picture. In patients with AIB, erosive and ulcerative lesions of the stomach are detected in 50% of cases. The clinical picture is typical for the AIB clinic. For ischemic ulcerative lesions, the seasonality of exacerbations characteristic of peptic ulcer disease is uncharacteristic. Often there is a coincidence of periods of exacerbation of ischemic heart disease or hypertension, acute cerebrovascular accident with erosive and ulcerative exacerbation. With sub- and decompensation, acid formation is reduced both in the basal period and after submaximal stimulation with pentagastrin. The fact is obvious: the more pronounced the ischemia, the more suppressed the secretion. Daily monitoring of gastric secretion and X-ray examination revealed disturbances in the motor-evacuation function of the stomach in the form of decreased contractile activity, weakened motility, decreased gastric tone, decreased gastric motility, and often bulbostasis, arrhythmia of gastric contractions, dystonia and dyskinesia of the duodenum and duodenogastric reflux, often with a picture of chronic duodenal obstruction. One of the reasons for impaired motor-evacuation function of the stomach is a deficiency of cholinergic mediators. Impaired motor-evacuation function is an early manifestation of mesenteric insufficiency. During endoscopic examination, erosive and ulcerative lesions of the stomach are most often observed, while in the absence of CAI, erosive and ulcerative lesions of the duodenum are observed. Typical localization of erosive and ulcerative lesions in CAI is the lesser curvature and antrum. The size of the ulcers varies from 0.8 to 2.5 cm, reaching a diameter of 0.2-0.3 cm. Scarring of the ulcers occurs within 4-12 weeks, and erosions of the antrum of the stomach may not heal for six months. A morphological study of biopsies of the gastric and duodenal mucosa stained with the HAPP reaction (hematoxylin basic-fuchsin-picric acid, used to identify ischemic damage) revealed pronounced atrophic and dystrophic changes in the mucous membrane of the stomach and duodenum. These changes are more pronounced in the mucous membrane of the antrum. Dilation and congestion of the capillaries with hemorrhage into the lamina propria of the stomach and duodenum were noted. Areas of intestinal metaplasia, hemorrhagic impregnation of the stroma, damage to the glands against the background of chronic atrophic gastritis, atrophic gastritis with focal lymphangiectasia, individual areas of pronounced swelling of the mucosa in the form of anemic fields, the presence of sclerotic changes in the gastric mucosa and the muscular plate of the own mucosa, the presence of sharp dilated and ectatic vessels. A morphometric study in patients with atrophic gastritis shows thinning of the gastric mucosa, a decrease in the depth of the gastric pits and glands.
Ischemic pancreatopathy
When studying the exocrine function of the pancreas, a decrease in the absolute concentration in the blood plasma of its enzymes - amylase, lipase, trypsin inhibitor - is noted. Microscopic examination of feces reveals a large amount of neutral fat and undigested muscle fibers, which is a sign of exocrine insufficiency of pancreatic function. Ultrasound examination reveals heterogeneity of the echostructure, thickening of the capsule, areas of focal fibrosis or atrophy, sclerosis or lipomatosis with cystic fibrous tissue changes. Morphological changes are represented by a violation of the microvasculature in the form of parietal thrombi and angiosclerosis with pronounced obliteration of blood vessels, stasis and lysis of erythrocytes, diapedetic hemorrhages and uneven accumulation of mucopolysaccharides in the vascular wall, which indicates a violation of intravascular permeability. The pancreas tissue is represented by dystrophic, atrophic changes in the parenchyma, necrobiosis of the acini against the background of pronounced degenerative changes in acinar cells, stromal edema and foci of sclerosis, with pronounced lipomatosis, proteinaceous, granular fatty degeneration, periacinar and perivenular fibrosis, the formation of cysts and cystadenomas. Patients with ischemic damage to the pancreas have a special type of metabolism: there is an increase in the content of intracellular adenosine monophosphate, a distortion of metabolism to the insulin load, a change in the functional connections between hormones and cyclic nucleotides, which causes tissue insulin resistance due to compensatory tension of the endocrine function against the background of chronic hypoxia and ischemia. Therefore, these patients should be considered as persons with prediabetes, in whom the development of macroangiopathy precedes the manifestation of carbohydrate metabolism disorders, and the condition itself - as a manifestation of ischemic pancreatopathy.
Ischemic hepatopathy
Disturbances in the intensity of hepatic blood flow are observed in 26.3% of patients. When studying the hepatobiliary system with methionine-selenium 75, which is tropic for hepatocytes, dystrophic changes were noted in the entire mass of hepatocytes, adhesions in the subhepatic space, intrahepatic and moderately expressed extrahepatic cholestasis, caused by a violation of the metabolic processes of bile secretion. In the morphological and histochemical study of liver tissue, microcirculation disorders are observed in the form of erythrocyte aggregation, changes in the parenchyma and stroma, protein and fatty degeneration of varying severity, necrosis of hepatocytes and tissue fibrosis. Functionally, this manifests itself in the form of latent or obvious hepatocellular failure with impaired protein-synthetic, absorption-excretory functions.
Ischemic enterocolopathy
The high percentage of complications in ischemic enterocolopathy is due to the peculiarities of the blood circulation of the colon. The most vulnerable place in the colon is the splenic flexure, located in the area of adjacent blood supply to the basins of the two mesenteric arteries. This part of the intestine is involved in the ischemic process more often than other parts, occurring in 80% of cases. During colonoscopy in patients with both lesions of the inferior mesenteric artery and combined lesions of the SMA and IMA, changes are visible in the form of diffuse or segmental colopathy with excess mucus production, mucosal atrophy with the appearance of multiple small polyps, segmental narrowing of the lumen of the colon with the disappearance of haustrations in this segment. In some cases, erosions are observed in the area of the transition of the sigmoid colon to the rectum, but there are no perifocal changes. Histologically, in the mucous membrane of the colon, there is a decrease in crypts and the development of tender areas of fibrosis, dilatation and angiectasia of the vessels of the submucosal layer, focal lymphoid cell infiltration in the superficial layers of the own mucosa and submucosal layer with thinning of the lamina propria, which indicates the presence of sluggish chronic segmental or diffuse enteritis and /or colitis.
Diagnostic algorithms
1. A thorough examination of the anamnesis to identify risk groups - the presence of CVD (coronary artery disease, myocardial infarction, hypertension, rhythm disturbances, cerebrovascular insufficiency) in the absence of chronic pathology of the gastrointestinal tract - 75%.
2. Clinical picture with analysis of complaints: the prevalence of the clinical triad.
3. Objective examination: palpation and auscultation of the abdominal aorta. In 50-65% of cases, pulsation is detected, and in 65% a vascular murmur is heard, the epicenter is localized 2-4 cm below the xiphoid process along the midline of the abdomen or in the area of the projection of the abdominal aorta from the xiphoid process to the navel.
4. Ultrasound Dopplerography of the abdominal aorta, ES, SMA and NBA - 50-85%.
5. Magnetic resonance imaging - 78-82%.
6. Angiography of the abdominal aorta and unpaired visceral branches: atherosclerosis of the abdominal aorta, stenosis of the emergency, hepatic, gastroduodenal arteries, SMA, NBA - 90-98%.
Treatment methods
Algorithms for the treatment of AIB are built in the same way as for the treatment of atherosclerosis in general, taking into account the main links of pathogenesis and clinical syndromes.
1. Impact on processes that stabilize endothelial dysfunction and atherosclerotic plaque.
2. Correction of peroxidation and apoptosis processes.
3. Correction of rheological parameters of blood and microcirculation.
4. Efferent methods: plasmapheresis, lymphopheresis.
5. Symptomatic therapy is aimed at correcting metabolic, functional disorders and organic changes, includes vasodilators, hepatoprotectors, enzymes, and reparants.
6. Surgical methods for the purpose of revascularization of the digestive organs are represented by 3 groups of interventions:
1) percutaneous endovascular angioplasty with stenting of the abdominal aorta, emergency surgery, laser recanalization;
2) reconstructive operations: endarterectomy, resection with prosthetics, implantation;
3) operations aimed at creating new bypass paths: aortoarterial and interarterial bypass or anastomosis.
Indications for surgical correction of stenosis of the ES or mesenteric arteries are: stage of subcompensation or decompensation; the presence of stenosis of more than 50% of one or more unpaired visceral branches of the abdominal aorta. The presence of an occlusive process is a direct indication for surgery. Contraindications to surgery are acute cerebral or coronary insufficiency, previous ischemic stroke, myocardial infarction less than six months ago, heart failure of 2-3 degrees. The choice of method of reconstructive surgery is carried out taking into account the localization and prevalence of atherosclerotic lesions.
Symptomatic interventions:
- Sympathectomy
(intersection of the nerve plexuses responsible for spasm (narrowing) of the arteries) is performed for repeated blockages of the arteries and in addition to reconstructive operations. This operation improves blood circulation in the extremities by dilating small arteries. - Revascularization osteotomy
is also an adjuvant technique that improves blood circulation by stimulating the formation of new small vessels in the lower extremities after bone injury. - Arterialization of the venous bed
is rarely used at this time, since its implementation is associated with various technical difficulties, and long-term results are worse than the methods described above.
Methods for the prevention and treatment of varicose veins
Many people underestimate the seriousness of the problem of varicose veins, so they consult a doctor already in the last stages of the development of the disease. If treatment is not provided on time, it can cause the development of complications, which are much more difficult to deal with.
First, you need to see a doctor to make an accurate diagnosis. Next, the specialist prescribes specific treatment based on the individual characteristics of the body and the symptoms of the disease. The most common treatment methods are:
- Using compression garments – tights, stockings or socks;
- Drug treatment with special drugs that have a vasoconstrictor, venotonic and angioprotective effect on venous vessels;
- Surgical intervention. Most often these are minimally invasive treatment methods: phlebectomy, sclerotherapy, EVLT, RFO.
Prevention of varicose veins includes regular physical activity (aerobics, walking, swimming, yoga), nutrition control, giving up bad habits and a comfortable, comfortable wardrobe.
Discussion
The optimal condition for performing robot-assisted operations was a sufficient gap between calcifications in the infrarenal aorta for adequate clamping without the risk of damage to the arterial wall.
Rice. 3. Results of multislice computed tomography angiography with 3D reconstruction of the infrarenal aorta and arteries of the lower extremities after surgery
During the operation, the advantages and disadvantages of using robot-assisted operations in vascular surgery were established. The advantages of such operations include increased accuracy, visualization and maneuverability of manipulators, which have virtually no boundaries in the planes of movement [5], as well as reduced invasiveness of the surgical operation, which reduces the number of hospital days. The disadvantages of robotic technology include the high initial cost of the robotic system and the additional cost of consumables [6], as well as the duration of the operation, which is slightly higher than with classical operations. However, with regular use of robotic systems and accumulation of experience with robot-assisted systems in vascular surgery, the duration of these operations will decrease to the level of classical operations, and perhaps even become shorter.
Consequences
Among the causes that provoke various diseases of the blood vessels of the legs, heart, and brain, stenosing atherosclerosis occupies a leading position.
- If the coronary vessels are affected, symptoms of cardiac ischemia occur. Coronary heart disease makes itself felt by chest pain and shortness of breath during exercise. This diagnosis ends with myocardial infarction. Every year, thousands of people are admitted to cardiology hospitals in Moscow due to atherosclerosis of the heart vessels.
- When stenosing atherosclerosis affects the arteries of the vascular system of the legs, obliterating atherosclerosis of the lower extremities occurs - a disease that threatens disability and amputation of the limb.
- Atherosclerotic plaques in the vessels supplying the kidneys lead to the development of renovascular hypertension and renal dysfunction.
- If the neck vessels narrow and the arteries supplying blood to the brain (BCA - brachiocephalic arteries) are blocked, stenosis in the damaged area leads to cerebral ischemia and stroke. Read more about stenosing atherosclerosis of the brachiocephalic arteries and its consequences in the following publication.
At-risk groups
Patients with the following problems are most susceptible to vascular diseases of the lower extremities:
· Long history of smoking;
· Diabetes mellitus types 1 and 2;
· Alcohol abuse;
· Prolonged physical inactivity;
· High blood pressure;
· Hypercholesterolemia (increased concentration of cholesterol and triglycerides in the blood);
· High level of non-proteinogenic amino acid homocysteine in the blood;
· Obesity;
· Severe hormonal imbalance.
Pathologies of blood vessels and arteries of the legs mainly affect people who have crossed the threshold of fifty years of age, but in the last few years their active spread has also been observed among the young population. Men are more susceptible to such diseases than women.
It should be emphasized that most vascular dysfunctions are of a psychological nature, and people with a stressful type of character are most susceptible to them.
It is important to have a family history of disorders. This is especially true for atherosclerosis and varicose veins.
Common diseases of blood vessels and arteries of the legs
Due to the global spread of vascular pathologies of the lower extremities, some people consider them to be normal, since disorders associated with them are observed in every second adult patient. But this does not mean that these diseases do not need treatment. Neglecting their therapy can result in extremely serious complications, therefore, if alarming symptoms are detected, it is important to consult a doctor for differential diagnosis and selection of the correct treatment tactics.
In medical practice, such diseases are divided into several groups:
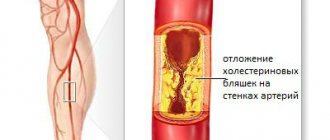
Atherosclerosis obliterans (OAOS) is a chronic degenerative metabolic process associated with hardening of arterial walls against the background of excessive deposits of lipids and cholesterol. These substances, in turn, become catalysts for the formation of atherosclerotic plaques, which can gradually narrow the lumens of blood vessels and lead to their absolute closure, associated with impaired nutrition and tissue viability.
Atherosclerosis is one of the leading causes of disability and mortality worldwide. Its characteristic features:
- pain in the legs, aggravated by running, climbing stairs and fast walking,
- intermittent claudication syndrome.
Obliterating endarteritis is a rapidly progressing disease of the arteries of the legs, associated with a gradual narrowing of the lumen of blood vessels and necrosis of tissues deprived of blood supply. The nature of the pathology has not been thoroughly studied, but doctors consider the key cause to be an inflammatory process associated with the predominance of autoimmune antibodies in the vessel.
Signs of the disease:
- rapid fatigue of the limbs when walking,
- sudden cooling of the extremities without objective reasons,
- swelling,
- formation of ulcers.
Acute arterial obstruction is a disease that occurs as a result of an abnormal increase in blood clotting (hypercoagulation), as well as against the background of an inflammatory or atherosclerotic process, leading to modification of the vascular walls and a sudden cessation of blood flow. This pathology often causes acute arterial ischemia syndrome.
It is expressed mainly in arterial spasm of both the affected and healthy legs.
Varicose veins are a common disease characterized by degenerative changes in the superficial veins, in which there is a loss of their elasticity, stretching, rapid growth and the formation of additional nodes.
The symptoms of this pathology are quite specific:
- congestive swelling of the legs,
- convulsions,
- change in skin pigmentation,
- feeling of heaviness
- soreness and fatigue,
- Characteristic bumpy nodes appear under the skin, often accompanied by itching and burning.
This pathology is accompanied by such aggressive complications as acute thrombophlebitis and intense bleeding.
Thrombosis of the superficial venous system is a syndrome that often results from varicose veins with an adjacent infectious process.
Signs:
- severe hyperemia and acute pain in the limbs,
- the occurrence of infiltrates localized along the course of the affected vein.
Venous thrombosis is the process of thrombus formation associated with dysfunction of coagulation and blood flow, inflammation or disruption of the integrity of the venous wall.
Signs:
- rapidly growing swelling of the limb,
- severe hyperemia and hyperthermia,
- cutting pain
- bluish skin at the site of injury,
- arterial spasms.
An aneurysm is a diffuse or saccular protrusion of part of an artery associated with an expansion of the lumen of a blood vessel and a decrease in its tone (excessive stretching or thinning of the wall).
The disease manifests itself in:
- limb weakness,
- periodic pain that tends to subside on its own,
- numbness, pulsation, coldness of the affected area,
- formation of a tumor-like neoplasm under the skin.
Vascular network (telangiectasia) is an abnormal proliferation of subcutaneous capillaries, accompanied by a local accumulation of thin capillary lines of a blue, red or purple hue, resembling a cobweb, an asterisk or a chaotic mesh in shape. It is painless and does not pose a potential risk to the health and life of the patient. Amenable to gentle surgical and hardware treatment. In the vast majority of cases, it brings purely aesthetic discomfort to the patient.
How do doctors diagnose atherosclerosis of the BCA?
The primary diagnosis is made based on the patient’s complaints - the doctor collects anamnesis, finds out the symptoms and manifestations of the disease. But for an accurate diagnosis you will need to do several tests:
- Ultrasound diagnostics - the speed of blood flow in different arteries is determined, the localization of plaques can be determined, and their size can be determined. The method is as accurate as possible and allows you to determine the main echo signs of atherosclerosis;
- Duplex ultrasound (USDG BCS) - is performed in the area of the vessels of the neck, helps to determine the characteristics of the pathology, the condition of the arterial walls, the size of blood clots, the presence of narrowings;
- A blood test is an additional examination that detects cholesterol levels in the blood. This method does not provide an accurate clinical picture, since in some patients suffering from atherosclerosis the indicator is normal;
- MRI is a modern method that is rarely used, since a special contrast agent must be injected into the vessel. But it is possible to find out the exact configuration of the plaques and their location.
Angiography for confirmed atherosclerosis is contraindicated - it can provoke a blood clot and blockage of blood vessels. A qualified doctor resorts to this method only in extreme cases.
Additionally, an ECG of the heart is prescribed to understand whether there are complications and whether the functioning of the main muscle of the body is normal. Therapy can be prescribed only after a comprehensive and comprehensive examination.
- Stenosing atherosclerosis of the brachiocephalic arteries (BCA): treatment and what is the prognosis for life?
Varieties
The disease manifests itself in different vessels, for example, the place of localization may be the carotid artery.
Depending on where the pathological changes occur, atherosclerosis can affect such important arteries as:
- sleepy;
- vertebral;
- subclavian
Taking into account the nature of the development of the atherosclerotic process, the following types of disease are distinguished:
- Stenotic. Atherosclerosis of the extracranial sections of the brachiocephalic arteries with stenosis is characterized by transverse deposition of lipid formations on the internal structures of the vessel. This is accompanied by a gradual slight increase in formations, however, if treatment is not carried out, soon the lumen is completely blocked, and obliterating atherosclerosis develops, which is complicated by stenosis.
- Non-stenotic. It manifests itself as a longitudinal arrangement of lipid formations, as a result of which blood flow is disrupted, but the risk of developing stenosis is much less. Non-stenotic atherosclerosis of the extracranial brachiocephalic arteries has a favorable prognosis and is often effectively treated conservatively.
Return to contents
Difference between stenosing and non-stenosing atherosclerosis
Atherosclerosis is a chronic vascular disease that develops with age, and all people are susceptible to it. At the initial stage, the plaques in the vessels are small, but if they do not block the vessel by more than half, this condition is called non-stenotic atherosclerosis. In this case, there are simply no signs of atherosclerosis, and the person feels great. As the cholesterol plaque grows, the vascular lumen becomes blocked—arterial stenosis occurs. In this case, organs deprived of the usual amount of oxygen and nutrients suffer from ischemia. This explains why the diagnosis of “stenotic atherosclerosis” occurs mainly in older and elderly people.
Diet therapy
Usually the diet is prescribed for life. Any form of atherosclerosis is endogenous and completely depends on the diet and lifestyle of the patient. The table below shows permitted and prohibited products.
| Allowed | Prohibited |
| Lean meats – chicken, turkey, beef | Fatty meats, lard |
| Fish | Trans fats (margarine, spread) |
| Fresh fruits, vegetables | Sausages, frankfurters, other smoked meats |
| Sea kale | Mayonnaise, all fatty sauces |
| Bran, cereals | Fast food |
| Low-fat dairy products, cheeses | Fatty dairy products, cheeses |
| Chicory, herbal teas | Baking, flour |
Fast food is considered one of the most harmful foods that provokes high cholesterol, it is especially important to give it up for life
How OASNK is developing
The inner wall of healthy vessels is smooth and even. This allows blood to flow within the lumen of the vessel without any difficulty. With atherosclerosis, the inner wall of the artery becomes uneven and thickened due to cholesterol deposits (cholesterol plaques). This pathological process is called atherosclerosis. With further development of the disease, narrowing or complete blockage of the arteries occurs, which leads to a significant decrease in blood flow to the legs. The consequence of this is the appearance of pain in the calf muscles when walking (intermittent claudication), numbness, and chilliness in the feet. As the disease progresses, pain in the legs becomes constant. Ultimately, trophic ulcers and necrosis appear in the foot area. If no therapeutic measures are taken, the next stage of the disease may be gangrene (death) of the limb.