Your phone number:
Send
ATHEROSCLEROSIS: HOW IT HAPPENS
ATHEROSCLEROSIS: DIAGNOSTICS
The development of a treatment strategy for atherosclerosis fundamentally depends on the diagnostic results. It is necessary to determine with maximum accuracy the location of atherosclerotic plaques, the degree of damage to the arteries, as well as the general condition of the patient.
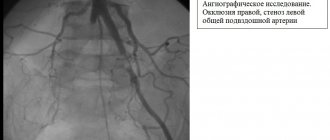
Diagnosis is made using clinical and instrumental methods. The “gold standard” for primary research is duplex ultrasound scanning of the arteries. If necessary, angiography can be performed - a contrast X-ray examination, which allows one to accurately determine the condition of blood vessels, the location and extent of damaged areas.
At the Vascular Surgery Clinic we use the most modern instruments, including the latest diagnostic ultrasound complex and a high-precision angiograph.
Depending on the diagnostic results, optimal treatment methods are selected.
ATHEROSCLEROSIS: CONSERVATIVE METHODS
I would like to warn you right away: the possibilities of conservative treatment are limited. Various products that, according to advertising, can “clean blood vessels” are not able to effectively fight the formed cholesterol plaques and restore the patency of the arteries.
Conservative therapy is aimed at reducing the risk of thrombosis, improving blood microcirculation, protecting tissues from “oxygen starvation,” and creating additional blood flow paths that “bypass” the affected areas of the arteries.
ATHEROSCLEROSIS: SURGICAL METHODS
Without belittling the role of conservative treatment as an element of complex therapy, I note that it is possible to radically restore the functionality of the arteries exclusively using vascular surgery methods.
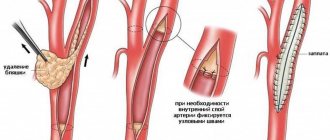
Basic technologies for surgical treatment of arteries affected by atherosclerosis include:
- Balloon angioplasty is the expansion of the lumen of an artery using a miniature balloon inserted into the vessel. When filled with air, the balloon expands and straightens the narrowed artery.
- Stenting is the installation of a mesh frame inside the artery, rigidly fixing the walls and preventing any deformation of the vessel.
- Bypass surgery – creation of additional artificial channels for blood flow
- Prosthetics – replacement of damaged areas of a vessel with artificial ones
If disturbances in blood flow have led to the appearance of ulcers, tissue death, and the development of inflammatory processes, then restoration of arterial patency must be combined with local therapy and methods of purulent surgery (For more details, see the article “Treatment of gangrene and critical ischemia”).
| Make an appointment with Professor Matveev |
SURGICAL METHODS: PRECISION AND LOW-TRAUMATIC
Modern medical technologies make it possible to perform low-traumatic intravascular (x-ray endosurgical) operations on the arteries. Instead of a large incision, there is a puncture through which a special long catheter is inserted into the artery, which is brought along the vascular bed to the affected area and then serves as a conductor for balloons and stents. In addition to the absence of postoperative scars (an important, but not the main advantage), intravascular operations do not require anesthesia, reduce rehabilitation time and minimize the likelihood of complications.
When choosing a surgical intervention technology, we give preference to X-ray endovascular methods, which ensure maximum efficiency and safety.
ATHEROSCLEROSIS: ISSUES OF PREVENTION AND REHABILITATION
Although there is still no unified theory of atherosclerosis, basic rules have been identified that can significantly reduce the risk of the occurrence and progression of this disease. These rules also apply to the postoperative rehabilitation period. Generally speaking, the recommendations are quite simple and boil down to following a healthy lifestyle:
- quitting smoking and alcohol,
- active lifestyle
- specialized anti-atherosclerotic diet (not too burdensome)
- body weight control
- maintaining psychological comfort
Atherosclerosis is a rather insidious disease that can enter a threatening phase with virtually no alarming symptoms. Therefore, I would like to recommend, if possible, to undergo examination by a vascular surgeon - this can identify the presence of the disease at an early stage and avoid surgical intervention.
| Make an appointment with Professor Matveev |
DON'T WASTE TIME! FORGET ABOUT THE DISEASE! GET YOUR BEAUTIFUL AND HEALTHY LEGS BACK!
Causes
The main cause of atherosclerosis of the vessels of the lower extremities is a violation of lipid metabolism - an increase in the level of cholesterol in the blood, and especially its “dangerous” fraction of low-density lipoproteins (LDL). However, an increase in high-density lipoproteins (HDL) does not cause atherosclerosis.
Elevated cholesterol levels alone are not enough to cause the disease. There must also be risk factors that affect the vulnerability of the artery wall, its protective properties, etc. These include:
- Smoking is the most dangerous risk factor and needs to be discussed separately. Even smoking several cigarettes a day leads to damage to the vascular endothelium; with high cholesterol, this gives a high risk of cholesterol deposition at the site of the lesion and the beginning of plaque formation. When smoking a large number of cigarettes per day, this risk increases significantly.
- Hypertonic disease
- Overweight
- Diabetes
- Alcohol abuse
Phlebitis
This is inflammation of the walls of the veins with subsequent disruption of blood vessels and deterioration of blood circulation. The main reasons for the development of phlebitis are as follows:
- Varicose veins.
- Infectious diseases.
- Injuries.
Signs of phlebitis:
- The affected vein becomes deformed, increases in size and becomes dense.
- The skin at the site of the affected vessel turns red and its temperature rises.
- The sore leg becomes uncomfortable and may swell.
The disease can be both acute and chronic. With phlebitis, thrombophlebitis often develops, that is, in addition to inflammation of the walls of the veins, their blockage (partial or complete) with a blood clot is added.
Treatment will depend on the causes of phlebitis. Typically, patients are prescribed anti-inflammatory drugs in the form of tablets or injections, and anticoagulants to prevent increased blood clotting and the formation of blood clots.
Symptoms, diagnosis
The main and earliest symptom of obliterating atherosclerosis of the arteries of the lower extremities is intermittent claudication. When walking a certain distance, the patient begins to feel fatigue, heaviness in one or both legs, and then pain, forcing him to stop and continue moving after a short rest.
The stage of the disease is even determined by the length of the pain-free walking distance. From 500 m to 1 km – stage 1, from 200 to 500 m – stage 2A, less than 200 m – stage 2B, less than 50 m and pain at rest – stage 3. Stage 4 of atherosclerosis of the extremities is gangrene.
When examining the patient, attention is drawn to a decrease in the calf muscles, dystrophy of the nail plates, and a decrease in the amount of hair on the legs. A characteristic symptom is the absence of pulse in the feet, popliteal, and femoral arteries (depending on the level of the lesion).
Important methods for diagnosing atherosclerosis of the vessels of the lower extremities are ultrasound (ultrasound ultrasound, doppler ultrasound, duplex angioscanning), angiography.
Narrowing of blood vessels in the legs: how is stenosis diagnosed?
What to do if symptoms of the disease are detected? In order to avoid an unfavorable prognosis due to narrowing of the blood vessels in the legs, you should plan a visit to the doctor as soon as possible. During it, the specialist will:
- a thorough survey to judge the development of a particular disease, its possible causes, and also to preliminarily assess the severity of the patient’s condition;
- examination of the legs to assess the condition of the skin;
- palpation of the extremities for pain, pastiness and compaction along the vessels.
After a physical examination, the doctor prescribes the necessary laboratory diagnostics of the patient’s condition. This may include:
- general clinical tests;
- extended hemostasiogram;
- lipid profile;
- immunogram;
- D-dimer test;
- analysis of blood composition for gases and acidity.
Diagnosis of narrowing of blood vessels in the legs
In turn, instrumental diagnosis of the disease is carried out in various ways: Dopplerography, duplex and triplex scanning, sonography, X-ray contrast angiography, electrocardiography, EchoCG, infrared thermography, rheoencephalography, etc. The most informative methods are considered to be contrast angiography and tomography with contrast. The selection of the optimal diagnostic method or their combination is made by the doctor individually in each specific case.
Treatment of atherosclerosis of the vessels of the lower extremities
Lifestyle changes, non-drug treatment
Patients with atherosclerosis of the arteries of the extremities, as a rule, need to change their lifestyle.
First of all, you need a COMPLETE cessation of smoking. Reducing the number of cigarettes smoked, of course, has a positive effect on the course of the disease, but the risk of damage to the vascular wall still remains.
Overweight patients need to lose weight.
An important factor in reducing blood cholesterol levels (especially its dangerous fractions - LDL) is following a diet low in animal fats.
Patients suffering from hypertension and diabetes mellitus need to be monitored by an appropriate specialist (therapist, endocrinologist) to correct these diseases.
Against the background of drug correction, training for the development of collateral circulation is desirable. The fact is that with obliterating atherosclerosis, the main vessels are affected. In this case, blood circulation begins to occur through small bypass (collateral) vessels. With good development of collateral circulation, limb ischemia can be minimized even with complete closure of the lumen of the main artery. Along with medications that help improve collateral circulation (they will be discussed below), training walking is used using special techniques on a treadmill and just on foot.
Recommendations for training walking: patients are recommended to walk 2-3 hours a day, not at a fast pace, so that there is no pain in the legs. At the same time they exercise on a treadmill. They start by selecting a walking speed along the path that does not cause fatigue in the legs for at least 10 minutes of continuous walking. Then increase the speed by 0.5 km/h. They begin walking at this speed, when fatigue and pain in the lower leg appear, they rest until the discomfort completely disappears, then they resume walking again until discomfort appears. The average walking time on the path is 30-40 minutes per day. The goal is to increase the distance of pain-free walking to 1.5 km, after which the walking speed is increased by another 0.5 km/h, etc. Training should be done under the supervision of a doctor.
Thrombophlebitis
This disease is characterized by inflammation of the walls of the veins with a simultaneous increase in blood viscosity, the formation of blood clots, narrowing of the lumen of blood vessels and poor circulation. Blood clots are life-threatening because they can break off and enter any part of the circulatory system, including the pulmonary artery. Often thrombophlebitis of the lower extremities develops with varicose veins, but there are other causes of the pathology:
- Infectious diseases.
- Injuries of the lower extremities.
- Increased blood clotting.
- Changes in blood composition, for example, as a result of taking certain medications.
- Pregnancy and childbirth.
Thrombophlebitis that develops with varicose veins usually affects the lower part of the thigh and the upper third of the lower leg. The following symptoms are noted:
- general deterioration of health (malaise, fever);
- pain in the area of the affected vessel, which intensifies with movement;
- redness and shine of the skin in the projection of the affected vein;
- swelling of the affected leg and its noticeable difference in size from the healthy one;
- infiltrates in the form of cord-like seals are easily palpable.
Treatment of thrombophlebitis primarily involves taking blood thinners to prevent blood clots, followed by anti-inflammatory drugs. If a blood clot is present, surgical intervention is indicated to remove the blockage of the vein. In addition, it is necessary to wear compression hosiery, use gels, massage, and physical exercises that improve blood circulation in the veins.
Drug treatment
There are many medications that are used for obliterating atherosclerosis of the lower extremities.
They can be divided into several groups:
- Antiplatelet agents - thrombo ACC, cardiomagnyl, trental, plavix, reopoliglucin.
- Drugs that reduce blood viscosity - vesel due f (sulodexide), phlogenzyme, wobenzym.
- Agents that improve peripheral blood circulation and microcirculation - alprostan (vasoprostan), nicotinic acid, xanthinol nicotinate.
- Agents that promote the development of collateral circulation - Actovegin, solcoseryl.
- Drugs that lower blood cholesterol levels - Torvacard, Crestor, etc.
- Other medicines – chimes, analgesics (for pain), antibiotics (for purulent-necrotic ulcers), etc.
Typically, patients are permanently prescribed one of the acetylsalicylic acid drugs for life - thrombo-ass or cardiomagnyl. Other drugs are prescribed in courses, depending on the stage of the disease and clinical manifestations.
It is believed that twice a year patients require hospitalization in the vascular surgery department for courses of conservative therapy - intravenous infusions, hyperbaric oxygen therapy, physical therapy.
Surgery
Surgical treatment is possible in the presence of narrowings (stenoses) of large vessels, mainly in the popliteal-femoral segment or above. Reconstructive operations for damage to the arteries of the leg are practically not used.
For small stenoses, stenting is possible - installing a stent in the area of stenosis in a minimally invasive way (through a puncture in the femoral artery), which restores the patency of the artery.
In case of significant narrowings, reconstructive operations on blood vessels are used - bypass surgery, prosthetics.
With timely and correct treatment of obliterating atherosclerosis of the vessels of the lower extremities, it is most often possible to stabilize the process and avoid late complications - trophic ulcers, gangrene.
Thrombosis
Inflammation of the deep veins and the formation of blood clots in them is called thrombosis. A thrombus quickly forms, and if it is not tightly attached to the wall of the vein, it can break off at any time and move along the vascular bed.
The main causes of thrombosis are as follows:
- congenital vascular pathologies;
- hormonal disorders;
- tumors;
- injuries with vascular damage;
- fractures;
- surgical interventions;
- leg paralysis and paresis;
- severe infections;
- excess weight.
In addition, provoking factors include:
- elderly age;
- heavy physical activity;
- sedentary lifestyle;
- prolonged bed rest and immobility;
- bad habits (drinking alcohol, smoking).
Symptoms of the disease are not always clearly expressed. Thrombosis can be suspected based on the following signs:
- Bursting, tugging, squeezing pain in the evening.
- Numbness and crawling in the lower legs.
- Heaviness in the leg at the end of the day.
- Swelling and increase in volume of the affected limb.
- Thinning of the skin of the affected leg, pallor and cyanosis.
- Glossy leather.
- Increase in temperature (general and local).
- Filling of the superficial veins with blood and their pronounced pattern under the skin.
- The temperature of the diseased leg is lower than that of the healthy leg.
Treatment of thrombosis can be conservative and surgical. In the first case, drugs of the following groups are prescribed:
- anti-inflammatory;
- anticoagulants of direct and indirect action;
- enzymes with thrombolytic properties;
- agents that improve microcirculation and blood fluidity.
In addition, elastic bandaging or wearing compression stockings is recommended.
Surgical treatment is prescribed for severe inflammation, a floating thrombus and a high risk of thrombus rupture with subsequent development of pulmonary embolism. The most common operation is thrombectomy, during which the clot is removed and blood flow is restored.