Surgeon
Bohyan
Tigran Surenovich
Experience 36 years
Surgeon of the highest category, Doctor of Medical Sciences, member of the International Association of Surgeons, Gastroenterologists and Oncologists
Make an appointment
Lymphostasis of the lower extremities is lymphatic edema, which is caused by the fact that the outflow of lymph is disrupted and it stagnates in the tissues. It is visually clear that the leg that is susceptible to this disease is enlarged and swollen. But let's talk about the symptoms in more detail.
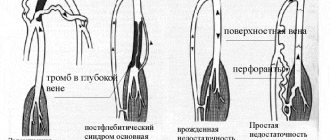
What is venous stagnation: types of venous hyperemia
Venous hyperemia (or plethora) can be local or generalized. In the first case, the disturbance of blood outflow is localized in one part of the body or a specific organ; in the second, we are talking about changes in blood flow in the entire venous circulatory system. Most often, generalized venous congestion develops against the background of heart disease - coronary artery disease, acute myocardial infarction, heart defects, etc. Based on the speed and intensity of development of the pathological process, acute and chronic forms of venous congestion are distinguished.
The topic of venous hyperemia is quite extensive, so in this article we will talk about one of its forms - venous stagnation in the vessels of the lower extremities.
Reasons for appearance
The most important factor in the occurrence of vein diseases is hereditary predisposition. It is this that determines the characteristics of the condition of tissues and blood vessels.
Another reason is associated with diseases and conditions caused by problems with venous circulation: thrombosis, trauma, varicose veins.
The third group of factors includes lifestyle: passive lifestyle, excess weight, excessive loads that involve lifting heavy objects. No less significant factors are the age category and hormonal background of the patient.
Doctors consider the following people at risk:
- athletes;
- women (pregnancy and changes in hormonal levels can affect venous circulation);
- people who have a family history of venous disease.
Causes and mechanisms of development of venous hyperemia of the legs
Impaired blood flow from the legs to the heart forms the prerequisites for the development of CVI - chronic venous insufficiency. This pathological condition is one of the most common diseases of the cardiovascular system: according to statistics, up to 40% of the adult population in Europe and the USA suffers from chronic venous insufficiency of the lower extremity vessels.
Venous congestion in the elderly
The causes of venous stagnation may be the following:
- Vascular diseases (varicose veins, thrombosis, phlebitis, etc.) Vein diseases are often associated with hyperemia, since in most of them there is a malfunction of the venous valve pump, decreased tone and fragility of blood vessels.
- Sedentary lifestyle and prolonged stay in a fixed body position. If a person spends most of his time sitting or standing, this leads to a slowdown in the blood circulation in the lower extremities. For this reason, it is extremely important to prevent disruption of blood flow in the legs of patients who are lying down.
- Leg injuries. Injuries almost always involve a violation of the integrity of the vascular wall. As it recovers, a blood clot or scar may form at the site of injury, preventing normal blood flow.
- Obesity. Excess weight puts increased pressure on the lower extremities, which impairs blood circulation in them and causes symptoms of venous stagnation.
- Pregnancy. During pregnancy, changes occur in a woman’s body that affect the entire cardiovascular system: there is a decrease in the speed of blood flow in the deep veins of the legs, a decrease in the tone of vascular smooth muscles, and an increase in blood clotting in late pregnancy. In addition, fetal growth can provoke compression of the pelvic veins, which in turn causes a disruption in the outflow of blood from the legs to the heart.
Expert opinion
An increase in body weight during pregnancy, in combination with the above-mentioned prerequisites for the development of CVI, creates favorable conditions for the occurrence of venous stagnation in the lower extremities. During pregnancy, many women note the appearance of telangiectasias (venous “stars”) and varicose veins on their legs. Based on this, expectant mothers are recommended to regularly visit a phlebologist during pregnancy.
Vascular surgeon, phlebologist
Osipova Ekaterina Yakovlevna
- Age-related changes. As the body ages, the condition of the veins may worsen: this is influenced by the presence of concomitant systemic pathologies, a decrease in vascular tone due to menopause, as well as a gradual deterioration in the blood flow of the veins and capillaries. As a result, older people are more likely than younger people to complain of signs of venous stasis.
Symptoms based on stage
Symptoms of lymphostasis of the lower extremities differ depending on the stage of the disease. In the first stage, the swelling is mild and reversible. It usually appears in the evening and is localized near the toes, in the ankle joint, and on the back of the foot. The tissues remain quite soft, and in the morning these manifestations disappear, the leg looks normal.
At the second stage, the swelling is already irreversible. This means that it does not fall off in the morning, but constantly maintains its shape. The connective tissue grows, the swelling itself gradually rises. All this can last for years, the situation worsens gradually. Over time, the skin over the swelling cannot be folded; it seems to be stretched. At the same time, a feeling of discomfort, heaviness appears, and pain begins. In places where the skin comes into contact with clothing and friction, wounds and ulcers may appear, from which lymph oozes. The skin also takes on a bluish tint.
At the third stage, the so-called elephantiasis disease is observed - this is the most complex stage of the disease. It is characterized by dangerous complications: fibrosis, ulcers of various types, loss of limb contours and much more. All this greatly affects the patient’s physical capabilities, as well as his psychological state.
There are also more general symptoms of lymphostasis of the lower extremities. These include severe fatigue, weakness, headaches, severe weight gain (even obesity), and joint pain. Due to physical and mental stress, a person’s concentration decreases, he becomes more distracted, and it is more difficult to cope with simple tasks.
Obviously, in this case it is better not to bring it to the third stage and consult a doctor as quickly as possible.
Do you have symptoms of lymphedema of the lower extremities?
Only a doctor can accurately diagnose the disease. Don't delay your consultation - call
Symptoms and signs of venous hyperemia
The pathological process manifests itself in the form of swelling, pastiness of soft tissues, changes in the color of the skin, increased vascular patterns, impaired sensitivity, the appearance of cramps, rapid fatigue, a feeling of fullness in the legs; Difficulties appear when walking and performing physical activity.
Ultrasound diagnosis of venous hyperemia
Chronic venous insufficiency. Complications
Disturbances in venous outflow lead to both the extreme degree of chronic venous insufficiency (CVI) - venous trophic ulcers, and thrombosis associated with slow blood flow and chronic inflammation of the venous wall.
Varicose veins and venous insufficiency in the form of ulcers
Medical complications of chronic venous insufficiency not only sharply worsen the quality of life, but also pose a direct threat to it.
How to cure venous congestion in the legs?
Therapy involves relieving the unpleasant symptoms of hyperemia and normalizing blood circulation during venous stagnation. For this, the patient is prescribed decongestants, antispasmodics, anticonvulsants, NSAIDs, phleboprotectors, and anticoagulants. An important role is given to weight normalization, lifestyle correction, and wearing compression stockings. Along with taking medications prescribed by a phlebologist, you can use additional means - for example, Normaven® products. Clinical studies have shown that regular use of the Leg Cream has improved the condition of the veins of the lower extremities in 95.5% of subjects.
Prevention and treatment of venous stagnation in the legs
Varicose veins as one of the causes of chronic venous insufficiency
By the term “chronic venous insufficiency”, modern medical science means a symptom complex associated with impaired venous outflow. Chronic venous insufficiency (CVI) is caused by a number of diseases that lead to disruption of the normal functioning of the venous system, most often of the lower extremities.
The clinical picture of chronic venous insufficiency is very diverse and depends on the stage of the disease.
Prevention of venous stagnation
- Do as much physical activity as you can.
- Eat right. Nutrition for venous stagnation should include foods rich in fiber, rutin and vitamin C.
- Avoid prolonged static loading.
- Avoid wearing high heels and tight pants.
Sources:
- Sklyarova N.P., Bakhteeva E.R. Organizational aspects of the prevention of postoperative venous thromboembolic complications and pulmonary embolism. // Chief physician of the South of Russia. – 2011. – No. 4 (27). – pp. 25-26.
- Zhane A.K., Zhane Ad. K., Napso H.R., Zhane T.I., Pichugin A.G. Possibilities of diagnosis and treatment of chronic diseases of the veins of the lower extremities. // Kuban Scientific Medical Bulletin. – 2010. – No. 9 (123). – pp. 78-84.
- Safonov L.V. Modern aspects of the prevention of venous circulation disorders of the lower extremities in athletes due to transport physical inactivity. // Bulletin of sports science. – 2009. – P. 36-38.
- Lukyanov V.V., Bondarenko A.V., Bondarenko A.A., Peleganchuk V.A. Disturbances of venous hemodynamics and thromboembolic complications during osteosynthesis of fractures of the lower extremities. // Polytrauma. – 2009. – No. 4. – P.32-28.
- Pisarev V.V., Lvov S.E., Kutyreva O.I., Molchanov O.S. Features of antegrade blood flow and venous thrombotic complications in patients with fractures of the tibia and femur. // Traumatology and orthopedics of Russia. – 2009. – No. 2 (52). – pp. 33-28.
- Bykov A.V., Nazaruk A.S. Selective surgical interventions for varicose veins of the lower extremities. // Bulletin of Volgograd State Medical University. – 2004. – No. 11. – P. 66-68.
For an accurate diagnosis, contact a specialist.
Treatment
Since the disease is caused by many factors, treatment of leg lymphostasis represents a whole range of measures. A conservative approach, including massage, a special diet, and the use of certain medications, is implemented only in the first stage of the disease. At the same time, doctors give many additional recommendations:
- avoid heat exposure. That is, you need to exclude baths, saunas, solariums, etc.;
- wear soft, non-compressive shoes without heels;
- avoid long static loads. It is not allowed to sit or stand for a long time; it is necessary to move moderately;
- eliminate unnecessary physical activity, especially excessive;
- wear only soft and loose clothing;
- make sure that the skin of your feet is always moisturized and does not rub against clothes and other things, etc.
It is important to fully comply with the list of restrictions that the doctor will indicate - with such an illness, even a minimal wound or unwanted ulcer can greatly complicate the matter.
But treatment of lymphostasis of the lower extremities is not limited to only the listed recommendations. Common methods to combat this problem include the following:
- kinesiotherapy, compression treatment. In the first case, it means performing lymphatic drainage massage, as well as performing physical therapy exercises. In the second case, we are talking about wearing special underwear, as well as bandaging, which, using pressure, changes the redistribution of lymph;
- drug therapy. It is difficult to list specific drugs here, because depending on the situation, drugs from more than ten categories are used. These include diuretics, phlebotropic agents, and much more - everything is prescribed individually;
- physiotherapeutic methods. Magnetic therapy, laser therapy, ultraviolet irradiation and much more help alleviate the patient’s condition;
- surgical intervention. It is indicated in critical cases when other methods cannot cope with the problem.
The sooner treatment is started, the higher the chance that leg lymphostasis will be neutralized and the patient will continue to live a full life. The further the disease develops, the more serious the risks of disability and irreversible changes. As a rule, the disease does not threaten the patient with death, but at the same time it deprives him of the ability to do many simple things (even normal movement), greatly reduces the quality of life, and has a bad effect on the psyche.
Ekaterina Misheneva: “Don’t let the blood stagnate”
Today in Russia, mortality from cardiovascular diseases directly related to thrombosis is twice the European average and amounts to more than 1.5 thousand people per hundred thousand population. Ekaterina Misheneva, a cardiologist at the State Institution of the Republic of Kazakhstan "Cardiological Dispensary", spoke in an interview with Respublika about what kind of disease this is and who is susceptible to it.
– So what is thrombosis?
– Thrombosis is a blockage of a vessel with a blood clot, while blood does not enter the organ, and it may suffer. Most often, a person's limbs are affected. In the body of a healthy person, the formation of such a clot helps stop bleeding. For example, if you cut yourself or have your blood taken for a test, the bleeding will stop after a while. But sometimes it also happens that thrombosis occurs when it should not exist, that is, for no apparent reason. Sometimes this causes myocardial infarction (a blood clot in the arteries that supply the heart muscle) or a stroke (a blood clot in the arteries of the brain). And this can threaten not only health, but also life. Such thrombosis can also occur due to certain characteristics of genes, i.e. hereditary information recorded in the cells of your body. Therefore, if a person wants to connect his life with a profession that involves high-risk situations, for example, working as a rescuer, police officer, or in professional sports, he should undergo a molecular genetic examination. Problems begin when blood clots, attaching to the walls of blood vessels, form a plug, which at any moment can break off, set sail through the veins and arteries and, once in a bottleneck, completely block the blood flow. And the man suddenly dies. Everyone is afraid of plane crashes, but few people know that after a safe landing you can collapse dead right on the plane's ramp - due to a blood clot that has formed in the veins during the flight. It is believed that blood clots form in one of the passengers on every flight. Fortunately, not every case ends in tragedy. According to statistics, 70 percent of people experience thrombosis.
– Why do blood clots occur? Can the danger be identified? And how to protect yourself from the threat?
- Let's figure out why blood clots occur in the veins. For blood clots to form, a combination of three factors is necessary. The first factor is damage to the inner surface of blood vessels (occurs after traumatic, tumor or inflammatory diseases). The second is a slowdown in blood flow (occurs with heart failure, prolonged bed rest and varicose veins). And the third is increased blood clotting (noted during injuries, inflammatory processes, surgical interventions and dehydration). Sometimes one reason is enough. If all three are present, thrombus formation is inevitable. There are two types of thrombosis - venous and arterial. Venous is more common. It is dangerous for its complications, the most severe of which is thromboembolism (blockage of branches) of the pulmonary artery. Surgeons claim that this diagnosis explains a third of cases of sudden death. More than half of patients die in the first two hours after the onset of embolism. Arterial blood clots are less common, but they are more insidious. Being in fast blood flow, they more often come off, first causing disruption of the blood supply to the organ that the artery supplies with blood, and then its death. Thus, thrombosis of the coronary arteries leads to myocardial infarction, and of the cerebral arteries - to a stroke. Veins are quite delicate and easily wounded anatomical formations. Their walls are much thinner than those of arteries of the same diameter. Blood pressure in the veins is much lower, so the middle (muscular) layer is less developed. Veins are less resistant to external compression and injury; they are easily involved in the inflammatory process even without the participation of microorganisms. In addition, the veins have valves, damage to which and stagnation of blood in the area where they are located contribute to the formation of blood clots. Maintaining blood in a liquid state is ensured by the simultaneous operation of a huge number of complex biochemical mechanisms. They maintain a precise balance between the coagulation and anticoagulation systems of the blood. There are a large number of typical situations, well known to doctors, in which venous blood flow is simultaneously disrupted and the coagulation system is activated. For example, during any surgical operation, a large amount of tissue thromboplastin, a substance that stimulates blood clotting, enters the bloodstream from the tissues. The more severe and extensive the operation, the greater the release of this substance. The same thing happens with any injury. This mechanism was formed in ancient times, and without it humanity as a biological species simply would not have survived. Otherwise, any injury to our distant ancestors, and to us, would have ended in death from bleeding. The body as an integral system is indifferent to what caused the wound - the claws of a saber-toothed tiger or a surgeon's scalpel. In any case, the blood clotting potential is rapidly activated. But this protective mechanism can often play a negative role, since it creates the preconditions for the formation of blood clots in the venous system in operated patients.
– It is clear that any operation is a risk.
– On the first day after surgery, it is difficult for the patient to get up, move and walk. This means that the work of the muscular-venous pump is turned off and venous blood flow slows down. In case of injuries, in addition, it is necessary to apply plaster casts, skeletal traction, and connect bone fragments with metal pins, which sharply limits the patient’s physical activity and contributes to the occurrence of thrombosis. Its incidence after surgical operations on the abdominal organs can reach 25-40 percent. With hip fractures, knee and hip replacements, thrombosis in the deep veins of the legs develops in 60-70 percent of patients. The most serious problem is venous thromboembolic complications during pregnancy. The fact is that a woman’s body itself prepares in advance for childbirth, and therefore for blood loss. Already from the early stages of pregnancy, the blood coagulation system is activated. The inferior vena cava and iliac veins are compressed by the growing uterus. Consequently, the risk of thrombosis increases. Acute venous thrombosis may complicate the use of hormonal contraceptives. These drugs seem to deceive the woman’s body, “convincing” it that pregnancy has already occurred, and hemostasis naturally reacts by activating the coagulation system. Although pharmacologists try to reduce the hormone content, primarily estrogens, in these drugs, the incidence of venous thrombosis (and therefore the possibility of pulmonary embolism) in women taking hormonal contraceptives is at least 3-4 times higher than in those taking hormonal contraceptives. who doesn't accept them. The risk of blood clots is especially high in women who smoke, since nicotine releases thromboxane, a powerful blood clotting factor. Excess weight also actively promotes thrombus formation. Venous thrombosis is a common complication of neoplasms, both malignant and benign. Patients with tumors usually have increased blood clotting. This is apparently due to the fact that the patient’s body prepares in advance for the future disintegration of the growing tumor. Often, venous thrombosis acts as the first clinical sign of the onset of a cancer process. Even a long flight in a cramped airplane seat, with legs bent at the knees, and forced inactivity, can provoke vein thrombosis, the so-called “economy class syndrome.” Thus, any surgical intervention, any injury, pregnancy, childbirth, any disease associated with the patient’s immobility, circulatory failure, can be complicated by venous thrombosis and pulmonary embolism. This is precisely what explains such a high incidence of venous thromboembolic complications, even in countries with well-developed medicine.
– How to determine thrombosis by external signs? And who is more susceptible to this disease?
– The insidiousness of venous thrombosis also lies in the fact that its clinical manifestations do not cause the patient a feeling of great distress. Swelling of the leg, pain, usually of a moderate nature, and slight cyanosis of the limb do not frighten patients, and sometimes they do not even consider it necessary to see a doctor. In this case, without any warning, a blood clot can break away from the vein wall in a few seconds, turn into an embolus - a blood clot that migrates through the vessels, and cause severe thromboembolism of the pulmonary arteries with an unpredictable outcome. According to experts, about 100,000 people die annually from pulmonary embolism in the Russian Federation. Thus, this disease claims more lives than car accidents, regional conflicts and criminal incidents combined. Due to its transience and unpredictability, pulmonary embolism is perceived as a bolt from the blue not only by patients, but also by doctors. Fortunately, not every venous thrombosis is complicated by thromboembolism, although their number is very high. Blood clots are more often found in older people. Physical inactivity that accompanies a sedentary lifestyle provokes blood stasis - one of the main risk factors for the disease. One of the common causes of arterial thrombosis is atherosclerosis. Atherosclerotic plaques cause narrowing of the arteries. Blood flow becomes difficult, and favorable conditions arise for the formation of thrombosis. The relationship between smoking and the formation of atherosclerosis, and therefore the occurrence of blood clots, has been proven. But most often people who have a tendency to form blood clots - thrombophilia - are at risk of thrombosis. It can be genetic, associated with gene damage, and be inherited. And in some cases it may be caused by an imbalance of the coagulation and anticoagulation systems.
– Blood clots often form in the summer, why?
– There are several reasons for this. The main thing is travel, or rather, the air travel that accompanies it. Air passengers sit for a long time in uncomfortable positions, veins are pinched, and low pressure and extremely dry air in airplane cabins contribute to blood stagnation and rapid dehydration of the body. To avoid blood clots, before the flight you need to tighten compression hosiery (it improves blood flow in the legs), take a quarter of an aspirin tablet, which reduces blood viscosity. And during the flight, stretch your legs more often: try to get up and walk around the cabin after the plane has gained altitude, every 30 minutes. The second reason is the summer desire to lose weight. Blood clots are more likely to form in women who are on diets (removing excess fluid from the body is the basis of diets, and this is where dehydration of the body begins) or taking birth control pills (they increase blood clotting).
– Is it possible to sense the lurking danger?
– Symptoms of venous thrombosis are heaviness in the muscles (usually the calf muscles), swelling of only one lower limb, hardening along the veins, bluish skin, pain. If venous thrombosis is complicated by thromboembolism in the pulmonary arteries, then in addition to swelling and pain in one of the extremities, pain in the chest, aggravated by breathing, cough, hemoptysis, and increased body temperature are added. Often such patients are treated by a neurologist diagnosed with intercostal neuralgia or by a therapist diagnosed with pneumonia. Sometimes such “minor” embolism may not manifest itself at all until repeated episodes lead to more severe changes in pulmonary blood flow. Signs of arterial thrombosis depend on where the blood clot is located. With arterial blood clots in the arms or legs, patients complain of sharp pain, coldness in this limb and loss of sensitivity. If it is the arm, then it is often difficult to measure blood pressure or impossible to measure it at all. Blood clots in the abdominal arteries cause vomiting, diarrhea, and abdominal pain. Thrombosis of the cerebral arteries can manifest as a stroke. Blood clots in the coronary arteries - myocardial infarction - severe pressing or burning pain in the chest. However, about 30 percent of venous thrombosis may be asymptomatic. They are the most dangerous. To detect them, you need to undergo examinations. As a rule, routinely detected blood clots are not removed, but dissolved with special preparations.
– How are thromboses treated?
– The fight against deadly thromboembolism of the pulmonary arteries is primarily a fight against acute venous thrombosis. Of course, it is much more effective to prevent thrombosis than to treat it. That is why the problem of preventing venous thromboembolic complications is now attracting the attention of doctors of various specialties. This is why surgeons, oncologists, gynecologists, physical therapy doctors so persistently try to get their patients out of bed the next day after surgery, or even on the same day, in order to take a few steps around the ward (often hearing accusations from their patients of all the deadly sins ). By the way, the common phrase “movement is life” comes to mind in this case. If thrombosis of the main veins has already developed, then doctors direct all efforts primarily to preventing pulmonary embolism. Previous attempts to remove the thrombus completely turned out to be futile, since against the background of altered hemostasis, a new thrombus appears on the inflamed vein wall, more friable and even more dangerous. Venous thrombosis does not threaten the vitality of the leg, since the arteries that pass through the blood flow regularly bring oxygen and nutrients. Venous gangrene is a very rare complication; it develops if blood clots close absolutely all veins, both deep and subcutaneous. Therefore, simultaneously with antithrombotic or anticoagulant therapy aimed at preventing the growth and spread of a blood clot, the patient is examined to identify floating, embolic forms of venous thrombosis. For a long time, only phlebography was used for this, that is, x-ray examination of the main veins using a contrast agent. Currently, most patients can be diagnosed using ultrasound techniques. First of all, this is an ultrasound examination of the veins, which does not require puncture of the veins, the introduction of a toxic contrast agent and, which is very important, especially when examining pregnant women, is not associated with irradiation of the patient. At the same time, the information content of the study is not inferior to phlebography. But the most dangerous, often catastrophic course of the situation occurs when a pulmonary embolism has already occurred. Thromboemboli are usually large in size, and in most patients they close the pulmonary trunk or main pulmonary arteries.
– So how to protect yourself from blood clots?
– First of all, lead an active lifestyle - physical activity improves blood circulation, prevents blood stagnation, and improves metabolic processes in the body. It is necessary to eat properly - the basis of the diet should be plant foods that do not contain cholesterol. The body should not be dehydrated—lack of fluid increases blood viscosity. Take care of yourself: injuries, operations, infectious diseases are a risk factor for blood clots. Get tested on time. Ultrasound duplex scanning of veins, during which the diameter of the vein is measured and the speed of blood flow is determined. Often the blood clot itself can be seen on ultrasound. Donate blood for cholesterol, undergo a coagulogram (blood clotting test). Get a blood chemistry test (a high level of an indicator called D-dimer is a key indicator of thrombosis, but can be elevated in other diseases). In-depth studies for thrombophilia are quite expensive to do for anyone concerned about their health, but we still recommend them when one of the relatives (father, mother, brothers, sisters, uncles, aunts, grandmothers, grandfathers) have had thrombosis in the family or thromboembolism, as well as cases of sudden death of relatives under the age of 55 years. Or in case of thrombosis in a person under the age of 50 years. We also recommend it in case of causeless recurrence of thrombosis of any location. These examinations are necessary to determine a more accurate treatment method. Modern medicine has a wide range of tools for diagnosing and treating acute venous thrombosis and pulmonary embolism. Nevertheless, it should be remembered that the best way to combat this most dangerous complication is prevention, carried out in collaboration between the doctor and the patient. The fight against excess weight, uncontrolled use of hormonal drugs, smoking, physical inactivity, conscious and active implementation of medical recommendations can significantly reduce the frequency of tragedies and misfortunes caused by this disease.