Small focal leukoencephalopathy of vascular origin is a diagnosis that is more often given to male patients who have crossed the age threshold of 55 years, but not everyone knows what it is.
With leukoencephalopathy of the brain, the white matter in its subcortical structures is destroyed.
This type of disease is one of the types of encephalopathy, first described by the German psychiatrist and neurologist Otto Binswanger in 1894, and therefore was named after him.
The unclear description of the disease and the small number of examinations of patients with signs of dementia for a long time prevented many neurologists and psychiatrists from recognizing the pathology.
With the advent of computed tomography and magnetic resonance imaging, changes in the white matter of the brain associated with persistently elevated blood pressure, causing dementia, have been confirmed.
Treatment of the disease is carried out by neurologists and psychiatrists.
Leukoencephalopathy has varieties, but almost always we are talking about changes in the white matter of the brain. The type of disease determines the treatment regimen.
Lecoencephalopathy of vascular origin
Lecoencephalopathy of vascular origin (small focal) is a cerebrovascular pathological process.
The fundamental factor for the appearance of vascular leukoencephalopathy is constantly elevated blood pressure, as well as its systematic jumps.
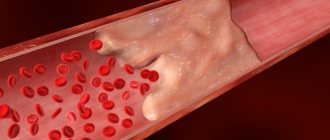
Arterial hypertension causes sclerosis of small cerebral vessels - capillaries, their ischemia, thickening of vascular walls, etc. As a result, the white matter that transmits nerve impulses undergoes atrophic changes. In this case it is observed:
- its reduction;
- decrease in density;
- fluid replacement;
- the appearance of numerous hemorrhages, cysts, small foci of destruction.
The ventricles of the brain begin to collapse.
Typically, the first signs of small focal leukoencephalopathy can appear in patients who have reached the age of sixty, and in case of a hereditary factor, even earlier.
Multifocal progressive vascular leukoencephalopathy
Multifocal progressive vascular leukoencephalopathy manifests itself with a viral infection of the central nervous system, which contributes to impaired immune function.
Weakening of the immune defense leads to the destruction of the white matter of the brain.
Pathological changes are provoked by immunodeficiency: HIV-infected (5%), AIDS patients (50%).
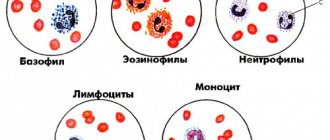
Also, modified leukocytes in leukemia lose the ability to fight infection, which contributes to the occurrence of immunodeficiency and, as a consequence, to pathological changes in the brain.
Exposure to viruses leads to focal damage to the sheaths of nerve fibers, enlargement and deformation of nerve cells. There is no involvement of gray matter in the process. The structure of the white matter changes, it softens and becomes gelatinous with the appearance of multiple small depressions on its surface.
This form of the disease poses a danger not only to the health, but also to the life of the patient. It should be noted that modern antiviral therapy has significantly reduced the prevalence of the pathology.
The manifestation of cognitive impairment can range from mild impairment to full-blown dementia. Focal neurological symptoms include: speech impairment and decreased vision, sometimes to the point of complete loss. Accelerated progression of movement disorders can cause severe disability.
Periventricular (focal) leukoencephalopathy
Periventricular (focal) leukoencephalopathy is extensive damage to the brain caused by a lack of oxygen or chronic disruption of its blood supply.
The areas of the cerebellum, brain stem and subdivisions responsible for human movements are affected by pathology. Prolonged lack of oxygen leads to dry necrosis (death) of the white matter. It develops rapidly and contributes to the occurrence of severe motor activity disorders.
Periventricular leukoencephalopathy can be triggered by fetal hypoxia and lead to cerebral palsy (CP).
Leukoencephalopathy - clinical forms, diagnosis
The medical term “leukoencephalopathy” is used to define a group of diseases accompanied by damage to the white matter and a number of deep structures of the brain.
Rapid progression leads to the formation of senile dementia. In children, there are vascular varieties, congenital forms with a long chronic course. The survival time for this type is longer compared to its multifocal counterpart.
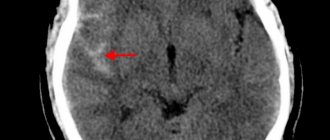
MR image of vascular leukoencephalopathy
To distinguish the pathology from a number of other neurodegenerative diseases with similar clinical symptoms, a classification according to ICD 10 has been developed, which clearly distinguishes the forms of the nosology.
Treatment
Modern medicine does not have methods that can completely rid a person of vascular leukoencephalopathy.
Self-treatment in this case is prohibited. When the first symptoms of the disease appear, it is necessary to urgently contact specialists: neurologists and psychiatrists, who, with the help of therapists, cardiologists, endocrinologists and other specialists, will draw up an individual treatment regimen, taking into account the peculiarities of the course of the pathology and the general health of the patient.
The goal of treatment is:
- slowing down the progress of pathological changes;
- relief of symptoms;
- restoration of the patient's mental state.
Treatment areas include:
- therapeutic measures aimed at combating the development of pathology;
- symptomatic treatment;
- correction of blood pressure, which ideally should not exceed 120/80 mmHg. Art. It should be remembered that the occurrence of hypotension is also undesirable, since a decrease in blood pressure can only aggravate the situation;
- elimination of spontaneous bowel and bladder emptying;
- rehabilitation;
- social adaptation.
Experts use the following medications:
- "Lisinopril" has cardioprotective, vasodilating, hypotensive effects;
- drugs that improve blood circulation in the brain: Cavinton, Pentoxifylline, Clopidogrel;
- nootropics to stimulate mental activity, improve memory and increase learning abilities: Cerebrolysin, Piracetam, Nootropil;
- angioprotectors that restore the walls of blood vessels: “Plavix”, “Cinnarizin”, Curantil”;
- antidepressants: Prozac;
- adaprogens that increase the overall tone of the body: “Aloe extract”;
- vitamins A, E, B;
- in some cases, antiviral drugs: Kipferon, Acyclovir;
- drugs from the group of acetylcholinesterase inhibitors that improve cognitive function: Rivastigmine, Donepezil, Galantamine, Memantine.
Reflexology and physiotherapy are not excluded: breathing exercises, massage, acupuncture, manual therapy sessions.
What is cerebral leukoencephalopathy
Damage to the white matter of the brain is caused in most cases by viruses. Vascular and discirculatory forms are caused by impaired blood supply to a certain area of the brain. Chronic ischemia causes irreversible changes.
Clinical symptoms of the disease more often occur when affected by papillomaviruses. The probability of nosology in patients with HIV is less than 6% according to brain MRI statistics in St. Petersburg.
Forms of vascular origin progress slowly. The chronic course of the disease is characterized by gradual irreversible tissue damage. Mild ischemia provokes the formation of small necrotic areas. Diffuse location leads to neurological disorders.
Leukoencephalopathy with cerebral calcification and cysts
A 10-year-old boy, weighing 23 kg, born from an unrelated union (the birth was without complications); complains of pulsating headaches for 1 year, mainly in the frontal and occipital regions, almost continuous; the pain intensified when coughing and prevented the patient from sleeping and studying. The boy was hospitalized after an exacerbation of headache, which was accompanied by repeated vomiting and partial attacks in the form of clonic twitching of the muscles of the left half of the face. Objective examination revealed no abnormalities.
Ophthalmologist: no telangiectasia, exudates, retinopathy, optic atrophy or any other pathological signs were detected. Neurological examination: the child is conscious, oriented, moderately increased muscle tone, brisk deep tendon reflexes, mild bilateral positive Gordon's sign, as well as mild stiffness of the neck muscles and positive Kernig's sign. Cerebellar symptoms are determined: dysmetria (impaired coordination of movements due to loss of the sense of distance, proportionality and accuracy of movements - author's note), intention tremor, ataxic gait.
History: tuberculous lymphadenitis at the age of 2 years, treatment with anti-tuberculosis drugs.
Complete blood count, ESR, renal and liver function tests, plasma calcium, phosphate, alkaline phosphatase, chest radiograph, and abdominal ultrasound were within normal limits.
Figure 1 |
General algorithm for differential diagnosis Serological tests did not confirm echinococcosis, toxoplasmosis, cysticercosis, cryptococcosis, cytomegalovirus and HIV infection.
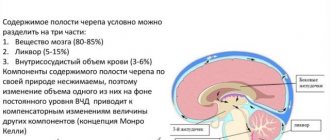
Computed tomography showed signs of a lacunar skull (groups of round, oval or finger-shaped depressions were identified on the inner surface of the cranial vault, separated by ribbed outgrowths of normal bone tissue in the thickest parts of the frontal, parietal and superior occipital bones - a characteristic sign of intrauterine increase in intracranial pressure or a disorder of bone formation - approx. .trans.), as well as extensive areas of intracranial calcifications, which extended bilaterally to the deep* cerebellar nuclei, the border of white and gray matter, thalamus, the region of the basal ganglia and capsules.
Figure 2
a: on the topogram, which is carried out to mark the scan, the lacunar skull and intracranial calcifications are clearly visible. b: Non-contrast enhanced CT scan showed bilateral calcifications in the dentate nucleus of the cerebellum; c: asymmetrical bilateral extensive calcification in the region of the basal ganglia and internal capsule, thalamus and d: borders of gray and white matter
MRI of the brain revealed large areas of hyperintense T2WI and FLAIR signal that affected the periventricular areas of the white matter, leaving intact U-fibers and the corpus callosum with cystic inclusions and signs of obstructive hydrocephalus. The calcifications previously detected on CT were hypointense in T2- and T1WI and showed a “loss” of the MR signal in GRE.
The clinical and radiological findings were classic for leukoencephalopathy with calcifications and cysts (LCC, also called Labrun syndrome - author's note), which was complicated by the development of obstructive hydrocephalus.
Figure 3
On axial T2WI (a, b) and FLAIR (c, d) tomograms, large areas of hyperintensity in the white matter of the brain can be seen, which indicates leukoencephalopathy.
Figure 4
Axial T1 and T2WI scans demonstrate cysts in both hemispheres of the cerebellum, located above the third ventricle in the pineal region; note dilatation of the lateral ventricles due to obstructive hydrocephalus.
The neurosurgical team recommended placement of a ventriculoperitoneal shunt, but the patient's relatives refused invasive procedures. The patient was prescribed treatment with valproic acid and acetazolamide, which provided a symptomatic effect.
Figure 5
The areas of “loss” of the MR signal on GRE in the region of the basal ganglia, thalamus and cerebellar nuclei correspond to calcifications.
A combination of extensive cerebral calcifications, cerebral white matter changes, and cysts has been described by Labrune et al. in 1996 under the name LCC. This is an extremely rare condition; only about 10 cases have been described in the literature; it occurs in children and adults; time of onset of symptoms up to 59 years. The classic clinical picture of progressive neurological deficit in a child for this pathology involves a huge list of differential diagnoses, but there are characteristic radiological signs that make it possible to make an almost unmistakable diagnosis.
In differential diagnosis, it is worth remembering such parasitic infections as echinococcosis, neurocysticercosis, cryptococcosis.
In neurocysticercosis there are multiple cystic inclusions with variable* punctate calcification; gelatinous pseudocysts and parenchymal calcifications have been described in HIV-infected patients with cryptococcosis, but the results of serological studies did not confirm these nosologies, especially since they are not characterized by manifestations of leukoencephalopathy (white matter lesions).
Our patient had increased intracranial pressure and cyst-related mass effect, which are the main manifestations of LCC.
Neuroimaging findings are closely related to pathogenesis. Typically, the disease manifests as bilateral asymmetric calcifications in the subcortical and cerebellar nuclei, diffuse white matter lesions, multiple cysts of varying sizes with signs of contrast accumulation in their walls, and, rarely, bleeding into the cysts or brain parenchyma. MR angiography is usually without abnormalities; a perfusion study detects hyperperfusion in the walls of the cysts, which, together with possible bleeding, suggests vascular disorders.
MR spectroscopy, which has been performed in some cases of LCC, did not detect lactate and showed decreased choline and NAA peaks in areas of affected white matter; these changes correspond to water content in areas of leukoencephalopathy, while high choline levels are expected from the demyelinating process. Perhaps swelling of the white matter of the brain is associated with disruption of the BBB. MR spectroscopy of the contents of the cysts did not reveal any typical metabolites for brain parenchyma. Histological examination revealed Rosenthal fibers (also found in Alexander disease) in most cases. These fibers are associated with mutations in the gene encoding glial fibrillary acidic protein. (GFAP) are cytoplasmic inclusions in astrocytes that contain the intermediate filament protein GFAP and small heat shock proteins. Accumulation of Rosenthal fibers may interfere with normal astrocyte function.
In addition to Rosenthal fibers, the most common findings are myelin pallor, angiomatous changes in cerebral vessels, microcalcifications, and hemosiderin deposits.
The etiology of the disease is currently unclear. In addition to mutations in the GFAP gene, mutations in the SNORD118 gene have also been reported to be associated with this nosology. A biopsy may be performed to definitively confirm the diagnosis, but in most cases this invasive procedure does more harm than good. Therefore, diagnostics and differential diagnosis rely to a greater extent on neuroimaging data, based on the data of which several similar genetically determined pathologies can be immediately eliminated.
Thus, Fahr's disease, Sturge-Weber syndrome and MELAS can cause intracranial calcifications, but without leukoencephalopathy and cysts. Cockayne syndrome presents with intracranial calcifications and diffuse leukoencephalopathy, but without cysts. Hippel-Lindau disease results in cerebellar cysts, but without calcifications or leukoencephalopathy. Alexander disease presents with leukoencephalopathy and cysts, but without calcification. Metachromatic leukodystrophy and adrenoleukodystrophy lead to diffuse damage to the white matter of the brain without cysts or calcification.
Only LCC, Coats Plus syndrome, Aicardi-Goutières syndrome, intracranial parasitic infection, and some astrocytomas may present with leukoencephalopathy, calcifications, and cysts. Coats Plus is a systemic disease associated with a mutation in the CTC1 gene. Intracranial parasitic infection should be considered after serological confirmation. Aicardi-Goutieres syndrome is associated with a TREX1 mutation. Astrocytomas suggest an increased choline peak on MR spectroscopy.
Figure 6
Axial CT scans (A, B) show bilateral calcifications in the thalamus and caudate nuclei, as well as multiple cysts in both hemispheres of the brain. T2WI tomogram (C) showed a diffuse pathological MR signal from the white matter with intact gray matter of the brain. Post-contrast MRI (D) showed that the cyst in the left frontal lobe exhibited heterogeneous ring-like contrast enhancement. MR spectroscopy (E): decreased NAA and choline peaks in areas of altered white matter. Perfusion MRI (F) showed hyperperfusion in the cyst wall. T2WI 5 months after the disease (G): the large cyst of the left frontal lobe has decreased, and the smaller cyst of the left frontal lobe, on the contrary, has increased.
Miao Wang et al. proposed the following diagnostic scheme for cases of combination of white matter lesions with intracerebral calcifications and cysts.
Sources:
- Pahuja, Leena, et al. "Labrune syndrome: A unique leukoencephalopathy." Annals of Indian Academy of Neurology20.1 (2017): 59.
- Pessoa, André Luiz Santos, et al. "Leukoencephalopathy with cerebral calcifications and cyst: Labrune syndrome." Arquivos de neuro-psiquiatria 70.3 (2012): 230-231.
- Karlinger, Kinga, et al. "Leukoencephalopathy, cerebral calcifications and cysts: a family study." Journal of neurology261.10 (2014): 1911-1916.
- Sener, U., et al. "Leukoencephalopathy, cerebral calcifications, and cysts." American journal of neuroradiology 27.1 (2006): 200-203.
- Wang, Miao, et al. "Leukoencephalopathy with cerebral calcification and cysts: cases report and literature review." Journal of the neurological sciences 370 (2016): 173-179.
- Jenkinson, Emma M., et al. "Mutations in SNORD118 cause the cerebral microangiopathy leukoencephalopathy with calcifications and cysts." Nature genetics 48.10 (2016): 1185.
Types of leukoencephalopathy
The least dangerous form is focal. Formed by chronic inflammatory processes of vascular origin. Lack of microcirculation in a certain part of the brain provokes hypoxia, a lack of oxygen. The death of white matter zones takes several years to develop.
Morphological changes occur more aggressively in hypertension. An increase in intracranial pressure causes ruptures of small capillaries with areas of necrosis of the brain parenchyma. A type of medical language is called “discircular encephalopathy.” Appears in people over 55 years of age.
Progressive multifocal leukoencephalopathy has an aggressive course. People with pathology live no more than 5 years. Lethal outcomes are associated with extensive heart attacks and strokes.
Classification of types of leukoencephalopathy according to ICD 10
A progressive type of vascular origin (Binswanger's disease) is coded with the symbols “I67.3”. Subcortical dementia with code “F01.2” has been excluded from the classification of diseases of the tenth revision.
Progressive multifocal (multifocal) leukoencephalopathy - “A81.2”. The group of the same name includes phenylketonuria, Alexander disease, and Canavan disease. Pathologies of category “IA” are distinguished for reasons, as they are of autoimmune origin - caused by tissue damage by immunoglobulins of the body’s own. Antibodies become aggressive when the structure of the membrane or the genetic information of the cell changes under the influence of viruses, chemical, and physical factors.
Let's look at the complete classification algorithm:
- Diseases of the circulatory system – “IX. 100-199";
- Cerebrovascular diseases “I60-69”;
- Other cerebrovascular diseases - “I67”;
- Progressive vascular leukoencephalopathy – “I67.3”;
- Other specified vascular lesions – “I67.8”.
The international classification of the tenth revision is valid. When encoding the diagnosis, discirculatory encephalopathy, acute cerebrovascular insufficiency, NOS, and cerebral ischemia (chronic) are often encountered.
Clinical symptoms of small focal leukoencephalopathy
Focal symptoms have a subacute course. The initial stages of the disease are identified by neurologists:
- Visual impairment, speech impairment;
- Pathology of the innervation of the muscles of one half of the body;
- Epilepsy attacks;
- Headaches, dizziness;
- Ataxia, anopsia.
Differential diagnosis of focal types is carried out to distinguish them from changes in white matter in HIV and dementia. Spinal lesions occur without impairment of mental functions. Damage to white matter is accompanied by cognitive impairment.
Progressive multifocal leukoencephalopathy
The cause of multifocal white matter damage is the JC virus, which leads to widespread damage to the nervous system. The disease develops against a background of reduced activity of the immune system. Antiretroviral treatment is expensive, so most people die.
Progressive encephalopathy quickly leads to the destruction of the myelin of most nerve cells. The changes are irreversible, the symptoms gradually increase.
About 80% of the country's population are carriers of human polyomavirus type 2, but encephalopathy does not occur. Only immunodeficiencies in AIDS create the possibility of rapid reproduction of the pathogen.
The immunity of older people cannot cope with the activity of polyomavirus (JC) after immunomodulatory or immunosuppressive therapy after treatment of cancer or organ transplant surgery.
In children, the appearance of pathology is observed after the start of therapy for chronic lymphocytic leukemia and Hodgkin's disease.
The 1C virus is transmitted by airborne droplets or fecal-oral routes. The majority of the population is asymptomatic. Provoking factors:
- HIV infection;
- Taking immunosuppressants;
- Lymphogranulomatosis;
- Leukemia.
Magnetic resonance imaging is the only way to identify pathological foci within the white matter. After the appearance of visual impairment, dysarthria, hemiparesis, and aphasia, neurologists will be able to suggest a diagnosis. Final verification is possible only after a microscopic examination of brain biopsies - tissue sections taken from the site of injury.
Clinical picture
Typically, the symptoms of leukoencephalopathy develop gradually. At the beginning of the disease, the patient may be distracted, awkward, and indifferent to what is happening. The patient becomes tearful, has difficulty pronouncing difficult words, and his mental performance decreases.
Over time, sleep problems may occur, muscle tone increases, the patient becomes irritable, involuntary eye movements and tinnitus may occur.
If treatment for leukoencephalopathy is not started at this stage, it progresses: psychoneuroses, severe dementia and convulsions appear.
The main symptoms of the disease are the following deviations from the norm:
- Movement disorders are manifested by impaired coordination of movements, weakness in the arms and legs;
- unilateral paralysis of the arms or legs may occur;
- Speech and vision disorders (scotoma, hemianopsia);
- numbness in various parts of the body;
- swallowing disorder;
- urinary incontinence;
- Epileptic seizures;
- intellectual impairment and mild dementia;
- nausea;
- headache.
All symptoms of damage to the nervous system progress very quickly. The patient may have false wrist paralysis and parkinsonian syndrome, which is characterized by abnormal gait, writing, and body tremors.
Almost every patient experiences memory and intelligence impairment, instability when changing body position or walking.
People usually do not realize that they are sick, so they are often brought to the doctor by relatives.
Discircular encephalopathy
The chronic progressive course of cerebrovascular pathology is accompanied by diffuse multifocal changes leading to hemiparesis, ischemic stroke, and multiple neuropsychological and neurological disorders.
The progression of dyscirculatory encephalopathy is associated with tissue degeneration and the accumulation of aggressive metabolites.
Before using neuroimaging methods, experts attributed most of the causes of cognitive disorders to dyscirculatory encephalopathy. Practice shows overdiagnosis of nosology cases. Nuclear magnetic resonance indicates only a 20% incidence of white matter lesions in elderly patients with vascular disease.
The main difference between the discircular type and a stroke is that it affects not large cerebral arteries, but small penetrating vessels, arterioles. Diffuse damage to small branches causes a number of morphological changes:
- Numerous heart attacks (lacunar);
- Diffuse destruction of white matter;
- Mixed form.
Early detection of any category prevents progression after proper supportive care is given.
Features of periventricular and residual leukoencephalopathy in children
Chronic lack of oxygen supply and prolonged ischemia of brain tissue leads to damage to subcortical structures, hemispheres, and the brain stem. Pathological foci are found deep in the gray matter and are accompanied by changes in subcortical fibers.
Periventricular encephalopathy is characterized by the predominant localization of pathological foci around the ventricles of the brain.
The residual appearance has congenital and acquired causes. The provoking factor in a child is traumatic injuries to the skull, inflammatory processes inside the skull. A separate type, encephalomyelopathy, occurs due to abnormalities in the structure of the vascular network of the brain.
Symptoms of residual encephalopathy in children:
- Cerebral paralysis;
- Oligophrenia;
- Epilepsy;
- Vegetative-vascular dystonia;
- Restless sleep.
Practice shows the presence of a latent course of nosology in newborns weighing about four kilograms. Clinical symptoms appear after the onset of active blood supply. Cases of dementia in preschoolers and schoolchildren are associated with injuries to the skull.
How long do people live with encephalopathy?
Life expectancy is determined by the clinical form of the disease, the rate of progression, and individual changes in the human body.
Progressive multifocal encephalopathy is accompanied by death 1-3 years after detection. Maintenance therapy increases survival.
Varieties of vascular origin have chronic progression. People with this variety, with proper treatment, live for decades. Reduces the duration of hypertension, pronounced ischemic foci of the brain structure, hemorrhages inside the brain.
Prevention
There is no specific prevention of leukoencephalopathy.
To reduce the risk of developing this pathology, the following rules should be followed:
- Strengthen your immune system by hardening yourself and taking vitamin and mineral complexes;
- normalize your weight;
- to live an active lifestyle;
- regularly go out into fresh air;
- give up drugs and alcohol;
- quit smoking;
- Avoid casual sex;
- Use a condom for casual sex;
- Follow a balanced diet, which should be dominated by fruits and vegetables;
- Learn to cope with stress;
- and get enough rest;
- Avoid excessive physical activity;
- For diabetes, atherosclerosis and hypertension, you should take medications prescribed by your doctor to compensate for the disease.
All these actions minimize the risk of developing leukoencephalopathy. If you become ill, you should seek medical attention as soon as possible and begin treatment that will help prolong your life.