Clinic experts:
- Zotov Alexander from the Federal Scientific and Clinical Center of FMBA
- Vasiliev Vladislav from the National Medical Research Center of Cardiology
- Amir Kramer from TASMC
- Dmitry Pevny from TASMC
For severe angina, atherosclerosis, and coronary heart disease, the best solution is CABG (coronary artery bypass grafting) surgery.
It is this procedure that not only saves a person’s life, but also significantly improves its quality. The Medis Clinic offers patients who have appropriate indications to undergo heart bypass surgery in Moscow or Israel with the most experienced and competent cardiac surgeons who have the most modern techniques for heart interventions, in premium hospitals. We also offer aortic or mitral valve replacement or surgery, as well as aortic root replacement. The cost of CABG and hospitalization is 300 thousand rubles, performed by a leading cardiac surgeon in the leading cardiac surgery center in the country. We approach the selection of doctors very carefully and cooperate only with conscientious, honest doctors who have extensive practical experience and have worked in various large clinics not only in Russia, but also abroad. International experience, the ability to perform the most modern procedures in high-tech and patient-safe ways, following medical protocols currently accepted in the world, as well as placing human health and well-being at the forefront - these are what we and our patients value in doctors.
About CABG surgery
Coronary artery bypass grafting (CABG) is one of the most effective methods in the treatment of coronary heart disease (CHD).
The operation is performed on a beating heart, without the use of artificial circulation, and is indicated in cases where damage to the arteries of the heart is so severe that the use of other methods of restoring coronary blood flow is impossible. In our clinic of the Federal Scientific and Clinical Center of Federal Medical and Biological Agency, coronary bypass surgery is performed using several methods:
- on a “working” heart without the use of artificial circulation;
- on a beating heart under conditions of assisted artificial circulation.
Risks and complications
- postoperative bleeding;
- inflammatory process of a postoperative wound;
- respiratory complications;
- heart rhythm disturbances;
- pain associated with nerve fibers, muscle spasm or dislocation of costal cartilage;
- encephalopathy;
- cardiac weakness, perioperative myocardial damage, stroke, death.
Anyone can calculate the risk of surgery using the international table for calculating the risk of cardiac surgery EuroSCORE II, which takes a few minutes.
Indications for coronary artery bypass grafting
Indications for CABG are determined by varying degrees of arterial damage and manifestations of coronary heart disease:
As a rule, CABG is not performed:
- severe multiple organ failure;
- during the first months after cerebrovascular accident;
- malignant neoplasms.
Therapeutic measures
Medicines are used for the following purposes:
- normalization of pulse and blood pressure;
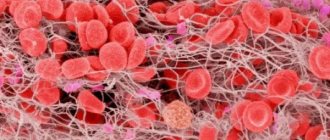
- preventing the formation of blood clots;
- reducing the amount of cholesterol in the blood;
- normalization of conductivity and nutrition of the heart muscle.
The list of main medications is presented:
- Atorvastatin;
- Bisoprolol;
- Brilinta;
- Lisinopril;
- Plavix;
- Preductal;
- ThromboASSom.
You can purchase medications at a pharmacy or buy them in an online store. It’s easier to buy medicines on virtual platforms; promotions are held there more often, and there is a system of discounts. Websites allow you to receive products from a warehouse or reserve them in stores.
Preparation for coronary artery bypass surgery
At the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, before performing coronary artery bypass surgery, the doctor draws up a preoperative examination plan. It includes laboratory tests and instrumental studies:
- general blood test, urine test;
- blood biochemistry;
- expanded coagulogram;
- ADP platelet aggregation;
- blood type and Rh factor;
- markers of infections: HIV, hepatitis B, hepatitis C, syphilis;
- Pro-BNP, SRP;
- ECG;
- Echo-CG;
- X-ray examination;
- EGDS (maximum duration – 1 month). An exception is patients with lesions of the left artery trunk;
- Ultrasound scanning of the brachiocephalic arteries (maximum duration – 3 months);
- Ultrasound scanning of the arteries of the lower extremities (maximum duration – 3 months);
- Ultrasound scanning of the veins of the lower extremities (maximum duration – 7 days);
- FVD (maximum duration – 7 days);
- Ultrasound of internal organs;
- coronary angiography.
If there is a concomitant pathology, additional tests may be prescribed:
- History of stroke - CT scan of the brain.
- thyroid diseases - TSH, T4, T3 (maximum duration - 30 days). Consult an endocrinologist if there are changes in the hormonal profile.
- diabetes mellitus - glycemic curve (maximum duration - 7 days). Consultation with an endocrinologist for glycemia more than 10 mmol/l.
- Gout - uric acid (maximum duration - 1 month). If the value exceeds 420 µmol/l, consult a therapist and select therapy.
- consultation with a dentist, urologist, gynecologist.
The day before surgery, the patient is examined by a surgeon and an anesthesiologist. On the eve of CABG, it is recommended to have a light dinner no later than 12 hours before surgery, not to eat or drink the night before, and to stop taking medications. A cleansing enema is given at night. In the morning the patient takes a shower.
After signing the informed consent, the patient is given premedication - medications are administered that will reduce emotional tension and help calm down. After 40-60 minutes, the patient is taken to the operating room.
At the cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, you can take all the tests and undergo studies recommended by your doctor before the operation. The structure of our center allows you to quickly go through the preparatory preoperative stage and get the results in hand. Having our own laboratory, we are responsible for the accuracy of tests and the quality of clinical and laboratory studies.
Coronary artery bypass grafting (CABG) occupies an important place in the complex of modern methods of treating patients with coronary heart disease (CHD). In most clinics, this operation is still performed under conditions of artificial circulation (CPB) and cardioplegia. Less commonly, CABG is performed without IR on a beating heart using OPCAB (off-pump coronary artery bypass) technology. The advantages of OPCAB over traditional CABG with CPB have been proven in patients with multifocal atherosclerosis, chronic obstructive pulmonary disease, chronic kidney disease and other severe concomitant diseases [3, 7, 28, 57]. At the same time, in their absence in low-risk patients, abandoning CPB does not lead to a significant improvement in CABG results [3, 8]. Moreover, in patients with disabled myocardium, significant dilatation and low pumping function of the left ventricle, the use of OPCAB technology is associated with an increased risk of severe hemodynamic disorders during cardiac dislocation. The optimal tactical solution in such patients can be considered CABG with CPB in the auxiliary mode without cardioplegia, which eliminates the indicated disturbances of central hemodynamics and possible complications associated with myocardial anoxia [14, 61, 65].
In a number of clinics, most CABG operations are performed without IR [64, 66]. However, it should be noted that a reserved attitude towards them remains, and the global share of such interventions among all CABG operations does not exceed 20% [33]. In our opinion, there are several reasons for this. First, there is no proven benefit of OPCAB in the above-mentioned, fairly large group of low-risk patients without severe comorbidities. Secondly, excellent results of traditional CABG with PC do not always contribute to motivation for introducing new technologies into practice [15, 72]. Thirdly, even extensive and successful experience in performing CABG under conditions of bypass and cardioplegia does not guarantee success in mastering the OPCAB technology, which also negatively affects the attitude of many cardiac surgeons to this operation [31]. In this regard, it is necessary to mention the large randomized multicenter studies ROOBY and DOORS, in which the authors showed significantly worse patency of autovenous bypass grafts after OPCAB operations in comparison with traditional CABG with the same patency of mammary-coronary anastomoses and the absence of significant differences in the incidence of adverse cardiac and cerebrovascular events in within a year after surgery [20, 73]. However, their opponents quite reasonably noted a significant drawback of these studies, which consisted in the little experience of OPCAB operations among many surgeons, which resulted in a high rate of conversion to IR (12.4%), which could not but negatively affect the presented results [33]. On the contrary, the experience of regularly performing a large number of operations without IR, when their share exceeds 60% of all CABG operations, is translated into high quality of formed anastomoses, which has a positive effect on the results obtained. The authors of such publications [50], in particular, the large randomized study JOCRI (Japanese Off-Pump Coronary Investigation), did not find significant differences in the patency of autovenous, radial and mammary coronary bypass grafts, or in the clinical condition of patients within 2 years after CABG with and without bypass. This is also confirmed by J. Puskas et al. [67], who in a randomized study did not find a significant difference between OPCAB and CABG with CPB in the patency of shunts and the incidence of adverse cardiac and cerebrovascular events both in the immediate term and 8 years after surgery.
It is clear that OPCAB can be considered as the procedure of choice for high-risk patients in the hands of experienced surgeons who perform it regularly and efficiently. Under this condition, refusal from bypass does not affect the patency of the shunts in the postoperative period, and the long-term results of OPCAB are in no way inferior to those after traditional CABG with bypass. This approach allows us to significantly expand the capabilities of OPCAB technology and use it in the majority of operated patients if the surgeon prefers to perform myocardial revascularization without IR.
The most important trend in modern cardiac surgery is the desire for minimal surgical trauma and the fastest possible rehabilitation of the patient, which is largely facilitated by the introduction of new, increasingly advanced minimally invasive surgical technologies into the clinic [2, 5, 17]. In accordance with the decisions of the First World Congress on Minimally Invasive Cardiac Surgery, the main goal of minimally invasive myocardial revascularization is to reduce the number of complications and accelerate the patient’s recovery, while maintaining the effectiveness and duration of the therapeutic effect of the operation [12]. One of the main principles of such an operation is to minimize the area of intervention. The use of mini-approaches in cardiac surgery is very important, given the traumatic nature of sternotomy and the specific complications associated with it [17]. Even in the absence of the latter, many patients report a decrease in quality of life for several months after surgery due to some discomfort in the sternotomy area [69]. However, it is not entirely correct to consider only the small size of the surgical approach as a determining factor that reduces surgical trauma. A number of cardiac surgeons consider an equally important criterion for “minimal invasiveness” to be the exclusion of I.K. from the means of supporting the operation. In their opinion, avoiding CPB and cardioplegia reduces the risk of intervention to a greater extent than reducing the size of the surgical approach [1].
OPCAB is a non-CPB operation through a traditional, longitudinal sternotomy. Can it be considered minimally invasive? Apparently not, since this operation does not fully meet all of the above criteria. According to A. Calafiore [29], the term “minimally invasive myocardial revascularization” should be understood only those coronary bypass operations that are performed without sternotomy and I.K. If we are guided by this definition, that is, there is every reason to consider V.I. to be the pioneer of this direction in coronary surgery. Kolesov, who in 1964 was the first to perform mammary-coronary anastomosis through a left-sided thoracotomy [9, 51]. In 1971, his son E.V. Kolesov [10] summarized and presented the results of 271 such operations. Abroad, coronary bypass surgery using the internal mammary artery (IMA) without bypass through a left-sided thoracotomy has become most widespread in Argentina, where F. Benetti [21] was distinguished by high surgical activity, who in 1991 reported the results of 700 such operations. Modern minimally invasive coronary surgery began in 1994, when F. Benetti et al. [20], as well as V. Subramanian et al. [76] almost simultaneously presented the results of mammary coronary bypass surgery without IR through an anterior left mini-thoracotomy. After 2 years, excellent results of such an operation in 115 patients with a hospital mortality rate of 0.6% were demonstrated by a group of Italian cardiac surgeons led by A. Calafiore [68]. By this time, certain progress had been made in technical support for myocardial revascularization on a beating heart; the first mechanical systems for local myocardial stabilization appeared, which provided a stationary field at the site of coronary anastomosis [29]. In 1996, the operation was given the name MIDCAB (Minimally Invasive Direct Coronary Artery Bypass), under which it exists to this day. In Russia it became widespread in 1997-1998. The pioneers and active initiators of the introduction of MIDCAB into the clinic were Yu.V. Belov and G.P. Vlasov [1, 2]. Another solution that seemed innovative was thoracoscopic exposure of the left ITA (LVHA). This procedure eliminated excessive traction of the ribs during direct exposure of the LVGA using imperfect and traumatic retractors of that time. The use of video support for MIDCAB was first reported by F. Benetti et al. in 1994, and in Russia - G.M. Soloviev et al. in 1997 [13, 22].
Despite the undoubted compliance with the above principles of minimally invasive myocardial revascularization, MIDCAB was not without very significant drawbacks. First, the scope of revascularization was limited to one anterior descending artery (LAD), and occasionally two coronary arteries, including its diagonal branch (DB). Because of this, indications for MIDCAB arose when it was necessary to intervene only on the LAD. Very soon, the high level of X-ray endovascular surgery achieved allowed the majority of patients with such lesions to effectively perform coronary angioplasty with implantation of drug-eluting intracoronary stents. Therefore, currently the indications for MIDCAB are limited to situations where, for some reason, coronary angioplasty cannot be performed. Secondly, mini-thoracotomy does not allow immediate connection of IC in cases of emergency conversion. If this disadvantage of MIDCAB can be eliminated due to the experience of using peripheral IR, then the first one has become the main reason for a significant decrease in interest in this operation. In subsequent years, the aforementioned OPCAB technology became incomparably more widespread. The introduction into surgical practice of vacuum positioning systems and local stabilization of the myocardium expanded the capabilities of this technology and made it possible to perform multiple CABG operations without IR in patients with multivessel coronary lesions and stenosis of the left coronary artery, which together make up the vast majority of operated patients with coronary artery disease [11, 16, 42, 67]. However, with all its advantages, OPCAV cannot be considered a minimally invasive intervention. All sorts of problems associated with a full sternotomy remain. This is no different from traditional CABG in the setting of cardiopulmonary bypass [52, 78]. This circumstance was of great importance in maintaining the motivation of cardiac surgeons to search for new technologies that, unlike OPCAB, could fully meet the definition of “minimally invasive myocardial revascularization” and, unlike MIDCAB, could be used in the majority of operated patients with varying volumes of lesions coronary bed.
Now we can state that the further development of minimally invasive myocardial revascularization is proceeding in several directions. The first and most common is hybrid myocardial revascularization (HCR, Hybrid Coronary Revascularization), which combines the advantages of MIDCAB and percutaneous coronary intervention. HCR was initially considered as a treatment modality that could provide adequate myocardial revascularization in high-risk patients. Acceptable results contributed to its further introduction into the clinic, and now HCR is included in most modern recommendations for the treatment of patients with coronary artery disease [45, 80]. In particular, this technology is indicated for use in cases of severe atherocalcinosis of the ascending aorta, “poor” condition of the target coronary arteries, conduit deficiency, and LAD lesions unfavorable for stenting with a low SYNTAX score.
There are 3 options for performing HCR, each of which has its own advantages and disadvantages. The first intervention option is possible in the presence of a hybrid operating room, in which MIDCAB is first performed and then immediately intracoronary stenting. The positive aspects of this option are the initial restoration of blood flow in the LAD and subsequent angiographic quality control of the mammary-coronary anastomosis; the negative aspects are the high risk of bleeding due to the need to begin disaggregant therapy immediately after neutralization of heparin, as well as the risk of developing contrast-induced nephropathy due to surgical stress. All of the above requires coordinated, highly professional work of cardiac surgeons, anesthesiologists and interventional cardiologists. The second option is intracoronary stenting delayed for several days after MIDCAB, which does not require a hybrid operating room. Previously restored blood flow in the LAD allows in such situations to safely perform angioplasty for lesions of the trunk of the left coronary artery (LCA) and ostial lesions of the circumflex artery (CA), and there is the possibility of angiographic quality control of the mammary-coronary anastomosis. There is no high risk of bleeding, but the patient undergoes two interventions, and while waiting for angioplasty there is a risk of developing ischemia of non-revascularized myocardium. The third option, a hybrid intervention with initial coronary angioplasty and delayed MIDCAB, is rarely performed, mainly in cases of acute coronary syndrome and the need for intracoronary stenting of the infarct-related OA or right coronary artery (RCA). A hybrid operating room is not required in these situations. In addition, there is a risk of thrombosis of previously implanted stents if antiplatelet therapy and heparin neutralization are temporarily interrupted after MIDCAB [70].
In general, a number of researchers [43, 44, 81] indicate certain advantages of HCR over multiple coronary artery bypass grafting in a certain, carefully selected group of high-risk patients with a low SYNTAX score. At the hospital stage of treatment, these advantages include a reduction in the duration of artificial pulmonary ventilation (ALV) and time in the cardiac intensive care unit, a reduction in the need for blood component transfusions and a reduction in hospitalization time. However, there are no longer differences in hospital mortality rates and the incidence of adverse cardiovascular events in the 1st year after HCR. In the future, the need for repeated myocardial revascularization is significantly higher after hybrid intervention.
The most high-tech method of minimally invasive myocardial revascularization is robot-assisted, fully endoscopic coronary artery bypass grafting (TECAB - Total Endoscopic Coronary Artery Bypass). Over the 20 years of its development since the experimental work of E. Stephenson and C. Ducko, the world's first TECAB operation, successfully performed by D. Loulmet in a Paris clinic in 1998, coronary robotic surgery has achieved impressive progress [37, 56, 75]. Currently, it is concentrated in a number of cardiac surgery centers in the USA, Canada, Germany and Southeast Asian countries. Initially, the use of the Zeus robotic systems, and then the first generations of da Vinci, was limited to the isolation of the IAV and the formation of a mammary-coronary anastomosis between the LVHA and the LAD. Surgical access to other target coronary arteries was achieved through a longitudinal sternotomy and, much less frequently, through a left anterior mini-thoracotomy [32, 34–36]. In 2000, U. Kappert et al. [48] from Dresden first reported a successful fully endoscopic bilateral mammary coronary artery bypass graft surgery, in which the LVGA was used for the obtuse edge branch of the OA and the right ITA for the LAD. It is quite natural that at the initial stage of its development, robot-assisted coronary bypass surgery was often accompanied by intraoperative complications, the frequency of which reached 50%. The problems concerned both the isolation of the IAV and the formation of distal anastomoses. Such complications often entailed conversion to conventional CABG and were accompanied by an increase in operative time, mechanical ventilation, and patient stay in the cardiac intensive care unit and hospital, but, fortunately, did not lead to an increase in hospital mortality [25]. As experience has gained, there has been a clear trend toward a significant reduction in complication rates, and TECAB itself has become increasingly competitive with traditional CABG. The advantages of TECAB included shorter hospital stay, faster physical rehabilitation, and less pain in the first months after surgery [23]. S. Savista et al. [74] in 2010 presented the results of TECAB of 1, 2 and 3 coronary arteries performed in 2004–2007. In addition to excellent short-term and long-term results, the authors reported excellent graft patency of 98.6%.
Modern TECAB is a multiple bimammary coronary bypass surgery performed with complete preservation of the integrity of the chest without any surgical access. The volume of myocardial revascularization is from 1 to 4 coronary arteries [24]. With a intact chest length of two IAVs in situ
usually sufficient to create the required number of coronary anastomoses. HAV is isolated in a skeletonized manner [27]. In most patients, operations are performed under peripheral bypass with transfemoral cannulation. Cardioplegia is performed through an endoaortic balloon catheter, which is inserted through a side branch of the arterial line. Under the control of transesophageal echocardiography, the catheter is inserted into the ascending aorta, the balloon is inflated, the aorta is completely obstructed, and, as a rule, blood cardioplegia is performed [53]. No less common is TECAB on the beating heart under conditions of parallel cardiopulmonary bypass, which is advisable to use in patients with low functional reserves of the myocardium [53, 74]. Operations without IR are performed relatively rarely, due to the high risk of central hemodynamic disorders when the heart is dislocated inside a closed chest cavity. Until recently, the exception was isolated mammary coronary artery bypass grafting of the LAD [38, 39]. However, currently there is a tendency towards an increase in the number of robot-assisted multiple coronary artery bypass grafting operations without IR [19, 79]. It should be noted that TECAB can be either an independent method of surgical treatment or a component of HCR, thereby enhancing its minimally invasive nature [26, 40, 74].
Despite all the obvious advantages, TECAB technology has not yet found wide application in cardiac surgery practice, primarily due to its high cost. Many clinics, for financial reasons, cannot afford to purchase and operate modern robotic systems. In addition, the long learning curve of TECAB suggests a more complex and time-consuming process to achieve the required proficiency compared with other myocardial revascularization techniques [53]. Therefore, this technology, despite the gradual expansion of its geography, still remains the prerogative of a small number of specialized and high-budget centers [19, 27, 39].
The above-mentioned disadvantages are largely devoid of another direction of minimally invasive myocardial revascularization, focused on performing multiple coronary artery bypass grafting through a left anterolateral mini-thoracotomy (MICS CABG - Minimally Invasive Cardiac Surgery/Coronary Artery Bypass Grafting). The first such operation without IR was performed by J. McGinn et al. [59] in January 2005 in New York at the Heart Institute. By 2014, more than 1,000 surgical interventions were performed here using this technology. The operation has become widespread in a number of clinics in the USA and Canada, Europe, Japan, India and China [4, 41, 49, 54, 58, 61]. In Russia, MICS CABG is performed in cardiac surgery clinics in Astrakhan, St. Petersburg and Moscow [6, 7, 17].
All stages of the operation are performed by the surgeon under direct vision control without video assistance. There is no need for an expensive robotic system and consumables. MICS CABG technology differs from MIDCAB in its ability to perform multiple bypass grafting in patients with multivessel coronary artery disease. In this respect, the operation is similar to traditional CABG through a median sternotomy [70]. However, in contrast to it, MICS CABG is accompanied by minimal surgical trauma and complete preservation of the chest frame, rapid rehabilitation and excellent cosmetic effect. Due to this, the time of patients’ stay in the intensive care unit and the duration of hospitalization after surgery are reduced (on average 4 days), the risk of sternal infection and the need to interrupt even double antiplatelet therapy are completely eliminated [71]. Complete myocardial revascularization can be performed in 95% of patients operated on using this technology. Perioperative mortality does not exceed 1.3%. In addition, there is no doubt about the reduction in the need for blood transfusion, as well as the early return of patients to full physical and social activity [58]. Summarizing 10 years of experience with MICS CABG, J. McGinn et al. [59] praised its clinical effectiveness. Up to 8 years after surgery (on average 2.9±2.0 years), the survival rate was 96%, the rate of adverse cardiac and cerebrovascular events was 2%, the need for repeated myocardial revascularization was 7%, while the rate of re-interventions on previously bypassed coronary arteries was 1%. Such a significant clinical result of the operation, which is not inferior to traditional CABG, is explained by the high functional viability of the shunts after MICS CABG. Their overall patency six months after surgery is 92%, with absolute (100%) patency of IMA shunts [58, 71]. High-quality performance of anastomoses is an indispensable condition for achieving such indicators. In addition to the necessary experience and surgical skill, the full implementation of this condition depends on the exposure and visualization of the target coronary arteries. In this regard, it should be noted that mini-thoracotomy is usually performed more laterally compared to the MIDCAB procedure. This approach allows the ribs to be spread wider with less risk of damage and provides optimal exposure of not only the LAD, but also the branches of the OA and RCA [70]. Isolation of both IAVs, as well as the formation of proximal anastomoses on the ascending aorta, is significantly facilitated by one-lung mechanical ventilation of the right lung - a mandatory element of anesthesia for MICS CABG [4, 59]. The two HAVs can then be used both in situ
, and in composite structures for multiple bimammary coronary artery bypass grafting, excluding manipulation of the aorta. In addition, some surgeons offer thoracoscopic exposure of the ITA, which reduces the size of the mini-thoracotomy and eliminates excessive traction of the intercostal space, which is possible when mobilizing the ITA under direct visual control [46].
In accordance with one of the fundamental principles of minimally invasive cardiac surgery, the MICS CABG procedure is usually performed without I.C. However, sometimes with a large volume of revascularization and a reduced left ventricular ejection fraction, the use of IR in an auxiliary mode is justified, for which its peripheral connection is used through cannulation of the femoral vessels [70]. This technique is optimal for calm work with complex patients, which is extremely important for acquiring the necessary experience in such operations. In addition, the operation can be performed under conditions of full bypass and cardioplegia. The cardioplegic solution is supplied through a catheter integrated into the arterial line of the IR circuit; a balloon is fixed on it, the inflation of which leads to obstruction of the ascending aorta. Clamping of the aorta can also be done externally using a clamp connected to it through an additional port, with infusion of a cardioplegic solution into the ascending aorta.
Despite all the undoubted advantages, the MICS CABG technology still has certain limitations. However, only some of them can be considered contraindications to its use. Most of the others, as a rule, are due to insufficient experience of such operations and can be leveled out as it accumulates. The first should include low tolerance to one-lung ventilation, which, as a rule, occurs in severe chronic obstructive pulmonary disease [46]. The degree of its severity can be judged by the Tiffno index - the ratio of forced expiratory volume in 1 s (FEV1) to forced vital capacity (FVC). Its decrease to less than 0.5 indicates severe bronchial obstruction and an extremely high risk of one-lung ventilation. MICS CABG is not indicated for patients who have previously undergone surgery with left pleural cavity invasion. In addition, the operation is contraindicated in case of significant atherosclerotic damage to the arteries of the lower extremities, which excludes the possibility of safely connecting a peripheral I.C. Great care should be taken when using this technology in patients with disabled myocardium and cardiomegaly, when the risk of hemodynamic disturbances increases significantly when positioning the heart. For such patients, it is safer to perform the operation under conditions of parallel bypass with its transfemoral or central connection, in the latter case abandoning the mini-access in favor of traditional sternotomy.
At the stage of mastering MICS CABG, certain limitations may be associated with its technical performance in certain groups of patients. Possible difficulties in exposing the surgical field through mini-thoracotomy in overweight patients dictate the need to accumulate initial experience of this operation in normosthenic patients with wide intercostal spaces. The anatomical conditions in such cases are close to ideal and provide optimal visualization of the target coronary arteries. Objective difficulties in forming distal anastomoses in diffuse lesions of the coronary arteries and the often emerging need for endarterectomy with traditional CABG can become a serious obstacle to achieving the success of the first MICS CABG operations. In contrast, a multivessel but local lesion with sufficient diameter of the target coronary arteries and good condition of their distal bed will undoubtedly contribute to this success. However, the above difficulties cannot be considered contraindications to MICS CABG, because with sufficient experience and high qualifications of the surgeon, they do not interfere with the performance of these operations.
Thus, the modern trend towards minimizing surgical trauma has been developed in surgery for coronary heart disease in several directions at once. The possibility of performing hybrid myocardial revascularization (HCR) should primarily be considered in cases of high risk of multiple coronary artery bypass grafting, conduit deficiency, LAD lesions unfavorable for stenting with a low SYNTAX score, severe atherocalcinosis of the ascending aorta without the chance of using the “no-touch aorta” surgical technique. Robot-assisted fully endoscopic coronary artery bypass grafting (TECAB) allows complete myocardial revascularization without any access at all, minimizing surgical trauma to the patient. There is no doubt that the most advanced TECAB technologies ensure maximum implementation of the surgeon’s professional skill in achieving the desired surgical result with minimal trauma to the patient. However, the high cost, long and rather complex training period are factors that still hinder the introduction of this technology into wide cardiac surgical practice. Unlike TECAB, the MICS CABG operation does not involve such significant material costs, the learning curve indicates its high reproducibility. Typically, experience with OPCAB operations allows for rapid mastery of the technology [70]. As experience in its use accumulates, its indications can be significantly expanded. Because of this, in the near future, the MICS CABG operation can be considered as one of the main methods of minimally invasive myocardial revascularization.
The authors declare no conflict of interest.
The authors declare no conflict of interest.
Information about authors
Zhbanov I.V. — email
Kiladze I.Z. - https://orcid.org/0000-0002-3342-2440; e-mail
Uryuzhnikov V.V. - https://orcid.org/0000-0002-5187-8169; e-mail
Shabalkin B.V. — email
Corresponding author:
Kiladze I.Z. — e-mail: [email protected]
HOW TO QUOTE:
Zhbanov I.V., Kiladze I.Z., Uryuzhnikov V.V., Shabalkin B.V. Minimally invasive coronary surgery. Cardiology and cardiovascular surgery
. 2019;12(5):377-385. https://doi.org/10.17116/kardio201912051
Carrying out CABG
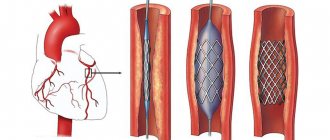
Coronary artery bypass surgery on a beating heart begins with providing access to the operation site - the skin, subcutaneous layers, and muscles are cut layer by layer.
A graft (shunt) - a healthy section of a vein or artery - is taken from the patient's chest or limb (thigh, lower leg). To perform surgery on a beating heart, special equipment is used to stabilize the myocardium at the site of the anastomosis. One end of the healthy vessel is sutured to the aorta, the other to the coronary artery below the stenotic/narrowed area. Then full heart function is restored, the wound is sutured, and the patient is transferred to the intensive care unit.
Coronary bypass surgery in most clinics is performed with cardiac arrest using a heart-lung machine. The use of this method is associated with the risk of complications that prolong recovery time, worsen recovery, and can lead to bleeding, stroke, and heart attack. Carrying out surgery without artificial circulation - on a beating heart - reduces the risk of postoperative complications.
Patient reviews
Georgy Ts.: As they say, if aortic bypass surgery is performed perfectly, then you should forget about it, but if it’s mediocre, then you’ll live for three to five years and good luck. So I decided to do it perfectly, I found out from my specialist who was worth what and decided to order everything to be done by the Medis clinic. I will not say anything about choosing a doctor, but I chose from the best, a famous heart surgeon flew to Moscow for the operation, and his team was local, but from the best. And as they explained to me at Medis, nursing also means a lot for recovery, so they provided it at the level. Everything went well, material for a shunt was taken from my leg, since the veins in my leg are good. Israeli surgeon Amir Kramer performed surgery on me when my heart stopped. An Israeli doctor took care of me and controlled everything. This is, of course, a “special order”, that is, a product specially built for me, this is me as a gene. I'm talking to the director. This is how you can ensure the highest level of CABG performance.
Samvel Karapetyan: I asked to organize a coronary artery bypass surgery with Medis and for three hundred thousand everything was done very well, quickly and efficiently.
After operation
In general, rehabilitation and recovery after CABG without artificial circulation is faster and easier. If the early postoperative period passes without complications, then after a day the catheters are removed and the patient is transferred to the department, where he remains for up to 7-10 days. There the condition of the heart and the whole body will be monitored.
In the postoperative period, a rehabilitation plan is individually selected for the patient and physical therapy is prescribed.
A good method of maintaining health is walking for 10 minutes at the very beginning (after you are allowed to walk) to 30-60 minutes 2-3 weeks after surgery.
It is important that during physical activity, the heart rate does not rise above 100-115 beats per minute and there is no shortness of breath.
If, after the operation and the rehabilitation period in the ward - in the cardiac surgery department, you are worried about independent recovery, you can undergo a rehabilitation program at our center.
Upon discharge from the hospital, the attending physician will issue a reminder about the rules of prevention after surgery and prescribe medications. Taking any other medications, including those from your home medicine cabinet, should be agreed with a cardiologist.
Smoking and drinking alcohol after CABG surgery are prohibited for life. You will also need to follow a diet with a reduced content of salt, fats, and sweets.
Afterwards, you will need to undergo a heart study at 1 month, 3, 6, 12 months. You can also do this in our center.
Doctors who operate on patients
We “collaborate” with such luminaries as the legendary professor Renat Akchurin, that is, if you have a complex problem, we will try to get you to an academician. We also work with the world-famous cardiac surgeon Maruo del Giglio , as well as with famous Israeli cardiac surgeons Amir Kramer and Dmitry Pevny , and other highly qualified specialists in whom we have complete confidence. The medical team involved in the operation and nursing is also highly qualified and gives our patients maximum attention.
What do you get when you seek treatment from us: