Essence, indications and contraindications
Attention! Only your attending physician will give you health recommendations that are relevant to you. The article contains only general information that will help you navigate the problem.
As a rule, the operation is performed when the patient’s coronary bed is affected by 75% or more, and angina pectoris is resistant to medications.
During the operation, an additional path is created for blood flow to the heart, bypassing the arteries affected by atherosclerosis. The donor of shunts, vascular grafts, is the patient himself - they are taken from the internal mammary artery, the great saphenous vein in the leg or the radial artery in the arm. The duration of the operation depends on the number of affected arteries - on average, 4-5 hours.
Also, before surgery, it is necessary to take into account such risk factors as:
- diffuse lesions of all coronary arteries
- heart failure and kidney failure
- scarring and decreased performance of the left ventricle by more than 30%
- oncological diseases
- chronic nonspecific lung diseases: bronchitis, pneumonia, asthma, emphysema
What types of heart surgeries are there?
During a palliative operation, another “defect” is surgically created, which the child does not initially have, but thanks to which the circulatory pathways in the large and small circles disturbed by the defect are changed. This includes surgical expansion of the atrial septal defect, all options for intervascular anastomoses - i.e. additional shunts, communications between circles. The Fontan operation is the most “radical” of all such methods; after it, a person lives without a right ventricle at all. For some of the most complex heart defects, it is impossible to correct anatomically, and surgical treatment aimed at correcting blood flow can be called a “definitive” palliative correction, but not a radical operation.
In other words, in case of heart defects, when the intracardiac anatomy - the structure of the ventricles, the state of the atrioventricular valves, the location of the aorta and pulmonary trunk - is changed so much that it does not allow for a real radical correction, today's surgery follows the path of eliminating poorly compatible conditions as early as possible. life of circulatory disorders, and then long-term palliation. The first stage of this path is saving a life and preparing for further treatment, and protecting against future complications, the second is the final stage of treatment. All together, this is a long path to the final operation, and on it it is necessary to overcome one, two, and sometimes three steps, but, ultimately, to make the child healthy enough for him to develop, learn, and lead an ordinary life, which this long-term palliation will provide for him. Check it out, not so long ago - 20–25 years ago this was simply impossible, and children born with defects of this group were doomed to death.
Such “final palliation” is the only way out in many cases; although it does not correct the defect itself, it provides the child with an almost normal life by improving the mixing of arterial and venous blood flows, completely separating the circles, and eliminating obstacles to blood flow.
Rehabilitation after bypass surgery
“Compliance with the stages of treatment reduces the risk of re-operations by 4 times, re-hospitalizations by 6 times, mortality as a result of relapse of the disease by 2.5 times... Saving costs for the treatment of relapses is 30-40%”
E.V. Shlyakhto, chief cardiologist of St. Petersburg and the Northwestern Federal District, President of the Russian Society of Cardiology.
Competent rehabilitation after coronary bypass surgery helps:
- eliminate the negative consequences of surgery
- consolidate treatment results
- restore physical activity and cope with psychological trauma
- block the further development of coronary heart disease and possible future complications
Effective rehabilitation implies an integrated approach to the physical and psychological condition of the patient. It lasts, on average, from 6 to 12 months and includes the stages of an inpatient department, a cardiological sanatorium and outpatient observation.
Inpatient rehabilitation department
The task of the first stage of rehabilitation is to control and stabilize the body’s condition after surgery, physical activation and psychological adaptation to the operation.
The minimum length of stay for a patient in the hospital is 7-10 days, the specific period is determined individually, depending on the complexity of postoperative complications.
During this period, the patient receives the following medical care:
- Drug treatment - control of pain symptoms, stress on the heart muscle and the formation of blood clots in shunts.
- Restoring physical activity - learning how to turn over in bed correctly, when you can sit up, get out of bed and walk. Important: if you do not devote time to physical activity from the first days after surgery, the risk of complications increases.
- Psychological adaptation involves working with the fear of heart weakness and the mindset that the pain will return. Statistics show: 60% of patients after bypass surgery are afraid of being left without constant medical supervision. Many believe that the heart may not be able to withstand it, remembering that the slightest load before the operation caused angina pectoris.
At the end of the inpatient rehabilitation phase, the patient undergoes a cardiac examination, and also, in many cases, a bicycle ergometer test, which determines exercise tolerance. Based on the data obtained, a plan for further rehabilitation is drawn up.
Rehabilitation center of the cardiological sanatorium
Monitoring and rehabilitation of the condition after bypass surgery and discharge from the hospital continues at the stage of the cardiological sanatorium. It is necessary to consolidate the result and effect of treatment, stabilize the patient’s physical and psychological condition, and prepare him for a return to normal life: everyday stress, socially active and work activities.
During this period the patient undergoes:
- an individually designed program of treatment, training and exercise therapy, taking into account the required rate of recovery, as well as the body’s capabilities
- program for normalizing the psycho-emotional state - analysis of the reaction to the disease, psychological support
- secondary prevention to prevent complications of the underlying disease and eliminate risk factors.
The rehabilitation stay in a cardiological sanatorium is usually 18-21 days.
Let us note that only a center can cope with the task, which combines extensive experience, a solid methodological base and qualified specialists: a cardiologist, psycho- and physiotherapist, doctors and exercise therapy instructors with special training, laboratory and functional diagnostics specialists.
Outpatient rehabilitation
Only a conscious and responsible attitude to health after the main stages of rehabilitation will help maintain the effect of treatment for as long as possible. Therefore, after discharge from the cardiological sanatorium, it is necessary:
- Register with a cardiologist at your place of residence and undergo observation once every 3 months. An appointment with a cardiac surgeon is required once a year.
- Give up bad habits - smoking reduces the life of shunts by at least half, and alcohol increases the load on the heart
- Purposefully increase the amount of physical activity - walking, climbing stairs, gymnastics without the active participation of arms and shoulders. It is important to remember that there should be no pain.
The Chernaya Rechka cardiological sanatorium specializes in the rehabilitation of patients who have suffered a myocardial infarction and bypass surgery, stenting and valve replacement. Over the 60 years of operation of our center, we have helped restore the health and ability to work of more than 650,000 patients. Read more about the rehabilitation program and how to get into it so we can help you too!
Inside the vessel
Alexander Melnikov, AiF: David Georgievich, you were the first in Russia to perform operations for heart attacks. But doctors have always insisted that operations are contraindicated in case of a heart attack...
Related article Cardiologist: Bitter people are more likely to have a heart attack and stroke
David Ioseliani: The cause of myocardial infarction is blockage of a vessel by a thrombus; it usually forms on an atherosclerotic plaque. In the area where this vessel is located, the heart muscle dies - it lacks oxygen.
But the death of muscle cells of the heart is usually extended over time for 6-8 hours, and sometimes the agony extends even up to two days, the body turns on compensatory processes. And, if blood flow is restored, the area of necrosis (death of muscle cells) will be significantly smaller.
As a result, the consequences of a heart attack will be less serious, there is less risk of developing heart failure, aneurysm, arrhythmias, etc. And if blood circulation is restored within an hour after the onset of the attack, the consequences of a heart attack can be avoided altogether.
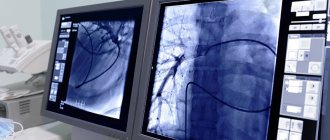
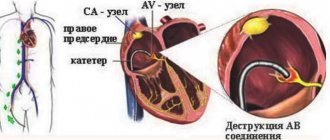
Now about surgery. We are not talking about a major operation - we operate endovascularly, which literally means “inside the vessel.” We bring a catheter through the arteries to the vessels of the heart and, under X-ray control, inject a contrast agent into them.
Article on the topic
Chief cardiologist of Moscow: “The heart cannot withstand the modern rhythm of life”
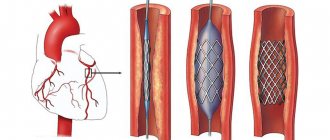
We determine where the vessel is blocked and open it - we pass through a catheter with a special balloon, inflate and expand the lumen of the vessel. And that’s basically it – blood flow is restored. Usually in such cases we also place a stent so that the lumen remains open, even if it is narrowed by plaque.
In fact, this is the so-called balloon angioplasty, and today it is already a routine operation. Even in Russia, it is already done in many places, but not for a heart attack, but as planned.
A heart attack has its own specifics. It is very important to start treating the patient at the pre-hospital stage: emergency doctors should, as early as possible, administer special drugs to the patient that stop the growth of a blood clot - thrombolytics. And organizing this is the most difficult thing, because such medicine costs about a thousand dollars.
But we managed to achieve this in Moscow, and now 40-50% of heart attack patients receive just such treatment in an ambulance, and then they are brought to special centers where they perform angioplasty, which I just talked about. Ours was the first such center in the capital, but now they operate at 13 city hospitals. They are led by my students.
Space numbers have become real
– That is, an emergency hospital, the structure of which will include a vascular center, can be said to be an ideal fit?
– Our structure for providing care to patients with cardiovascular diseases has been working for several years. Judge for yourself: in the emergency hospital there are three departments of cardiology, departments of X-ray surgery, neurosurgery and neurology - these are six departments that, in principle, should deal with vascular accidents. In 2014, I was appointed head of the department of x-ray surgical methods of diagnosis and treatment of the hospital, and we were faced with a problem: there are many patients, but we operate on few. Why? The new technologies that we have begun to introduce are very expensive. Stents, catheters - all this equipment is miniature, disposable, but minimally invasive methods allow you to solve the patient’s problem quickly and with minimal losses. We managed to create a small bed capacity in the X-ray surgery department, a prototype of a future vascular center, although not with the same capabilities as now. It was opened on January 1, 2016 by decision of the city duma, the regional Ministry of Health and the health department of Rostov-on-Don. We were given quotas for 300 operations per year. Then we performed 150 operations a year, half as much! We mainly operated on patients with heart attacks and pre-infarction conditions. The question became: where to find specialists? We recruited staff in four months, and now they are a very strong, united team. Currently we perform about 900 operations per year.
– Where did you find good specialists? Lured from other hospitals, discharged from Moscow?
– To be honest, we raised ourselves. They sent me to various symposiums and advanced training courses. You can go anywhere, but within reasonable limits. There is a sea of information, and we still need to cope with it, and while studying theory, we must not forget about practice. The surgeon does not have time to sit and think; the surgeon makes a decision within a second.
In parallel with the x-ray endovascular surgeon, cardiologists, resuscitators-anesthesiologists, and ultrasound doctors immediately join the work. Patient logistics are structured in such a way that the diagnostic stage takes 5–7 minutes. And a decision follows. In particularly difficult cases, we assemble a consultation of a multidisciplinary team of doctors.
Extensive myocardial infarction
Extensive myocardial infarction means damage to a large area of the heart muscle. Its most serious form is transmural infarction, in which necrosis extends to the entire thickness of the myocardium. Thus, the main thing that distinguishes an extensive myocardial infarction from a small focal one is the scale of necrosis of cardiac tissue. This also determines the more pronounced symptoms, as well as the much more serious consequences of this clinical form. While a small focal heart attack is often carried on the legs, a large myocardial infarction requires emergency hospitalization.
Symptoms of extensive myocardial infarction have several clinical forms - angiotic, gastralgic, asthmatic, cerebral, edematous.
Angious symptoms of extensive myocardial infarction are acute pain behind the sternum and in the region of the heart, radiating to the left arm, under the shoulder blade or to the neck, lower jaw. The pain is accompanied by fear of death, anxiety, pale skin, and cold sweat. With extensive myocardial infarction, a person can only be in a sitting position with his legs down. When lying down, severe discomfort is felt due to the influx of venous blood.
Extensive myocardial infarction is usually accompanied by an increasing cough and shortness of breath (asthmatic form). In some cases, a heart attack can be mistaken for food poisoning due to symptoms such as vomiting, cramping pain in the upper abdomen, diarrhea, and the urge to defecate. This is the so-called gastralgic form of heart attack. Another symptom of extensive myocardial infarction is the occurrence of edema.
Cerebral symptoms of extensive myocardial infarction are associated with impaired cerebral circulation - dizziness, loss of consciousness (fainting), speech impairment, headache, unilateral numbness of the arms and legs. There may be no chest pain.
The main and most serious complications of extensive myocardial infarction are heart failure, pulmonary edema, thromboembolism, and myocardial rupture. Treatment of a large myocardial infarction begins in the intensive care unit or intensive care unit. The goal of intensive care is to prevent the most serious life-threatening complications. After this, inpatient treatment is carried out, after which a course of rehabilitation is recommended. Rehabilitation after a major myocardial infarction is necessary not only for maximum restoration of performance and quality of life, but also for the prevention of recurrent infarction.