Author
Frolov Konstantin Borisovich
Doctor
Candidate of Medical Sciences
Phlebologist
until January 31
You get 10% cashback when purchasing a gift certificate More details All promotions
Femoropopliteal bypass surgery
is a surgical intervention that restores blood flow bypassing the blocked section of the femoral artery.
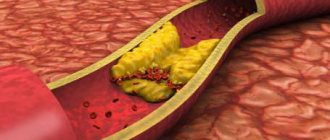
The operation is indicated for occlusion (blockage) of the femoral artery. The cause of occlusion in most cases is the development of atherosclerosis. With obliterating atherosclerosis of the arteries of the lower extremities, plaques form on the walls of the femoral artery, which, increasing, block the blood flow. As a result, the lower leg lacks fresh, oxygenated blood. This causes pain in the legs during physical activity, as well as intermittent claudication, when a person is forced to stop walking due to pain. At a later stage, ulcerative-necrotic changes may develop.
Femoral-popliteal bypass surgery is designed to restore proper blood supply to the lower leg, eliminate leg pain, and prevent the development of gangrene.
The essence of the operation is to install a shunt that connects the artery above and below the blocked area. In this case, the damaged section of the artery is usually not removed. As a rule, the patient’s own vein is used as a shunt (the absence of a vein is easily compensated by the body); in some cases, a synthetic prosthesis is used. An incision is made in the groin area where the shunt is sutured to the femoral artery. Through a special channel, the shunt is brought to the lower part of the leg, where it is sewn into the popliteal artery.
The operation is performed under general anesthesia or (more often) epidural anesthesia. Epidural anesthesia involves installing a thin catheter in the area of the spinal cord roots, which allows you to reduce the dosage of the pain medication.
The average duration of the operation is 3 hours.
Briefly about the treatment method
Vascular bypass (Bypass) is an operation to create a bypass when a vessel is blocked by atherosclerotic plaques or blood clots.
Arterial bypass surgery is used for severe forms of arterial circulatory insufficiency. Bypass surgery allows you to save a limb in case of gangrene. A shunt is placed from the artery above the blockage to the artery below the lesion, completely restoring blood supply to the affected organ. Most often, to bypass the arteries of the lower extremities, the patient's own saphenous veins are used, which are treated in such a way as to carry blood to the leg, and not back.
Advantages of treatment at the ISC
The Innovative Vascular Center is the only clinic in our country where unique microsurgical, endovascular and plastic methods are comprehensively used to treat patients with incipient gangrene and diabetic foot. Vascular surgeons at our clinic successfully use the method of restoring blood circulation in the limb using a microscope, developed at the University Hospital of Aachen (Germany), for patients with damage to the small arteries of the leg and foot. This is a microsurgical bypass of the arteries of the leg and foot using the patient’s own saphenous vein. Microsurgery allows the successful connection of vein grafts and the smallest vessels with high quality. This allows doctors at our clinic to save limbs for patients already sentenced to amputation.
Since 2011, our clinic has been a leader in Russia in the use of bypass surgery of the arteries of the leg and foot and has the best results in preserving limbs against the background of atherosclerosis of small arteries.
Indications and contraindications for the treatment method
Patients who are in good general condition are selected for bypass surgery. Therefore, a detailed assessment of comorbidities, obesity and other life-threatening factors is carried out. Only an immediate threat to life is a reason for risk in patients with severe concomitant diseases.
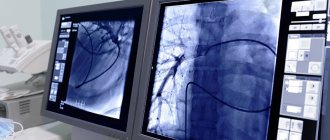
It is necessary to evaluate the vascular bed in detail using diagnostic ultrasound and angiography in order to formulate a clear concept for the operation.
A careful assessment of the saphenous veins is necessary, since the success of bypass surgery and the duration of the bypass operation depend on their quality. The use of artificial prostheses as shunts is an operation of despair, since such shunts close in half of the cases within 2 years.
Postoperative care and sustainability of the result
How long a shunt lasts depends in part on the graft material. Veins have venous valves that protect against calcification and blood clots. Care must be taken to ensure that they are not prematurely damaged by other factors such as re-calcification. To prevent the formation of deposits in the junctions and venous valves, long-term therapy with an anticoagulant drug is recommended after surgery. Heparin is suitable for this immediately after surgery, and platelet aggregation inhibitors for long-term prophylaxis, such as aspirin 100 mg once daily or Marcumar. Because the shunt usually consists of its own vessel, it is not rejected by the immune system. The shunt grows into the existing vascular system relatively quickly, but can also close over time. The rate of obstruction depends on the shunt material and location. In the hip area, an average of 60-80% of shunts are still open after 5 years, in the lower leg area -50-70%. Plastic shunts on the lower limb are an exception today. In 70-90% of cases, the plastic shunt is usually clogged after five years.
If many of the risk factors and comorbidities of peripheral arterial occlusion persist after bypass surgery, it is likely that over time the bypass will also become affected by atherosclerosis. Then the blood supply to the lower limb through the shunt will not be sufficient and repeated intervention will be required. Therefore, after bypass surgery, as many risk factors as possible should be eliminated, because surgery is not a cure for this disease, but only reduces the symptoms of occlusion.
You should undergo regular inspection every 3-6 months. It is strongly recommended to visit your family doctor periodically to minimize and control risk factors.
Preparing for treatment
To determine the indications for femoral-tibial bypass surgery, the patient must be examined in terms of vascular lesions and general health.
The following methods are used to diagnose vascular lesions:
- Ultrasound of the arteries of the lower extremities with pressure measurement at the ankles
- Multislice computed tomography with contrast of the aorta and arteries of the lower extremities
- X-ray contrast angiography - most often used to accurately determine the possibility of angioplasty, instead of bypass surgery
- Duplex scanning of saphenous veins - to determine their suitability as a bypass
General diagnosis of the patient includes:
- General blood and urine tests
- Blood chemistry
- Blood tests for syphilis, HIV and hepatitis
- Electrocardiogram (ECG)
- Ultrasound of the heart (echocardiography)
- Ultrasound of the carotid arteries
- EGDS (gastroscopy of the stomach)
- Chest X-ray
The actual preparation for surgery is to reduce the swelling of the affected leg. To do this, the patient is first given prolonged epidural anesthesia (so that he can lie down). Before surgery, a catheter is inserted into the bladder to monitor urine output. For the purpose of administering medications, an intravenous catheter is installed in the subclavian vein.
On the eve of the operation, the patient is given sedatives, which are supplemented with premedication immediately before the patient is taken to the operating room.
Pain relief during treatment
Surgeries on the arteries of the lower extremities in our clinic are performed under epidural anesthesia. The latter involves the introduction of an anesthetic drug into the epidural space of the spine. This type of anesthesia can effectively eliminate pain during surgery and in the early postoperative period.
To monitor the state of the cardiovascular system, we use tracking monitors that are connected to the chest to take an ECG and to the upper arm to monitor blood pressure. In order to improve blood oxygen saturation, the patient is given an oxygen mask.
How the treatment method works
The patient is placed on his back in the operating room. A special cushion is placed under the knee of the operated leg.
The operation begins with a revision (assessment) of the arteries of the leg, to which the shunt should fit. To access the arteries of the leg, incisions 4-6 cm long are used in the groin area and on the lower leg (foot). The artery in the thigh is then accessed to assess its suitability as a donor for the bypass.
After assessing the arteries, the surgeon begins to prepare a venous bypass. Through small incisions, the saphenous vein is exposed on the lower leg, then on the thigh.
The first connection is made between the great saphenous vein and the femoral artery. After stitching the anastomosis, blood flow starts. Shunt pulsation is possible up to the first venous valve.
Then a special instrument with a valvulot is inserted into the venous shunt and the valves are excised. This is necessary so that blood flow can go through this vein from the femoral artery to the artery of the leg. Without cutting the valves, blood will not flow through the shunt.
After removing the valves, the surgeon evaluates the vein using ultrasound and finds blood discharge through the shunt into the side branches. These branches are ligated through separate small incisions. This is necessary so that the blood through the venous shunt moves in the direction of the foot, and does not go into the lateral branches.
When all the discharges along the venous shunt are tied, we begin suturing the shunt and artery on the leg or foot under a microscope. High magnification at this stage is necessary for success, since any error in this will result in failure of the entire bypass operation.
Then the blood flow is started and the operation of the shunt is checked using ultrasound. If blood circulation is restored, the operation ends with suturing of the wounds. If there is any doubt, control angiography is performed and, if necessary, angioplasty of the altered artery below the shunt.
Surgery
Bypass surgery of the blood vessels of the legs is a complex operation that requires high professionalism and certain experience from the surgeon. The operation is performed under general or local anesthesia, depending on medical indications and the general condition of the patients. Epidural anesthesia is considered a modern priority method of pain relief, significantly reducing surgical risk.
Bypass surgery is performed when the patency of arterial and venous trunks is impaired, if their obstruction is more than 50% of the diameter. During the operation, a bypass path is created using a graft from the beginning of the obstacle to its end. Correctly performed surgery ensures restoration of blood flow in the affected vessels.
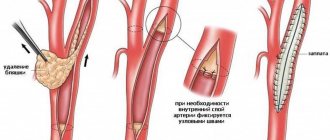
Stages of the operation:
- A layer-by-layer dissection of the skin and underlying tissues is performed above and below the affected area.
- The vessel is isolated, inspected and its suitability for the upcoming bypass is determined.
- The vessel is incised below the lesion, a shunt is sewn in, and then fixed from above.
- Check the integrity of the implant.
- After assessing the state of blood flow and pulsation of the arteries, deep tissues and skin are sutured.
There are several options for bypass surgery. The choice of each is determined by the localization of the affected area. Immediately after the operation, patients are put on an oxygen mask and given intravenous drips of painkillers.
For the first two days after surgery, patients are prescribed bed rest. Patients are then allowed to walk around the room and hallway. Cold compresses applied for 20 minutes will help relieve pain and reduce swelling of injured tissues during the first 24 hours. All patients are advised to wear compression stockings and socks to prevent blood clots. An incentive spirometer should be used to improve lung function. Doctors examine the incisions daily for possible infection. For 10 days after the operation, specialists conduct dynamic monitoring of the patient, examining indicators of the body’s basic vital functions.
Vascular bypass does not eliminate the etiological factor of the pathology, but only facilitates its course and the condition of the patients. Complex treatment of the underlying disease includes not only surgery, but also lifestyle changes that prevent further development of the pathological process.
Possible complications during treatment
In situ femoral-tibial bypass.
This method involves the use of the patient’s own great saphenous vein, which remains in its usual place, but with the help of special techniques, arterial blood flow is allowed through it into small arteries on the lower leg and foot. Femoro-tibial bypass is the mainstay of treatment for critical ischemia and impending gangrene. Success, with the correct indications for surgery, is achieved in 90% of patients with incipient arterial gangrene (necrosis of the fingers, arterial trophic ulcers). The ability to walk on your own leg is preserved. A venous bypass can be made from the veins of the legs or arms if the main saphenous vein is not preserved.
Peroneal artery bypass
The smallest artery of the leg is the least affected by the atherosclerotic process. However, its capacity is often not enough for the full operation of the autovenous shunt, which leads to thrombosis. The peculiarity of operations on the peroneal arteries is the need to clearly assess the volume of blood flow. To unload the artery, special techniques are often used - unloading fistulas with veins far from the anastomosis.
Multi-storey "jumping" shunts
Patients are often denied leg preservation due to the lack of a good length and patent artery in the lower leg, however, we often see individual sections and branches of arteries with preserved blood flow. Our leading vascular surgeon I.M. Kalitko For such situations, a technique for multi-story bypass of the lower leg arteries has been developed. Often several short bypasses are performed to individual patent segments of the arteries. An important condition for the normal operation of such a complex reconstruction is a reliable assessment of the incoming and distributed blood volume. When shunts are overloaded, unloading fistulas can be used.
When is leg bypass surgery required?
Leg bypass surgery is sometimes necessary for peripheral arterial occlusive disease (PAA). With this disease, partial or complete occlusion of an artery located at a distance from the heart occurs. This leads to a decrease in arterial blood flow. In most cases, the legs are affected. The cause in 95% of cases is atherosclerosis, as well as a chronic process. Acute occlusions due to clots are very rare.
Peripheral arterial occlusion is classified according to severity into four Fontaine stages. The leading symptom of the disease is the so-called intermittent claudication: pain during exertion in the affected area of the body due to insufficient blood supply. For stages III and IV or acute vascular occlusion, interventional or surgical therapy (for example, bypass surgery) should be performed. Stage III is characterized by pain at rest, and stage IV is characterized by tissue damage due to decreased blood flow. If there is extensive damage to the tissue of the legs or a high risk of infection, bypass surgery is not possible, and amputation remains as a last resort.
Prognosis after treatment method
General surgical complications:
- Bleeding during surgery is a rare occurrence; usually blood loss is 300-500 ml and does not require replacement.
- Suppuration of postoperative wounds - can be observed in weakened patients with diabetes and a purulent process on the foot. Most often the course is favorable, but it delays the patient’s recovery.
Specific complications:
- Reperfusion syndrome is a limb condition associated with the restoration of blood flow against the background of critical ischemia. It is characterized by severe swelling of the limb, pain, and hyperemia. Usually goes away within 2-3 weeks after surgery.
- Lymphorrhea is a prolonged leakage of lymph from incisions. A rare complication in our clinic, the cause of which is damage to enlarged lymph nodes in the groin area during surgical access to the femoral artery.
- The formation of false mycotic shunt aneurysms is a rare complication that occurs when an infection is associated with an autovenous shunt. This is a dangerous condition as it can lead to late shunt rupture or thrombosis.
- Thrombosis of an autovenous shunt can be early or late. Early thrombosis is associated with insufficient outflow through the shunt due to poor arteries below the shunt or high blood clotting. Late thrombosis is associated with the progression of atherosclerosis in the outflow or inflow arteries and scarring of the shunt itself. The use of anticoagulants and control angiography after bypass surgery can eliminate the causes of early thrombosis. To prevent later complications, observation by a vascular surgeon is necessary.
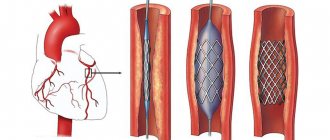
Which is better: a stent or a shunt?
If we compare two methods for correcting myocardial ischemia and hypoxia through the vessels supplying the muscle, the advantages and disadvantages of stenting and bypass surgery of the heart vessels become obvious:
| Evaluation criterion | Stenting | Bypass surgery |
| Scope of intervention | Minimal, intravascular | Technically complex intervention |
| Operation duration | From an hour to three | From three to nine or more |
| Heart failure | Need not | More than half of operations take place with the heart stopped |
| Incision | Deleted | The sternum is cut |
| Anesthesia | Local, less often - taking into account the individual threshold of pain sensitivity | Deep anesthesia |
| Rehabilitation | A few days | Up to six months |
| Acute cases | Relief of AMI is practiced | Not allowed due to the severity of the intervention |
| Capillaries | Correction of vessels with a diameter of 3 mm is possible | Cannot adjust small branches |
| Restoration of blood flow | For several years | Up to 10 years or more |