Sometimes problems with the cardiovascular system become so serious that conservative treatment methods no longer have the desired effect. If the patient is diagnosed with atherosclerosis, which has seriously affected one or more vessels, surgical intervention is indicated. In the problem area, certain manipulations are carried out aimed at restoring normal vascular patency and the correct functioning of the entire cardiovascular system.
If blood vessels are blocked by atherosclerotic deposits, the heart tissue experiences oxygen starvation. This leads to the occurrence of coronary disease. This condition is extremely dangerous for the patient’s life, especially in the case of complete blockage of the vessel, which entails myocardial infarction. However, today there are effective methods for treating coronary heart disease - stenting and bypass surgery.
What are coronary stents and why are they needed?
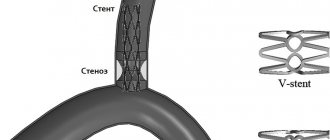
A coronary stent is a medical device that is a frame in the shape of a metal cylinder, installed in narrow places in the artery (with cholesterol deposits) to widen them, thereby ensuring normal blood flow.
Stents can combat arterial stenosis that occurs due to the deposition of atherosclerotic plaques. Cholesterol is deposited on the walls of the arteries and narrows the lumen, thereby preventing blood flow. Poor blood flow causes oxygen starvation and lack of nutrients in the organs. One of several ways to relieve such bottlenecks in the arterial system is stenting. Installation of a stent is not always indicated for the patient, but only in some severe cases when there are no contraindications, but more on that later.
Application area
One of the common causes of the development of heart pathologies is a decrease in vascular elasticity and vasospasm. The arteries gradually lose their ability to expand, which leads to local disturbances in blood supply. Also, if the process is chronic, this contributes to the accumulation of cholesterol deposits on the vascular walls. Scientists all over the planet are actively working to develop an effective method to combat this disease. Coronary stenting is one of the existing ways to solve the problem.
Stenting is a procedure for integrating a special dilating device into a vessel. It is a tube with a mesh texture that can take the desired shape when implanted. The device acts as a frame. As a result, the narrow or spasmodic section of the artery should expand, and the blood flow should return to its previous state.
This treatment method belongs to endovascular surgical interventions and is considered minimally invasive. It is performed exclusively by experienced surgeons of the highest category.
Let's consider the stenting algorithm using the heart as an example. The catheter on which the element is fixed is passed through the femoral artery through the introducer. The conductor must be moved to the designated area where it is planned to install the expander. As soon as the catheter is inserted, the artificial frame is fixed, inflated under the action of the balloon, and normalizes blood supply to the heart muscle.
The operation involves local anesthesia. The average duration is relatively short, from 20 minutes to 3 hours. If necessary, the surgeon installs several devices at once.
Indications
Installation of coronary stents may be indicated by a doctor in the following cases:
- complete blockage of the coronary artery during or after myocardial infarction;
- narrowing or complete blockage of the arteries with a high risk of heart failure;
- narrowing or complete blockage of blood vessels with a high risk of severe angina.
Stenting is done only in cases where there are no contraindications to the operation. In another case, bypass surgery is performed.
When is bypass surgery performed?
Shunting is performed in the following cases:
- it is impossible to install a stent without surgery;
- the affected vessel has a miniature diameter;
- large extent of atherosclerotic changes in blood vessels;
- two or more vessels are affected, which is accompanied by multiple blockages of the lumens.
The operation has a number of contraindications. Bypass surgery should not be performed on elderly patients with severe concomitant diseases. Sometimes doctors are forced to urgently perform an operation even if there are contraindications, but then the risk of death increases significantly, of which the patient’s relatives must be notified.
Contraindications for surgery
- If intervention is required in an artery with a diameter of less than 3 mm.
- If the patient has a large number of cholesterol plaques, more than 1 centimeter in length.
- If the patient is allergic to iodine-containing drugs.
- If the patient has a large number of cholesterol plaques, more than 1 centimeter in length.
- If the patient has poor blood clotting.
- If the patient has a serious condition, accompanied by a drop in blood pressure, impaired consciousness, shock, liver, kidney or respiratory failure.
- The patient has malignant tumors that cannot be treated.
If a patient is contraindicated for stenting, but still wants this operation, then in some cases he may insist on having it performed at his own risk.
Prognosis after treatment
Coronary angioplasty significantly increases blood flow through a previously narrowed or blocked coronary artery. In this case, chest pain (angina) should usually decrease, and the physical capabilities of the body, on the contrary, should increase.
You need to understand that angioplasty and stenting do not cure coronary heart disease, but only eliminate specific circulatory disorders of the heart muscle. To achieve a stable result, you must lead a healthy lifestyle and take medications prescribed by your doctor.
If the symptoms of angina return, then you need to contact your doctor again, and if you have chest pain at rest that does not respond to nitroglycerin, then call an ambulance.
After coronary angioplasty and stenting, the quality of life improves in 95% of patients, with many of them maintaining the effect for more than 5 years.
Types and types of coronary stents
Stents differ from each other:
- Length. The size of the stents varies from 8 to 38 millimeters.
- Diameter. There are from 2.25 to 6 millimeters.
- By design. They differ in the shape of the elements from which they are created.
- Material. They are made from steel, cobalt-chrome, PLLA polymer and others.
- Coated. Stents are available without coating or with drug coating Sirolimus, biolimus and others.
- Method of disclosure. They can open either independently or with the help of a balloon on a catheter.
- By type of drug coating. The medications used are Sirolimus, everolimus, paclitaxel and others.
By lenght:
Stents are available: 8, 10, 13, 16, 18, 23, 28, 33, 38 mm.
By diameter:
Stents are available: 2.25, 2.5, 2.75, 3, 3.25, 3.5, 3.75, 4, 4.25, 4.5, 4.75, 5, 5.25, 5.5, 5.75, 6 mm.
By design:
- mesh (made of woven mesh);
- tubular (from a tube);
- wire (made of wire);
- ring (from separate rings).
According to the material from which the frame is made:
- stainless medical steel;
- cobalt-chrome alloy;
- alloy of platinum and chromium;
- polylactose acid (PLLA) polymer.
By type of coverage:
- Uncoated with bare metal.
- Drug-coated, which releases a drug that reduces the likelihood of future artery narrowing.
- With double coating - external and internal, to heal the artery itself and prevent the formation of blood clots.
- Coated with antibodies, attracting endothelial cells, reducing the risk of thrombosis.
- Dissolving, made from a material that dissolves and releases a drug coating that prevents the recurrence of stenosis.
By opening method:
- self-expanding;
- opened by a balloon.
By drug coverage:
- Sirolimus;
- Zotarolimus;
- Everolimus;
- Biolimus;
- Paclitaxel.
Depending on the manufacturer, stents may differ in their characteristics and price. In Russia, the production of stents is carried out in accordance with GOST R ISO 25539-2-2012.
Stenting or bypass surgery: pros and cons
Let's start with the fact that each method of operation has its pros and cons. Stenting (angioplasty with stenting) is performed if the arteries are affected in 1-2 places. If three or more vessels are affected, and also if the plaque is long-lasting, then, of course, bypass surgery .
Rice. Angioplasty with stenting
Stenting
Stents are placed on balloons, which allows them to have very small dimensions when unexpanded, and after the balloon is inflated inside the coronary artery, they expand, remaining in this position forever.
When stenting blood vessels, the lumen of the affected artery is restored to normal diameter. Stenting is performed invasively, through a catheter with a stent at the tip. The catheter is moved to the desired area, after which a stent is installed, which forms the required width of the vessel, and as a result, blood flow is normalized. In addition to low morbidity - no need to cut the chest - this procedure has a number of other advantages. This operation does not require general anesthesia, it has a short rehabilitation period and a minimal number of complications.
Currently, a variety of stent models are used in interventional cardiology, differing from each other in certain design features. All of them are absolutely compatible with human organs and tissues, have a flexible structure and are elastic enough to support the artery wall.
Rice. Bypass surgery
Bypass surgery
Bypass surgery is performed through an open approach. This operation makes it possible to identify narrowing of the lumen of the vessel with higher accuracy. But at the same time, the postoperative period will be longer, since during the operation the chest cavity is opened. Like any surgical intervention, such an operation has its own risks; it should not be performed on patients of advanced age or with concomitant serious illnesses. The operation is performed under general anesthesia. It is more invasive and has a greater chance of complications, such as bleeding or infection.
Bypass or stenting?
Recently, cardiologists have given preference to stenting, which is performed without incisions in advanced medical centers.
Rice. Vessel stenting
Under X-ray control, a miniature balloon is inserted through a small puncture into the vessel affected by atherosclerosis, on which a thin metal tube-stent with a diameter of 2.5–4.5 mm is placed. The balloon moves into the narrowing area and inflates under pressure. The cholesterol plaque is flattened and the vessel expands to the desired diameter.
Rice. Coronary artery bypass surgery
With the development of stenting technology, the proportion of patients for whom bypass is only 5–10%. And this is understandable. Stenting is much less traumatic and the rehabilitation process after it is much faster (after 1–2 days the person is discharged home). It is not always possible to perform bypass surgery using minimal access. In addition, shunts made from your own veins inevitably age. They are susceptible to atherosclerosis and degenerative changes. At the same time, there are very few opportunities for re-restoring blood circulation. The same cannot be said about stents , which are now produced with a special drug coating that prevents restenosis (re-narrowing) of blood vessels.
Why is drug coverage important?
Drug coating of a stent plays a very important role in preventing restenosis (re-occlusion) of the coronary arteries at the site of its implantation. The drug coating (for example, sirolimus) consists of immunosuppressants, which in turn locally stop the growth of endothelial cells (the inner layer of blood vessels), thereby keeping the lumen of the vessel clear for blood flow.
Dr. BOSTI recommends high-quality stents Orsiro®, Magmaris® from BIOTRONIK (Germany)
The German company BIOTRONIK is a world leader in the production of coronary stents, introducing innovative and high-tech methods of diagnosis and treatment.
Rice. Orsiro® BIOTRONIK stent
Orsiro stent is indicated for complex patients and lesions, including:
- acute coronary syndrome;
- myocardial infarction with ST segment elevation;
- diabetes;
- high risk of bleeding;
- complex of lesions;
- small vessels;
- multi-vascular diseases.
Advantages and disadvantages of using stents
Stents are an outstanding invention that can save the lives of many patients. But it is not suitable for all patients suffering from stenosis. Like other medical instruments, stents have advantages and disadvantages.
Advantages:
- Minimally invasive, to eliminate the problem you do not need to make large surgical incisions on the body, but only a small hole on the body into which a catheter with a stent is inserted. Fast healing. The patient can be discharged on the 3rd day.
- Use of local anesthesia during surgery. There is no need to put a person to sleep. High percentage of successful cure (90%).
Flaws:
- There is a possibility of secondary stenosis, the appearance of blood clots and heart attacks. Occurs in 10% of patients.
- Complexity of the operation. The installation of stents in the heart is performed only by highly qualified surgeons.
- Some drug-eluting stents are expensive.
- Not all patients can undergo stenting - there are contraindications.
Differences between operations
To clarify which is better: stenting or cardiac bypass surgery, let’s summarize the differences between the operations:
- Anesthesia. For stenting, local anesthesia in the area of the artery through which the prosthesis is inserted is sufficient. The operation does not require large incisions or stitches. Shunt installation is a long and complex procedure performed under general anesthesia.
- Providing access. The femoral artery is used to insert the stent. The shunt requires more extensive access. Surgeons have to make an incision in the sternum, sometimes in the ribs or intercostal spaces, and open the pericardium.
- Age of patients. Installation of a shunt is indicated if stenting is not possible. Accordingly, the age of patients with a shunt is much older.
- Use of a heart-lung machine. Used to create a shunt when it is necessary to turn off the heart. In the case of stenting, this is not necessary.
- Angiography. X-ray examination of blood vessels with the introduction of a contrast agent is necessary before surgery. Stenting is performed with coronary angiography, and a shunt is attached after it.
- Duration of the operation. It only takes a few minutes to install the stent. Creating a shunt is a long-term intervention, lasting up to 6 hours. The duration of the procedure also depends on the number of affected areas.
- When they are discharged. Stenting does not require long-term medical supervision, so the patient is sent home within 24 hours. After installation of the shunt, the patient remains in the clinic for another 10-14 days.
- Rehabilitation period. Recovery time after a stent is about 2 weeks. For a shunt, the period is extended to 3-4 months; during the operation, an incision was made in the sternum. After bypass surgery, the patient is recommended to wear a medical corset.
- Risk of relapse. After stenting, blockage of blood vessels develops faster. Being a foreign body, the stent provokes the formation of blood clots. Plaques can also form in the shunt, but this process is slow and can take up to 10 years. In both cases, if there is a relapse, repeat surgery is indicated.
- Life expectancy of patients. According to statistics, 95% of patients survive within a year. Within 5 years this figure is reduced to 86%. With bypass surgery, life is extended by another 15-25 years.
Having considered what cardiac bypass and stenting are, we can say that the first, although it is a complex operation, leads to lasting results and fewer relapses.
Difference between stenting and bypass surgery
Both surgeries are performed to improve blood flow in areas where the arteries are narrowed due to the formation of atherosclerotic plaques. The difference between these methods is in the way they solve the problem of stenosis.
The bypass method involves creating a section of artery that bypasses the problem area. Normal blood flow is ensured through this new area. A section of the saphenous vein of the femoral, radial or internal mammary vein is used as a shunt. Bypass surgery is performed under general anesthesia.
Stenting involves installing a stent in a narrow place in an artery and expanding it, thereby normalizing blood flow. In this case, a shunt is not used, but the problem area in the artery is simply restored. The stent is inserted into the artery using a catheter with a balloon through a small hole in the body. At the desired location, the stent is expanded using a balloon and the catheter is pulled out. The operation takes place under local anesthesia.
Both methods are now used in medicine. Each patient is better suited to a certain method of operation based on his diagnosis and condition. Stenting is a more advanced method of treating stenosis, but it may be contraindicated for some.
What is cardiac stenting?
Stenting is a more modern, low-traumatic operation to restore the affected area of the vessel. The main direction of the intervention is restoration of the lumen of the vessel.
The essence of stenting is the introduction of a special balloon into the affected vessel, which opens under high pressure, destroys the atherosclerotic plaque and ensures patency of the vascular bed. The balloon is located in a stent - a special supporting structure made of a special alloy. When the balloon is deployed, the stent opens and remains in the vessel forever, fixing its walls and preventing the re-formation of atherosclerotic deposits. The balloon is removed from the artery.
Preparing for stenting
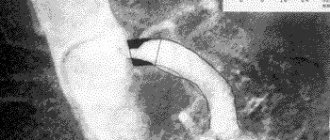
Before stenting, the patient is examined. They take basic tests, do echo and electrocardiography. Coronary angiography is performed by injecting contrast into the circulatory system and performing an X-ray examination. A map of the coronary arteries is obtained. The site of stent insertion is determined.
As a rule, to prepare for surgery, doctors may require:
- Avoid food and water 8 hours before surgery.
- Avoid taking blood thinning medications 3 days before stenting.
- Shave your groin and wash yourself.
- Eliminate or reduce the intake of glucose-lowering drugs 2 days before surgery.
Operation stages
- The operation is performed in an operating room equipped with an angiograph, which allows the doctor to observe the artery and the movement of the catheter on a monitor screen. The patient is placed on his back and sedated to keep him calm and relaxed.
- Doctors cover the patient with sterile linen and neutralize the stent insertion site.
- Local anesthesia is given.
- A thin wire is inserted into the artery through a needle, which acts as a conductor.
- An introducer is inserted along the guidewire, through which other instruments will be inserted into the artery and the wire is removed.
- Through the introducer, the doctor carefully inserts a thin catheter with a stent and a balloon.
- A contrast agent is injected into the coronary artery to accurately visualize the movement of the stent.
- The stent continues to be carefully moved to the desired location.
- The stent is expanded using a balloon on the catheter, thereby normalizing the diameter of the artery.
- After stent placement, the introducer and catheter are removed from the patient.
- A compressive bandage is applied to the catheter insertion site.
Differences from surgery
Angioplasty and stenting of the internal carotid artery (ICA) is considered a high-tech, minimally invasive endovascular intervention, performed under local anesthesia.
There are no scars left on your body on your neck, except for a very small cut - about 2-3 mm (puncture site) in a blood vessel in the groin or on the wrist.
There is no need for general anesthesia; everything is done under local anesthesia, so you are awake during the procedure. Fluids and medications are given through an IV.
Before the procedure
- You will be taken on a gurney to the cath lab operating room. You will place your head in a comfortable cup-shaped area on the operating table.
- Your wrists and groin should be shaved on both sides and prepared with an antiseptic solution.
- A local anesthetic is injected into the puncture site for pain relief.
- To monitor the ECG of the heart, electrodes will be connected to the chest.
During the procedure
Once you are calm, your operating x-ray surgeon will puncture an artery, usually the femoral artery in the groin area. The angioplasty and stent procedure are described below.
- A special catheter with a unique bend (tube) is inserted into the artery . Under X-ray control, a catheter with the necessary instruments and a balloon is brought to the narrowing of the carotid artery. You will not feel the catheter going through the arteries because the insides of the arteries do not have nerve endings. The entire instrument is guided through this catheter to the narrowed section of the artery.
- A radiopaque contrast agent (RCS) is injected into the carotid artery through a catheter . RCV may cause a temporary feeling of warmth on one side of your face. The RCV gives a detailed view of the narrowed artery and blood flow to the brain.
- The filter is opened in the artery . A filter, called an embolic protection device, is inserted beyond the narrowing to catch any particles that may break off from the narrowed section of the artery (plaque) during the procedure.
- A balloon catheter on the delivery system is positioned at the site of narrowing and inflated to dilate the vessel.
- A small metal mesh tube (stent) may be placed in the newly opened vessel . A self-expanding metal frame with a specially designed closed cell or double-layer stents that incorporate all the advantages of previous generations. The expanded stent provides support that helps prevent the artery from narrowing again.
- The filter, balloon and stent delivery system, and the catheter itself are removed.
When the procedure is complete, you lie still in one position and the bleeding stops at the site where the tube was inserted. You will usually not have stitches, but a bandage will be placed over the small incision. You are then transferred to a recovery room.
After the procedure
To avoid bleeding from the catheter site, you will need to lie relatively still for several hours. You will either be in the recovery area or in your hospital room. After the procedure, you may be given an ultrasound of the carotid artery. Most people are discharged from the hospital within 24 hours of the procedure.
The catheter site may be sore and swollen for several days. There may be a small hematoma in the puncture area. You can take medications in the recommended dose needed to relieve discomfort as prescribed by your doctor.
You may need to avoid vigorous activity and heavy lifting for a week after the procedure.
Is stenting possible during pregnancy?
Installation of stents is not recommended for pregnant women, as during the operation an X-ray is taken, which can be harmful during pregnancy. The operation can be stressful; the pregnant patient is given contrast, anesthesia and other drugs, which can also have a negative effect on the fetus. Some drugs may cause allergic reactions.
Surgery for pregnant women is prescribed only in extreme cases; the surgeon informs the patient in advance about the possible risks and consequences and performs the operation only with her consent.
Complications
In some cases, complications may occur after stenting. The reason may be an incorrectly performed operation or the characteristics of the patient’s body, how it reacts to the installed stent.
- Thrombus formation at the site of stent placement is the most common complication. To reduce the likelihood of blood clots, the patient is given blood thinning medications.
- Bleeding with hematoma. Occurs due to the introduction during surgery of drugs that reduce blood clotting. Rarely seen.
- Infection of the incision site where the catheter is inserted.
- Allergy to radiopaque contrast agent or drug coating on the stent.
- Re-narrowing of an artery in another location, as plaques carried by blood from a previously problematic area can break off and block another area in the artery.
- Restenosis is the body’s reaction to the installed stent, expressed in excessive growth of the inner lining of the vessel in the area where normal lumen was restored.
- Heart attack during stenting.
There is a greater risk of complications in patients with chronic diseases such as diabetes, kidney disease and blood clotting disorders. To exclude a number of complications, the patient is thoroughly studied before the operation and adjustments are made to the treatment, regulating blood clotting with medication, and selecting a stent with the desired drug coating. Carefully monitoring the patient's condition after surgery.
Recovery period
During this period, a set of measures is formed for the patient that will help him recover faster and reduce the risk of complications and recurrence of the disease.
After the operation, the patient lies in bed for 1-3 days in the hospital. At this time, doctors closely monitor the patient. After this, the person is discharged home, where he must also be at emotional and physical rest and observe bed rest. He should not take a bath or shower or exert himself physically.
During the recovery period, drug treatment is prescribed for six months, designed to reduce the risk of re-stenosis, thrombosis and heart attack. And increase the length and quality of life.
During the recovery period, the doctor prescribes everything necessary to:
- Improve a person's physical abilities.
- Restore heart functionality.
- Slow down the process of ischemia.
- Bring laboratory parameters back to normal.
- Prevent possible complications after surgery.
- To form in the patient a correct lifestyle that ensures longevity.
- Provide psychological comfort.
When is each operation assigned?
The main indication for both operations is narrowing of blood vessels or their complete obstruction. In atherosclerosis, plaques consisting of cholesterol and fat become overgrown with connective tissue and block the vessel. The consequence will be coronary disease, leading to a heart attack due to insufficient nutrition of the heart.
Stenting or bypass surgery of the heart vessels, in each case the doctor decides after assessing the condition of the patient and his blood vessels. The Syntax Score is used for this purpose.
During surgical practice, it was found that in case of a single lesion it is better to resort to stenting. In case of complex blockage of blood vessels, in difficult cases a shunt is installed. If the patient has 1 plaque, a stent is inserted. If there are several lesions, it is better to perform a shunt.
Drug therapy
After stent installation, the patient is usually prescribed the following medications:
- Antiplatelet, reducing the risk of blood clots. (Aspirin, Aspicard, Aspinat, Trombogard, Acetylsalicylic acid, Clopidogrel, Detromb, Trombex and others. Prescribed by the doctor to each patient individually.)
- Statins, which lower cholesterol levels and reduce the likelihood of restenosis. (Simvastatin, Pravastatin, Pitavastatin, Lovastatin, Atorvastatin, Rosuvastatin and others. Prescribed by the doctor to each patient individually.)
- Drugs that reduce the risk of heart attack.
The range of medications prescribed depends on the patient’s condition and health characteristics. It is necessary to strictly take in full all medications prescribed by the doctor for the period of treatment. After stenting surgery, it is strictly forbidden to self-medicate and take medications at your own discretion.
Disadvantages and advantages
Each method of surgical intervention has its own pros and cons. The doctor evaluates them before deciding on stenting or bypass surgery.
Installation of a shunt preserves the effect of the operation and improves the patient’s quality of life. Another plus is that there is less need for repeat surgery. The shunt allows you to cope with complex cases when drug therapy, stenting or angioplasty do not help.
But this type of operation has many contraindications. It is difficult for the doctor and the patient with a long rehabilitation period. The intervention requires open access.
Stenting solves the problem of single plaques. The operation is minimally invasive and is performed under anesthesia. The advantages include relative cheapness, speed and ease of implementation, and short rehabilitation.
But after stenting, there is a need to operate due to relapses of vascular blockage. The life expectancy of patients after stent installation is shorter than after bypass surgery.
Lifestyle change
Atherosclerosis, as a rule, is caused by an incorrect lifestyle, and in order to fully recover after surgery and avoid arterial stenosis in the future, it is necessary to change your lifestyle to a healthy one.
The transition to a healthy lifestyle is:
- Do morning exercises, move and walk quietly for 30 minutes - 1 hour about 3-4 days a week.
- Completely eliminate active and passive smoking.
- You can safely enjoy swimming, skiing, use an exercise bike or treadmill evenly and measuredly for up to 6 hours a week.
- Avoid alcoholic drinks.
- Avoid fatty, fried and salty foods.
- Do not consume more than 4 grams of salt per day.
- Drink tea instead of coffee.
- Attend examinations by your attending physician.
- Eat more vegetables, fruits, fish, rye and bran bread.
The diet and exercise program is prepared by the attending physician. For successful recovery, you must fully adhere to the schedule he has drawn up.
All articles →
| Our company offers high-quality stents for coronary vessels. You can familiarize yourself with the entire range of manufactured medical equipment for cardiac surgery in the website catalog. We are pleased to present you a coronary stent at a price affordable for every consumer! | Go to catalog > |
What is cardiac bypass surgery?
Bypass surgery is an operation to replace the affected area of a vessel. In the vast majority of cases, this is the coronary artery. Radical surgical intervention significantly increases the patient's life expectancy, reduces the risk of developing acute coronary syndrome, angina pectoris, and heart attack.
The operation lasts from 4 to 6 hours. The patient is put into medicated sleep. Access to the heart is made through an incision in the sternum or intercostal space. The essence of the operation is to create a bypass for blood flow. To do this, a section of the radial, internal mammary artery or femoral vein is taken (at the discretion of the doctor). The vessel is replaced, after which the chest wall is sutured.