An ophthalmological abnormality, known as hypertensive retinal angiopathy, often leads to a systematic and significant decrease in visual acuity. Despite the presence of complications, this pathology is not an independent disease. This type of angiopathy refers to the consequences of diseases of the cardiovascular system that occur against the background of a stable increase in blood pressure, that is, hypertension.
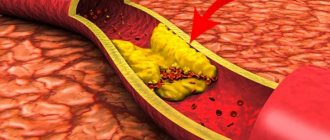
Essentially, retinal angiopathy of the hypertensive type is a complex change in the blood vessels in the fundus: arterioles narrow, and venules and veins, on the contrary, expand and become more tortuous. As a result of this process, the retina does not receive enough nutrients, swells, and pinpoint hemorrhages appear on it. Without timely detection and correction, the disease ends in widespread atrophy or retinal detachment, accompanied by loss of vision.
Causes
Doctors call the main cause of hypertensive retinal angiopathy hypertensive vascular syndrome, in which a high level of tension in the walls of arteries and arterioles remains. As a result of this process, the diameter of their lumen is reduced and, accordingly, the pressure on their walls increases. Arterioles can resist the increased load for some time, and veins stretch and often burst.
The appearance of hypertensive changes in the vessels of the eyes and the body as a whole can be provoked by:
- neurological disorders;
- chronic endocrine diseases - diabetes mellitus, thyroid dysfunction, etc.;
- chronic intoxication of the body due to living in unfavorable environmental conditions, smoking or alcoholism;
- congenital abnormalities in the structure and patency of blood vessels;
- diseases accompanied by increased or unstable intracranial pressure;
- diseases of the blood and hematopoietic system, accompanied by decreased fluidity and increased formation of blood clots;
- chronic diseases of the spine, especially the cervical spine, as well as injuries to the soft tissues of the neck.
Despite the fact that the pathology is caused by various diseases, ophthalmologists cite the patient’s age as the most common cause of hypertensive retinal angiopathy. According to statistics, more than 80% of people with this diagnosis are elderly. Such figures are explained by the fact that a worn-out body is not able to stop the transformation of blood vessels in time, so angiopathy occurs in different parts of the body and organs - weakness of the blood networks.
Important! In most cases, patients with chronic diseases have unilateral angiopathy of the eye vessels. If we are talking about bilateral deterioration of retinal trophism, this may be the consequences of a cervical spine injury.
Preventive measures
You can protect yourself from such a disease - just listen to the following advice and follow them unquestioningly.
- The diet should include vegetables, fruits, fish and dairy products. We exclude fatty and fried foods. Salt is also an enemy, so it is necessary to reduce its amount.
- Bad habits are bad for your health. Alcohol and smoking are prohibited.
- The patient must monitor his mental state, avoid stress, depression, and be sure to follow the correct daily routine. At the request of the patient, the attending physician may prescribe sleeping pills or sedatives.
- If you have a sedentary lifestyle, you need to walk in the fresh air more often, engage in light sports: swimming, walking, physical therapy.
- Even if you don't have diabetes, it's a good idea to check your blood sugar levels daily.
Symptoms and stages of the disease
The manifestation (the first obvious manifestation) of the symptoms of hypertensive retinal angiopathy occurs at the stages of actively developing vascular insufficiency in the fundus. According to statistics from ophthalmologists, in 90% of cases we are talking about irreversible tissue changes in the retinal area. To identify the disease in the early stages, when it does not manifest itself at all or is accompanied by a slight deterioration in vision, doctors pay attention to the following signs:
- regular stable increase in blood pressure;
- complaints of frequent headaches;
- complaints of inability to concentrate on work that requires prolonged eye strain;
- complaints of temporary visual impairment, for example, the inability to focus in the dark or the need to “get used to” bright light for a long time.
In general, retinal angiopathy of the hypertensive type is characterized by clinical similarities with retinal detachment. In this case, the patient may have difficulty recognizing the text due to its blurriness or many dark spots in the field of vision.
The intensity of symptoms depends on the stage of development of the pathology:
- The initial stage is asymptomatic, although vascular changes are already clearly visible when examining the fundus. Only with significant and prolonged strain on the eyes do signs of “visual fatigue” appear - lacrimation, headache localized in the bridge of the nose and forehead, burning sensation.
- The second stage is accompanied by transient symptoms, a significant increase in the venous pattern, retinal edema and the presence of pinpoint hemorrhages. The patient begins to experience mild discomfort in the eyes, headaches, and difficulty with twilight vision.
- At the third stage, the symptoms characteristic of the second stage of disease development intensify. The discomfort becomes longer lasting. During a hypertensive crisis, retinal detachment may occur, accompanied by loss of part of the visual field or complete blindness.
- The fourth and final stage is accompanied by the release of exudate into the cavities adjacent to the retina and the onset of the inflammatory process. The patient's vision drops sharply or disappears if exudate is released into the space between it and the underlying layer. Additionally, intense headaches may occur; in the most severe cases, fever occurs.
Ophthalmologists note that in the early stages of development, hypertensive retinal angiopathy is easier to correct. The earlier the disease is detected and measures to save the retina begin, the higher the chance of saving vision.
Symptoms
Signs and treatment of hypertensive macroangiopathy depend on the main factors in the occurrence of the disease and the condition of the blood vessels in general. The types of damaged vessels are also important. If the disease affects the limbs, the person feels pain, discomfort, swelling and bluish skin. It is even possible to develop gangrene if the vessels become clogged. With macroangiopathy, the patient sometimes limps, and the gait changes.
If the disease affects the brain, then strokes and ischemic attacks occur, from which the brain suffers. Typically, such patients suffer from constant headaches, memory loss, dizziness to the point of fainting, pressure changes and darkening in the eyes. It is important to know that these are signs of hypertensive macroangiopathy.
If the disease affects the heart vessels, then ischemia and then a heart attack may develop. A person suffers from shortness of breath from any physical activity, he suffers from constant pain in the back and chest, feels tired and overwhelmed. The symptoms of the disease worsen if the patient does not take any measures to cure it. Further development of cardiac vascular macroangiopathy threatens myocardial infarction, severe pain and exercise intolerance.
If angiopathy affects the kidneys, then cure is almost impossible. The kidneys begin to suffer from edema, which impairs the electronic and water processes in them. As a result, kidney failure develops. So, we learned what hypertensive macroangiopathy is and the signs (symptoms) of this disease. How to identify it and with what?
Diagnostics
Hypertensive retinal angiopathy is diagnosed during complex therapy. To identify vascular abnormalities, the ophthalmologist only needs to examine the fundus of the eye using the ophthalmochromoscopy method (a method of examining the retina in red and white light) and visualize the signs of the disease:
- expansion of the venous network;
- narrowing of arteries, arterioles and capillaries;
- pinpoint hemorrhages, etc.
To identify the causes of angiopathy, additional diagnostic methods are used:
- Ultrasound of the eye;
- Doppler scanning of the vessels of the retina, head, and, if necessary, neck;
- radiography with contrast;
- MRI of the head.
If hypertensive retinal angiopathy is suspected, a therapist will refer you for examination, an ophthalmologist will monitor the process, and treatment will be prescribed by a therapist, ophthalmologist, and a neurologist and cardiologist.
Our advantages
"Moscow Eye Clinic" offers comprehensive diagnostics and effective treatment of eye diseases. Modern equipment and the high professional level of specialists working in the clinic eliminate diagnostic errors.
Based on the results of the examination, each visitor will be given recommendations on choosing the most effective methods of treating the eye pathologies identified in them.
Author:
Yakovleva Yulia Valerievna 5/5 (1 rating)
Honey. portal:
Treatment methods
Since ocular angiopathy is not an independent disease, for its treatment it is necessary to use two types of therapeutic measures:
- restoration of vascular tone
, strengthening and normalization of blood circulation; - stabilization of blood pressure.
Groups and names of funds aimed at strengthening and restoring eye blood vessels:
- vasodilators;
- agents that improve blood flow;
- vitamins to strengthen blood vessels.
Additionally, local agents Taufon or Quinax are prescribed, which help reduce the load on the eye vessels, reduce the inflammatory process, and improve metabolic processes in the tissues of the visual organs.
Since hypertensive retinal angiopathy is often provoked by high blood pressure, during therapy it is important to use medications to normalize blood pressure:
- beta blockers to maintain blood pressure at a stable level;
- diuretics for emergency reduction of blood pressure during a hypertensive crisis;
- medications that reduce spasm of vascular walls.
Important! Medicines for complex therapy are selected by a doctor. Self-medication with the medications listed above can cause life-threatening complications.
Identification of the disease
The diagnostic process is a comprehensive examination of the patient’s body. This includes blood tests and reactions to treatment, and recording blood pressure numbers. After a detailed examination, it is established that these are signs of hypertensive macroangiopathy, and not another disease.
In case of damage to the vessels of the brain or neck, MRI and ultrasound examination are additionally prescribed. The work of the heart and the state of the vascular system can be studied by ECG, echocardiography, and coronary angiography. The condition of the kidneys is determined by ultrasound and urography.
An important stage of diagnosis is monitoring changes in blood vessels. Correct diagnosis and adequate assessment of existing disorders are the key to prescribing competent treatment. The result largely depends on the diagnosis.
Prevention and prognosis
The prognosis for ocular angiopathy depends entirely on the course of hypertension. Patients who manage to maintain normal blood pressure readings for a long time are not at risk of blindness. Patients facing aggressive forms of hypertension need to prepare for a serious decrease in visual acuity.
There are no specific preventive measures for this disease, because hypertension is often a hereditary disease. To avoid complete loss of vision, people prone to high blood pressure should regularly measure this indicator and take medications prescribed by their doctor. Twice a year they need to be examined by an ophthalmologist, and if signs of angiopathy are detected, follow additional instructions.
General information
Diabetic angiopathy (abbr. DAP ) manifests itself in the form of impaired hemostasis and generalized damage to blood vessels, which are caused by diabetes mellitus and is its complication. If major large vessels are involved in the pathogenesis, then we speak of macroangiopathy , whereas in the case of disruption of the walls of the capillary network - small vessels, pathologies are usually called microangiopathy . Diabetes mellitus today affects more than 5% of the world's population; complications and generalized lesions of the cardiovascular system lead to disability due to the development of blindness, amputation of limbs, and even lead to “sudden death,” most often caused by acute coronary insufficiency or myocardial infarction .
The code for diabetic angiopathy according to ICD-10 is “I79.2. Diabetic peripheral angiopathy", diabetic retinopathy - "H36.0".
Pathogenesis
The pathogenesis is usually based on improper or ineffective treatment of hyperglycemia caused by diabetes mellitus. At the same time, patients develop shifts and severe metabolic disorders not only of carbohydrates, but also of proteins and fats; sharp changes in glucose levels are observed during the day - the difference can be over 6 mmol/l. All this leads to a deterioration in the supply of body tissues with oxygen and nutrients, vascular cells are also involved in pathogenesis, glycosylation of lipoproteins of the vascular wall occurs, deposition of cholesterol, triglycerides, sorbitol , which leads to thickening of the membranes, and glycosylation of proteins increases the immunogenicity of the vascular wall. Thus, the progression of atherosclerotic processes narrows blood vessels and disrupts blood flow in the capillary network. In addition, the permeability of the blood-retinal barrier increases and the inflammatory process develops in response to advanced glycation end products. The adverse effects are enhanced by hormonal imbalances - increased secretion of fluctuations in the bloodstream of somatotropic and adrenocorticotropic hormone , cortisol , aldosterone and catecholamines .
The process of development of angiopathy in diabetes is considered insufficiently studied, but it has been established that it usually begins with vasodilation and increased blood flow, resulting in damage to the endothelial layer and blockage of capillaries. Degenerative and disorganization processes, increased permeability of the vascular wall, impaired reactivity of autoregulatory function cause disruption of protective barriers and lead to the formation of microaneurysms , arteriovenous shunts , and causes neovascularization . Damage to the walls of blood vessels and microcirculation disorders are ultimately expressed in the form of hemorrhages.