Infographics for the “bio/mol/text” competition: A clinical blood test is the most common laboratory test prescribed by a doctor when we come to an appointment and complain of feeling unwell. “Blood from a finger, tomorrow from 8:00 to 9:30, on an empty stomach, Nth office,” several generations have invariably heard this phrase. However, blood testing technology has undergone great changes in recent decades and has moved from manual methods to automatic ones. Let's figure out how your grandmother's blood was analyzed and why things are done differently now.
Competition "bio/mol/text"-2019
This work was published in the category “Visually about the beloved” of the “bio/mol/text” competition-2019.
The general sponsor of the competition and partner of the Skoltech nomination is the Skoltech Center for Life Sciences.
Competition sponsor: the largest supplier of equipment, reagents and consumables for biological research and production.
The audience award was sponsored by BioVitrum.
"Book" sponsor of the competition - "Alpina Non-Fiction"
What will we explore?
Blood is a liquid connective tissue of the body, consisting of plasma and three types of formed elements: red blood cells, platelets and leukocytes. Leukocytes, in turn, come with granules in the cytoplasm - these are neutrophils, eosinophils and basophils - and without granules - lymphocytes and monocytes. In order to distinguish pathology from the norm, you need to know what the concentration of blood cells is, what they look like and what function they perform. It's time to remember who we are dealing with.
Figure 1. Formed elements of blood [1–3]
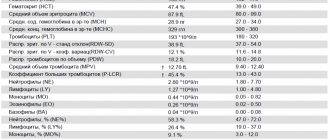
Figure 2. The figure shows: the concentrations of blood cells are normal; leukocyte formula - the percentage of different types of leukocytes in the blood; erythrocyte sedimentation rate; hemoglobin concentration; hematocrit is normal [4].
So, experts analyze the relative and absolute content of cells, their morphological characteristics, distribution over blood volume and many other parameters. These indicators can tell whether cells are able to fully perform their functions, and if not, then indicate the reason for their “inoperability” and serve as the basis for making a diagnosis.
Figure 3. Blood testing: then and now
1.Blood and blood functions
Blood
- This is one of the body’s liquid media, continuously circulating through the system of blood vessels and capillaries. The functions of blood are very important and varied. Blood delivers oxygen and nutrients to all organs and tissues, participates in maintaining immunity to various infections, removes harmful metabolic products from tissues, carries enzymes, hormones, and other substances that give a signal to start certain processes in the body.
Since blood is involved in all processes occurring in different organs and systems of the body, its composition is very variable under the influence of substances received or released into the blood. Healthy blood, “serving” the diseased organ, receives from it a kind of information about the quality and degree of disorders. During positive events in the human body (for example, the production of sex hormones, endorphins), the resulting substances enter the brain with the blood, which commands the organs and systems to most effectively participate in processes beneficial to the body.
Forward to the past!
1965, 8 am, there is a line for tests at the local clinic. Your grandmother donated blood, and the laboratory assistant takes a number of test tubes for testing. Let's follow him to the laboratory and see what's there and how. In the laboratory we see doctors bending over microscopes or working with test tubes. It is no exaggeration to say that in your grandmother’s youth, a specialist’s eye and a microscope were the main tools for blood analysis. The following basic characteristics of blood are determined: the concentration of each type of formed element, the number of different types of leukocytes, the erythrocyte sedimentation rate and the concentration of hemoglobin. In addition, the specialist calculates the hematocrit - the ratio of the volume of red blood cells to the total volume of blood [5].
Calculate in order!
The first step is to count the cells and determine their concentration in the blood. The counting of red blood cells, leukocytes and platelets is carried out in the Goryaev chamber, named after its inventor. Goryaev’s chamber is a glass with a recess and a mesh applied, into which a drop of blood diluted in saline solution is placed. To determine the number of formed elements, the camera is placed under a microscope and the cells located in large and small grid squares are counted. Each type of cell has its own counting rules and formula by which their initial concentration is calculated, taking into account blood dilution and the number of grid squares [6]. Changes in the number of formed elements serve as an important criterion for the diagnosis of anemia, inflammatory and viral diseases, disorders of the blood coagulation system and other pathological conditions [7].
Who are you?
Another stage of blood testing is the differentiation of leukocytes into populations. Special attention is paid to it: a change in the concentration of a certain type of cell indicates a specific pathology. Bacterial infection, viruses or allergies? Leukocytes will tell you what diagnosis to make and what treatment to prescribe. The distinction of leukocytes is trusted only to a highly qualified specialist. To begin with, a blood smear is fixed in alcohol and stained using the Romanovsky-Giemsa method. The composition of the dye is selected in such a way that different cell structures are painted in different colors. Coloring depends on the ability of the components of the color mixture to bind to structures containing acids or bases. For example, hemoglobin and eosinophil granules acquire a red-pink color due to eosin, and the nuclei of formed elements and basophil granules (having an affinity for bases) are stained with methylene blue and blue [1]. When the smear is ready, a specialist examines it under a microscope and determines by its appearance what type of different cells they belong to [8]. The presence of colored granules, features of the shape of the nucleus, cell size - all parameters must be kept in mind for error-free classification. Typically, one hundred leukocytes were counted, followed by calculation of the percentage, and in order to avoid confusion, an 11-key counter was used [9]. If you see a cell under a microscope, press the key indicating the cell of this type, and at the end of the count, the number of leukocytes of each type will be displayed on the counter screen [10].
Precipitated
Another characteristic of clinical significance is the erythrocyte sedimentation rate (ESR). This is an indicator that evaluates the rate of separation of blood into plasma and formed elements. What is the reason for this division? Macromolecules found in blood plasma can simultaneously bind two red blood cells to each other, resulting in the formation of “coin columns” [11]. Such complexes, under the influence of gravity, settle to the bottom of the test tube, leaving a layer of transparent plasma above them - this is called erythrocyte sedimentation. An increase in erythrocyte sedimentation rate indicates pathological processes occurring in the body, such as inflammatory, infectious or oncological diseases [12].
To determine ESR, the Westergren method received worldwide recognition, but the Panchenkov method was also widespread in Russia. The operating principle of the methods is the same, only the types of tubes used differ. The blood is mixed with an anticoagulant - sodium citrate - and placed in a capillary - a thin glass tube. Red blood cells settle to the bottom of the tube within an hour, and then the height of the plasma column formed on top is measured [13]. In this way, the erythrocyte sedimentation rate is obtained, expressed in mm/h.
Taste and color
Hemoglobin is the red pigment of red blood cells that binds and transports oxygen and carbon dioxide. A decrease in hemoglobin content in red blood cells is the cause of anemia that accompanies a number of diseases. Hemoglobin concentration is determined visually using a Sali hemometer. The device looks like this: in the center is a test tube for the blood being analyzed, and on the sides are colored reference tubes. The laboratory technician adds hydrochloric acid to the blood being studied - hemoglobin turns into brown hemin. Then the blood is diluted with distilled water until its color (in the subjective opinion of the laboratory assistant!) matches the color of the standard. The liquid level obtained in the central tube corresponds to the hemoglobin concentration [14].
As you may have guessed, 50 years ago it was very easy to make a mistake when testing blood. Incorrect identification of the type of leukocyte or failure to count the formed elements - all this led to inaccurate analysis results. What has been done to prevent errors? Let's go back to our time and find out how blood is studied today.
2.General blood test
A general blood test is a very important and informative examination. Based on its results, without resorting to other types of examination, doctors of many specialties can already make a preliminary diagnosis, which is then only confirmed by subsequent diagnostics.
To donate blood for a general analysis, no special preparation is required, however, the most accurate readings will be the blood test that the patient took in the morning on an empty stomach. Blood is most often taken from the capillaries of a finger or from a vein in the bend of the elbow.
The blood taken for analysis is subjected to several studies, then the doctor must decipher the blood test (compare the data obtained with normal values).
Times change
Changes are visible already at the stage of blood sampling: if previously the doctor collected blood in several test tubes with reagents, a glass capillary and made a smear on the glass, now very small volumes are used - from 12 to 150 μl [15] of blood is enough to examine it for all parameters.
Let's take a look into a modern hematology laboratory. Wow! Everything is cluttered with equipment, and the laboratory assistant is nowhere to be seen... Maybe he went off to make himself some coffee? He won't make it in time! The blood test will be ready in a minute, and the device will give the result in the form of a paper tape with numbers and abbreviations, behind which all sorts of parameters are hidden.
Modern hemoanalyzers are divided into several classes, depending on what they can do. Each subsequent class is a new stage of evolution - faster, more accurate, more perfect. The use of a combination of technologies works wonders: if the first analyzers could determine eight blood parameters and did not distinguish between types of leukocytes [16], then the latest devices are able to differentiate up to seven populations of leukocytes [17] and in total examine more than 40 blood characteristics.
As Arthur C. Clarke said, “Any sufficiently advanced technology is indistinguishable from magic.” Indeed, the most detailed results in such a short period of time cannot but surprise. But all magic is based on physical laws. And although names like electrical impedance, light scattering and photometry are a little intimidating at first glance, now we will understand what principles underlie each analysis technology.
Population census
In the middle of the last century, Wallace Coulter made a revolution by patenting the technology of automatic cell counting. One of the leaders in the production of hematology analyzers, the Beckman Coulter company, is named after him [18]. The aperture-impedance method (or Coulter method) is based on the registration and analysis of impulses that occur when a cell passes through an aperture from one container to another, each of which contains an electrode. When there is no cell in the hole, current flows freely through the electrolyte between the electrodes under the influence of an electric field. To direct the cells to the aperture, a pump is used that pumps out liquid from one container, and the formed elements rush into it. Passing through the aperture, the cell displaces a volume of electrolyte equal to its volume from one container to another. In this case, a pulsed change in resistance (impedance) occurs - the cell membrane creates an obstacle to the free flow of current. At the same time, the current strength recorded by the meter also changes. The number of generated impulses corresponds to the number of formed elements, and the height of the impulse is proportional to the volume of the cell [19]. Using information about the number and volume of formed elements, the device can calculate hematocrit, the average concentration of hemoglobin in an erythrocyte, the width of the distribution of cells by volume and many other parameters [15].
Divide and rule
Differentiation of leukocytes into populations can be carried out using a Coulter counter, but a problem arises - different types of leukocytes are similar in volume and similar pulse amplitude does not always allow one to accurately determine the cell type. What should I do? To solve this problem, combinations of reagents are selected that change the size of cells to varying degrees so that it becomes possible to separate them [15].
But the most common method of differentiation is flow cytometry [20]. The method works as follows: cells in the flow are alternately irradiated with a laser, and the resulting light scattering and fluorescence signals are recorded by detectors and analyzed. In order to correctly determine membership in a population, several parameters are examined at once. Thus, light scattering at a small angle provides information about the relative size of cells, and light scattering at a right angle allows you to “look” inside the cell and study its internal structure - the presence of granules and the shape of the nucleus. Another parameter - fluorescence - can tell about the number of antigens and their appearance on the surface of cells - this cannot be accurately determined by eye. Unlike manual differentiation methods, not 100–200 cells are analyzed, but tens of thousands per second! And each leukocyte receives an individual approach: hydrodynamic focusing ensures that the cells line up in a row and are irradiated one by one in the flow cell. The result of the count appears on the screen in the form of scatter diagrams, where cells with similar properties form clusters.
Precipitated: 2.0
Modern instruments can measure ESR in two fundamentally different ways. The first is the modified Westergren method. The principle of operation has not changed since your grandmother's time, but due to automation it has become faster and more accurate. The second is measuring the kinetics of erythrocyte aggregation using an optical method [21]. It happens like this: an anticoagulant is added to the blood, the tubes with blood are placed in a rotor, where automatic mixing occurs. After this, the analyzer takes part of the blood into a microcapillary, where it accelerates and abruptly stops (the so-called “stopped stream” method). The stop causes aggregation of red blood cells, and at this moment the optical density of the blood is determined using a photometer - the denser the red blood cells are located, the less light will pass through the sample. The device uses the data obtained and builds a sedimentation curve - its analysis will allow you to present the result in the usual units of ESR measurement [22], [23].
Photo for memory
To determine hemoglobin concentration, the International Committee for Standardization in Hematology recommends the methemoglobin-cyanide method. However, a different test that does not use toxic cyanide is now widely used. Meet the SLS method. It is named after the main reagent - sodium laurithyl sulfate. SLS destroys red blood cell membranes, after which it binds to heme groups and forms stable complex compounds. They are analyzed photometrically - laser light is passed through the blood sample. Complex compounds absorb part of the light, as a result of which the intensity of the output light flux weakens. Attenuation is measured using a photosensor and the resulting data is converted into hemoglobin concentration units [24].
How to donate blood from a fingertip
There are general rules for donating blood from a finger prick that must be followed in order for the CBC result to be reliable:
- The analysis is taken in the morning, on an empty stomach - at least 8-12 hours must pass after the last meal.
- Two days before the procedure, you need to exclude fatty and fried foods, smoked foods, and alcohol from the menu.
- During the day before the analysis, it is necessary to minimize physical activity - hard work, intense training.
- There is no need to worry before donating blood from your finger; smoking is strictly not recommended.
Blood is usually taken from the ring finger of the left hand. If there are bruises, wounds, thermal damage (burn, frostbite), swelling, cyanosis, blood is taken from any other finger. Hands should be warm. If the hands are cold or the patient has low blood pressure, blood will not flow well. In such cases, before the analysis, it is recommended to hold your hand for some time under warm water or wrap it in a heated towel, and gently massage your finger before puncture.
After drawing blood, the fingertip is treated with an antiseptic solution and a sterile cotton swab is applied to it until the bleeding stops completely.