High cardiovascular risk: main components
Lecture transcript
XXV All-Russian Educational Internet Session for doctors
Total duration: 29:10
00:00
Oksana Mikhailovna Drapkina, Secretary of the Interdepartmental Scientific Council on Therapy of the Russian Academy of Medical Sciences, Doctor of Medical Sciences, Professor:
- We continue. Next lecture of the master class. It will be read by Doctor of Medical Sciences Igor Vladimirovich Sergienko. "Cardiovascular risk stratification." Please.
Igor Vladimirovich Sergienko, Doctor of Medical Sciences:
— Dear Vladimir Trofimovich, Oksana Mikhailovna, thank you for your introduction.
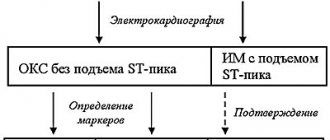
We currently use two risk stratification systems. These are the SCORE system and the Framingham scale. However, you all know that these risk stratification systems have certain disadvantages. What do these scales take into account? What do we consider when using the SCORE risk stratification scale?
We take into account the patient's gender. We take his age into account. We take into account whether the patient smokes or not. Of course, we take into account the level of blood pressure. What is very important is to take into account your cholesterol level. As soon as this system appeared, doctors (ordinary therapists) immediately began to ask questions: does the system work or not for patients with diabetes? If a patient (I know for sure) has atherosclerosis, and the SCORE scale shows a low risk, what then should be done?
We realized that this system is not entirely perfect, and that it needs to be improved and optimized.
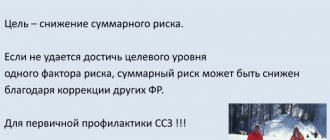
At the moment, for risk stratification, risk factors are used, which can be divided into, you know, large (or classical) and new (or non-classical).
Large ones are the patient’s age and gender, family history, arterial hypertension, dyslipidemia, diabetes mellitus, smoking, obesity (at the moment, waist circumference rather than body mass index is used), physical inactivity and an atherogenic diet.
However, now new or non-classical risk factors are becoming very important, which can be divided into lipid, non-lipid and subclinical atherosclerosis, which we will talk about today. It should be noted that non-classical risk factors (for example, low LpA) can already be considered classical.
02:23
What risk factors does the European Society of Cardiology and the Russian Society for the Study of Arterial Hypertension recommend that we use? This is the value of pulse pressure. This is age. This is smoking. This is dyslipidemia. This is the change in fasting plasma glucose. Impaired glucose tolerance. Unfavorable family history. Abdominal obesity.
On the slide you see the risk stratification that the Russian Society for the Study of Arterial Hypertension proposed to use in 2010. What is very important? We focus not only on the level of arterial hypertension (that is, pressure numbers), but also look at whether the patient has risk factors, target organ damage, diabetes mellitus and so-called associated conditions.
If you look, you will see that even in patients with a slight increase in blood pressure, if there are three or more risk factors, or if the patient has end-organ damage, or if the patient has diabetes mellitus, then we immediately classify this patient as at least into the high additional risk category. If the patient has previously suffered a heart attack or stroke, then it no longer matters what his blood pressure level is. This is already a very high risk patient.
This is very good, it should be used, but the slide shows the Federal Register of Arterial Hypertension for 2009. It shows the frequency of assessment of risk factors for cardiovascular diseases and target organ damage in real outpatient practice. What do we see? Risk factors for cardiovascular diseases are taken into account by 9% of doctors, and target organ damage by 13% of doctors. We see that the system in real practice does not work as well as we would like.
What methods does a doctor use when a patient comes to him to determine his risk? This is data from a survey and physical examination. He will talk with the patient, find out whether his relatives were sick, determine gender, height, measure body mass index or waist circumference, and ask if the patient smokes. In the best case, the doctor will have a biochemical blood test in front of him and can even see the patient’s lipid spectrum. All. This will already give the doctor the opportunity to stratify the risk.
05:09
Is it correct? Why do we not take into account the results obtained using instrumental methods? For example, 10 years ago it was probably not necessary to talk about duplex examination of the carotid arteries in widespread practice for risk stratification. But now the devices are available in many medical institutions.
The slide presents a rather interesting study that lasted three years. It took place in the USA. We looked at the incidence of complications of coronary disease in patients with different levels of initial risk. Conventionally, they can be divided into conditional risk, low and moderate risk. We see that in patients whose risk was determined to be low, the incidence of complications was 75%, and in patients whose risk was determined to be high, it was 12%.
What is it? It turns out that we have identified the risk incorrectly. This is partly explained by the “Glagov” phenomenon (Professor Arutyunov spoke well about it today). It turned out that in 60-70% acute coronary syndrome develops with angiographically slightly altered arteries of the heart (coronary arteries).
Why? When an atherosclerotic plaque appears, the vessel begins to remodel. This is aimed at maintaining its lumen. This situation may last for a long time. The plaque volume in this patient may not be different from the plaque volume in a patient who significantly stenoses the coronary artery. But this patient may also experience tearing, rupture of the fibrous capsule, and thrombosis. This patient's risk of developing a myocardial infarction is no less than that of a patient with significant coronary artery disease.
But we will actively treat a patient with significant damage to the coronary arteries and prescribe medications. If we see, let’s say, uneven contours during coronary angiography, we may not prescribe any medications to the patient, thereby sharply increasing the likelihood of him developing some adverse cardiovascular events. We understand that a search for new risk criteria is needed.
The slide presents an interesting study that included 222 patients who had previously suffered a myocardial infarction. These are men and women of the middle age group. In these patients, the first diagnosis was myocardial infarction. These patients and the doctors who had previously seen them did not know that the patients had coronary heart disease.
07:54
Seventy percent of these patients had a low risk of developing coronary heart disease according to the Framingham risk scale. Moreover. Already when it became known that the patients had suffered a myocardial infarction, the risk in these patients was re-evaluated, including using lipid profile data. It turned out that 75% of these patients according to this risk stratification do not need to take any medications.
What factors are now mainly considered as candidates for inclusion in a risk stratification system? These are heredity and genetic markers. These are biochemical markers of inflammation. If I think everyone knows about high-sensitivity C-reactive protein, then maybe not everyone knows about lipoprotein-associated phospholipase A2.
I would like to draw your attention to the fact that there are different types of phospholipases – there are several of them. We know, for example, secretory phospholipase, there is LpA-small associated phospholipase A2. However, there is a separate protein - this is LP FLP A2. It is considered as a possible marker of atherosclerotic plaque instability.
It is believed that if its level is elevated, then the patient most likely has an unstable plaque. It is urgent to take measures to stabilize it. I must say that in Israel this marker is already used as a standard screening method. A patient with ABS comes for examination. They suggest to him - would you like to see if you have an unstable atherosclerotic plaque? To do this, you need to conduct this analysis.
Maybe they are getting a little ahead of themselves. This protein still needs to be studied, but we see that we will be able to diagnose unstable atherosclerotic plaque in the future.
We must take into account signs of organic vascular damage, and we can take this into account at the moment. This is, first of all, preclinical atherosclerosis, that is, thickening of IMT, the presence of atherosclerotic plaques. An increase in the stiffness of elastic vessels, which we can determine by an increase in the speed of the pulse wave. This is the ankle-brachial index, which is very easy for any doctor to measure with only an ankle tonometer. This is the level of coronary calcium, which is not very easy to measure.
10:19
The slide shows the 2010 recommendations of the American Heart Association. They can be used to identify additional cardiovascular risk criteria in asymptomatic patients with respect to atherosclerosis. We see that this is a family history in the first place, and the class of evidence is one (very high). Genetic studies show only third class evidence.
Thickening of the MI complex in high-risk patients is class IIa evidence. This is the ankle-brachial index, this is the pulse wave velocity, this is the coronary calcium index, the level of evidence of which varies depending on the risk determined by the Framingham scale. This is the level of C-reactive protein, this is the level of lipoprotein-associated phospholipase A2.
A very interesting SHAPE algorithm was also proposed to clarify the risk in men over 45 years of age and in women over 55 years of age, in whom the risk was initially determined to be low or moderate. This is the so-called test for preclinical atherosclerosis. The test can be considered negative or positive.
What is a test for preclinical atherosclerosis? This is a multispiral computed tomography to assess the coronary calcium index and a duplex study of the carotid arteries, which takes into account the thickness of the MI complex, as well as the presence or absence of an atherosclerotic plaque.
We see that if the test is negative, then the patient remains in the low to moderate risk group. However, if the test is positive, the patient immediately moves into at least the moderately high risk category. Next, we look at what specific values were obtained from the patient during the examination. We focus specifically on the numbers, on the quantitative determination of the coronary calcium index, the quantitative assessment of the thickness of the MI complex and whether atherosclerotic plaques significantly narrow the arteries or not.
We see that if the plaques narrow by more than 50%, then the patient already falls into the very high risk category. But this is not something abstract that we wrote to the patient and forgot about it. No. When we classify a patient into one category or another, we must achieve target levels of cholesterol or low-density protein. The doses of drugs and the drugs we use will be different. This is our strategy for treating the patient.
12:58
The slide presents the prognostic significance of the thickness of the MI complex in different parts of the arterial bed for the diagnosis of stenotic atherosclerosis of the coronary arteries. We looked at which arteries are best examined with ultrasound, so that these values can be used for risk stratification.
We see on the slide in green that the best vascular basin is the carotid artery basin, since the sensitivity and specificity are higher here. It is best to look at the carotid arteries.
The CAFES-CAVE study is presented in a slide that shows the likelihood of developing cardiovascular complications in patients whose baseline risk is determined to be low, depending on what we find on the carotid duplex study. We see that if we find a completely normal picture, then the risk will be minimal.
Increasing the thickness of the MI complex slightly increases the risk of complications. The presence of an atherosclerotic plaque without stenosis increases the risk by almost 40%. The presence of a plaque that significantly stenoses the lumen of the carotid artery increases the risk by 80%, that is, it completely changes our understanding of the patient.
The slide also shows the relative risk of development in individuals who do not have complaints, depending on physical and instrumental examination. In first place is the positive stress test. If, during a stress test, we see data in a patient that indicates myocardial ischemia, most likely he will have damage to the coronary arteries. However, we see that if we listen to a bruit on the femoral artery in a patient or identify atherosclerotic plaque in the carotid or femoral artery, then that patient also has a high probability of coronary artery disease.
15:04
The thickness of the “intima-media” complex as a risk factor, that is, how can this be displayed quantitatively? Quantitatively, we can display this as follows. An increase in the thickness of the MI complex by 0.2 millimeters increases the risk of developing myocardial infarction by 33% (by a third), and stroke by 28%.
A meta-analysis of 8 studies was also conducted, which showed that each increase in the thickness of the MI complex by 0.1 millimeter increases the risk of myocardial infarction from 10% to 15%, and stroke from 13% to 18%. We have no right to ignore this indicator.
LP FLPA A2 as a risk factor for complications. What? Coronary heart disease, stroke, death from cardiovascular causes and death not related to cardiovascular causes. We see the relative risk assessment. In all cases, LP FLPA A2 plays an important role. We should, in theory, take its level into account when we stratify a patient's risk.
How can we take this into account? We have to measure the patient's phospholipase A2 level and see if it is more than 200 nanograms per milliliter, then the moderate-risk patient will move into the high-risk group. If a high-risk patient has more than 200 nanograms per milliliter, then that patient goes straight into the very high-risk category. I once again emphasize that it will not just be a formal transition, but we must change our therapy.
Allow me to report the results of our research, which was carried out in our medical institution - the Russian Cardiology Research and Production Complex - together with 12 clinics in the Western Administrative District of Moscow. It included 2400 patients. These patients were divided into three groups. Group one is healthy people who have less than two risk factors. The second group is patients with risk factors who have more than two risk factors. The third group is patients who have coronary heart disease.
17:25
What did we get? As would be expected, in patients with coronary heart disease, the level of LP FLPA A2 was the highest. In healthy individuals (group one) it was the smallest. Pulse wave speed. Here we got results that were not entirely clear to us at first. We see that in patients with coronary artery disease, the pulse wave speed is in the middle, and the highest pulse wave speed is found in patients with high risk.
Why is this happening? We had the right to expect something different, however, after analyzing how these patients were treated, what treatment was prescribed to them, we saw that patients who have coronary heart disease took medications. In particular, it was mainly a combination of Diroton and Amlodipine. Some used this combination, some used the equator drug right away, which, as you know, consists of amlodipine and diroton.
In patients, we reduced the pulse wave speed in this way. It became closer to the indicators of healthy individuals. This, colleagues, is very important. This shows that we treat patients who have coronary heart disease correctly and treat them well. But we do not pay any attention at all, excuse the vulgarity, to patients who have a high risk of developing cardiovascular diseases, but who do not yet have them.
We are talking in this case about primary prevention, although, as you know, Professor Nelson said that there is no primary prevention. When we treat a patient, this is always secondary prevention. In this case he is right. We are already beginning to treat subclinical atherosclerosis. We must do this.
Oksana Drapkina : I would like to ask. The question is practical. This combination - an ACE inhibitor and a calcium blocker - in clinical practice, it suggested itself. Then - if we remember this octagon, hexagon, then the triangle of rational antihypertensive therapy, then the lines were always not dotted, but solid, connecting ACE inhibitors and calcium blockers.
In my opinion, it is very successful to combine Amlodipine, a rather powerful drug in terms of lowering blood pressure, and plus lisinopril. Indeed, the experiment proved some antiatherogenic effects of amlodipine. Vascular cell proliferation decreased and endothelial function improved.
You talked about pulse wave speed. Calcium blockers are the drugs of choice. For example, for elderly patients with isolated systolic hypertension. This is a pretty successful combination (I just want to share), which is in one tablet (fixed combination), of course, it greatly helps us retain patients and maintain their compliance. Do you feel this too in the clinic?
20:44
Igor Sergienko : Of course. Clinic doctors - local therapists - are advanced doctors. Don't underestimate it at all. Without our help, they treated patients correctly and correctly, if I can, of course, evaluate the results of their work.
We see very concrete results. We see that the people for whom they made efforts, who were prescribed the drug... I very much agree with compliance, because when several tablets are prescribed, we know that some patients refuse. Moreover, one visit to the clinic, and after that...
When the patient is with us, it’s easier for us (in the hospital). We can prescribe several medications, the patient can take them and feel better during hospitalization. Then he won’t refuse. The patient came here once. Okay, he came to the appointment twice. He needs to be prescribed the drug immediately. Equator was prescribed, the patient began taking it and felt better. When we inform him of the results we get...
Oksana Drapkina : About the forecast.
Igor Sergienko : About the forecast. Here the patient, of course, will not refuse this drug.
Oksana Drapkina : About its metabolic neutrality, because hypertensive people in our country, in general, are obese.
Igor Sergienko : Yes, as a rule.
Oksana Drapkina : You especially showed a picture with a high risk - it’s quite difficult. Sorry for the interruption!
21:59
Igor Sergienko : No, no. Thank you. On the contrary, it's very nice.
Oksana Drapkina : Please, continue.
Igor Sergienko : The value of the coronary calcium index. Everything is clear here. In patients with coronary heart disease it is higher than in other groups. This is completely understandable: calcium is deposited, and, unfortunately, we cannot dissolve it with any medications.
Very interesting slide. Duplex study of the carotid arteries in patients with low and moderate risk. What does it mean? Roughly speaking, this patient came to close his sick leave for ARVI, for example. He was asked to participate in our study. The patient agreed. He underwent a duplex study of the carotid arteries.
We see that only 40% of women and 30% of men have arteries without atherosclerotic plaques. However, 20% of men have two atherosclerotic plaques in the carotid arteries, and 16% have four. These are people who considered themselves and whom doctors considered to be completely healthy, without, of course, prescribing anything to them. We see on the slide what kind of picture they have, however. The patients were clearly not thoroughly examined.
The slide also shows low- and moderate-risk women. The frequency of detection of atherosclerotic plaque depending on age and the presence or absence of arterial hypertension is shown. We, of course, see that in patients with arterial hypertension, the likelihood of identifying atherosclerotic plaque in the carotid arteries is higher than in patients without arterial hypertension. This is completely understandable.
We also see the distribution by age: in patients of an older age group, the likelihood of detecting plaques is increased compared to patients of average age and women under 45 years old, because I cannot say that this is a younger age group.
This allowed us to draw an interim conclusion from our study. Women over 55 years of age, regardless of the presence or absence of arterial hypertension, should undergo a duplex examination of the carotid arteries in all cases.
24:07
The presence of arterial hypertension increases the likelihood of detecting an atherosclerotic plaque, but its absence does not at all exclude a significant likelihood of the presence of an atherosclerotic plaque in women with low and moderate risk. We set a task - to find criteria for an increased likelihood of the presence of atherosclerotic plaques in the carotid arteries in women who initially have a low or moderate risk.
We searched for differences in the studied parameters in women with low and moderate risk under the age of 45 years without arterial hypertension, and did not find significant differences. The same is true for women under 45 years of age, but with arterial hypertension. Also, no significant differences were found.
This allowed us to make an interim conclusion that in women with low and moderate risk under the age of 45, without taking into account the presence of arterial hypertension, it is not advisable to conduct a duplex examination of the carotid arteries as a screening method.
What about the 45-55 age group? We assessed the likelihood of having an atherosclerotic plaque in this age group, regardless of blood pressure level. They showed that there is a relationship with body mass index, with uric acid levels greater than 260 µmol/liter, and with PL A2 levels greater than 315 ng/ml. With these indicators, the likelihood of having an atherosclerotic plaque in this age category of women is higher.
We concluded that in women 45-55 years old, regardless of the presence of arterial hypertension, it is advisable to conduct a duplex study of the carotid arteries when the BMI is more than 30 or the uric acid level is more than 260. We do not take into account the FL level for now, since this indicator is not determined everywhere. Rather, this is an exception for now.
26:13
A study of low- and moderate-risk men found that men under 40 years of age had the same findings as a subgroup of women under 45 years of age, and men over 50 years of age had the same findings as women over 55 years of age.
Let me not repeat the same calculations, not show the same slides, but simply make an intermediate conclusion that it is always advisable for men over 50 years old to conduct a duplex study. For men under 40 years of age, duplex examination of the carotid arteries is not advisable. I mean, of course, only as a screening.
What happens in the middle age category among men aged 40-50 years with a moderate initial risk? We have shown that the likelihood of detecting an atherosclerotic plaque is associated with the presence of metabolic syndrome and a uric acid level greater than 350 µmol/liter.
An interim conclusion was made that men aged 40 to 50 years, regardless of blood pressure, should undergo a duplex examination of the carotid arteries if they have metabolic syndrome or a uric acid level of more than 350 µmol/liter.
The slide shows the algorithm that we developed after conducting this research. The research is ongoing. It will end at the beginning of 2012, but for now we can propose an algorithm of indications for duplex examination of men and women of low and moderate risk in various age categories.
Let me present a potential algorithm for moving men and women at low and moderate SCORE risk to high risk.
So, if we have a woman over 45 years of age or a man over 40 years of age, and they have a blood pressure of 130-139 systolic and 85-80 diastolic, or if patients are taking antihypertensive drugs and it doesn’t matter what their blood pressure is if we If we find an atherosclerotic plaque in these patients (I repeat, it does not matter whether it significantly or insignificantly narrows the lumen), then these patients can immediately be included in the high-risk category.
For the third time, I draw your attention to the fact that they are not only classified as high risk, but we are obliged to change their treatment.
28:40
The objectives of the next stage of the examination will be to study the growth rate of atherosclerotic plaque in the carotid arteries. Study of the prognostic significance of the number of atherosclerotic plaques in the carotid arteries, since we have not yet taken this into account. Of course, the search for markers of instability of the atherosclerotic plaque, which, it seems to me, would be very promising with LP PLA A2.
I would like to thank 70 local therapists in 12 clinics in the Western Administrative Circle of Moscow for this study.
Thank you.
29:10
Causes of the disease
Arterial hypertension is a disorder of the cardiovascular system, characterized by an increase in systolic blood pressure (the first digit on the tonometer) above 140 mm Hg.
Art. and/or diastolic (second digit) – above 90 mm Hg. Art. It can occur as an independent disease or result from another pathology. The most common is hypertension or essential hypertension, which develops independently, without obvious reasons. It occurs in 90% of patients with high blood pressure.1
Secondary or symptomatic hypertension is directly related to other diseases or factors that can be controlled.1 This form of the disease is usually suspected in young people under 30 years of age with high blood pressure.
The main causes of secondary arterial hypertension are2:
- Obstructive sleep apnea syndrome.
- Kidney diseases.
- Neoplasms of the adrenal glands – pheochromocytoma.
- Pathologies of the thyroid gland: thyrotoxicosis, hypothyroidism.
- Congenital abnormalities of the heart and blood vessels, including coarctation of the aorta.
- Primary hyperaldosteronism.
- Itsenko-Cushing syndrome.
- Side effects of medications such as: oral contraceptives, non-steroidal anti-inflammatory drugs, antiviral drugs.
Risk factors
There are a number of factors that increase the likelihood of developing hypertension. The most significant include:
- Age. The risk of high blood pressure increases with age, mainly after age 65.
- Hereditary tendency to arterial hypertension.
- Overweight.
- Physical inactivity, lack of physical activity.
- Smoking, including passive smoking.
- Excess salt and potassium-containing foods in the diet.
- Alcohol abuse.
- Chronic stress, frequent emotional stress and lack of sleep.
- Pregnancy.
- Early menopause.
- Heart rate exceeding 80 beats/min at rest.
Modern diagnostic methods
24-hour blood pressure monitoring can help diagnose hypertension.
Photo: Minaart / Depositphotos The diagnosis is often made based on blood pressure readings obtained from tonometry and patient interview data.
In order to identify potential causes, as well as to assess risks to human health and select the most appropriate treatment regimen, a number of laboratory and instrumental studies are additionally carried out.
The examination program for a patient with arterial hypertension includes:
- Laboratory tests. This includes routine general blood and urine tests, as well as determination of a number of biochemical parameters, including: blood glucose, uric acid, sodium and potassium levels, total cholesterol and high and low density lipoproteins (HDL-C, LDL-C), serum creatinine blood followed by calculation of glomerular filtration rate (GFR).1
- Instrumental diagnostics. For patients with newly diagnosed arterial hypertension, in order to exclude white coat hypertension (increased pressure as a result of fear or “tremor” in front of the doctor), 24-hour blood pressure monitoring with simultaneous recording of an electrocardiogram (ECG) according to Holter is recommended. Also, if necessary, ECHO-CG, ultrasound diagnostics of the kidneys, duplex scanning of the vessels of the kidneys, head and neck, fundus examination (ophthalmoscopy), computed tomography or magnetic resonance imaging (CT or MRI) of the brain are performed.1
Folk remedies against hypertension
Ginger tea is beneficial for people with high blood pressure.
Photo: jcomp - ru.freepik.com In addition to drug therapy, traditional methods of treatment can be effective adjuncts. They include a variety of tinctures and decoctions from various plants, roots, leaves or berries. The following have a proven antihypertensive effect:
- Ginger tea.
- Ginseng infusions and teas.
- Foot compresses with apple cider vinegar.
- Decoctions with sunflower seeds.
- Pomegranate juice.
- Dark chocolate (containing at least 60-70% cocoa, in moderation) and cocoa.
- Celery juice.
- Garlic.
- White mistletoe decoction.
- Dietary supplements or foods that increase nitric oxide or dilate blood vessels (vasodilators), such as: cocoa, coenzyme Q10, L-arginine.
- Omega-3 fatty acids found in oily fish, high fish oil supplements and flax seeds.
Various procedures can also help reduce high blood pressure, including massage courses for the back and collar area, contrasting water procedures for the feet and hands, etc.5, 6
Important! Traditional medicine cannot be the only method of treatment. Also, many medicinal plants contain biologically active substances that can cause adverse reactions. Therefore, before using them, you should definitely consult a doctor.
Symptoms of stage 1 hypertension
Clinical manifestations of stage 1 hypertension often go unnoticed or are completely absent, since the body’s compensatory capabilities neutralize a slight increase in blood pressure.3 Because of this, the disease is often called the “silent killer.”
If high blood pressure levels persist for a long time, nonspecific symptoms may appear, including:
- Throbbing or pressing headache with the epicenter in the occipital region.
- Tinnitus and dizziness.
- Flashing "flies" before the eyes.
- Increased and rapid heartbeat.
- Nosebleeds.
- Poor exercise tolerance and shortness of breath.
- Swelling of the lower extremities, numbness in the legs.
When should you see a doctor?
In most cases, arterial hypertension is detected during a routine examination or seeking medical help for another disease or condition. Therefore, if there are risk factors, regular visits to your family doctor or primary care physician are recommended.
An unscheduled consultation or call to emergency medical services is required in the following situations:
- Decreased effectiveness of medications taken – situations where previously effective antihypertensive drugs no longer work.
- Increased blood pressure during treatment.
- The appearance of side effects from drug therapy.
- Deterioration of general condition while maintaining current blood pressure numbers.
- A sharp increase in blood pressure to more than 180/120 mmHg. Art., that is, the development of a hypertensive crisis.
- A sudden decrease in systolic or diastolic blood pressure of 30 mm Hg. Art. and more.
Forecast
With arterial hypertension of the 1st degree, as a rule, it is possible to avoid a further increase in blood pressure without the use of pills - by eliminating risk factors and changing a person’s lifestyle.
However, sometimes it is impossible to do without appropriate antihypertensive therapy and drug treatment. Taken together, following simple rules of behavior and regularly taking pills allows you to most effectively control the condition and prevent the development of serious complications such as myocardial infarction or stroke.
Differences between degrees and stages of hypertension
In clinical practice, several classifications of arterial hypertension are used simultaneously. Of key importance is the division of this pathology into degrees and stages of development.1
If the degree is determined depending on the pressure indicators, then the stage of the disease depends on the severity of target organ damage and the presence of clinical conditions associated with high blood pressure, diabetes mellitus and chronic kidney disease. There are 3 stages of arterial hypertension:
- Stage I: There is no end organ damage or associated clinical conditions, but there are associated risk factors. In addition to those previously mentioned, this also includes a number of laboratory indicators: lipid and blood sugar levels, uric acid and others.
- Stage II. There is asymptomatic target organ damage, determined by the results of additional examination and/or stage 3 chronic kidney disease and/or concomitant uncomplicated diabetes mellitus.
- Stage III. The presence of manifesting target organ damage and clinical conditions associated with hypertension, stage 4-5 chronic kidney disease or complicated diabetes mellitus.
What are the different degrees of hypertension?
Normal blood pressure is considered to be between 110/70 and 130/85 mm Hg. Art., which on average is the well-known 120/80 mm Hg. Art. With arterial hypertension, there is an increase in systolic blood pressure above 140 mm Hg. Art. and/or diastolic above 90 mm Hg. Art.
The degrees of hypertension are determined depending on the systolic (SBP) and/or diastolic (DBP) blood pressure (Fig. 1).
Figure 1. Degrees of hypertension in adults. Source: MedPortal, photo by cottonbro: Pexels
As a rule, at the first stage of development of hypertension, serious structural changes in the internal organs and structures of the body do not yet occur.
If hypertension continues to develop, over time, excessive blood pressure on the walls of the arteries will negatively affect both the blood vessels themselves and the target organs: the brain, retina, heart. The higher the pressure and the longer it remains uncontrolled, the greater the potential threat of decreased visual acuity, deterioration of cognitive abilities, heart pain, etc.
The most significant complications of arterial hypertension are:
- Myocardial infarction.
- Heart failure.
- Loss of visual acuity and blindness.
- Stroke.
- Dementia.
Hypertensive crisis is a complication of arterial hypertension in which blood pressure suddenly rises to 180/120 mmHg. Art. and more. In this case, direct damage to target organs occurs. This condition requires emergency medical care in a hospital setting.
Sources
- Russian Cardiological Society. Clinical guidelines “Arterial hypertension in adults”, 2021.
- High blood pressure (hypertension). Mayo clinic. 2021.
- T. V. Ashcheulova, T. N. Ambrosova, V. I. Smirnova. “The main symptoms and syndromes of hypertension and symptomatic arterial hypertension: method. decree. for students” / comp. – Kharkov: KhNMU, 2021. – 32 p.
- Tabassum N, Ahmad F. Role of natural herbs in the treatment of hypertension. Pharmacogn Rev. 2011;5(9):30-40.
- Givi M. Durability of effect of massage therapy on blood pressure. Int J Prev Med. 2013;4(5):511-516.
- Mohebbi Z, Moghadasi M, Homayouni K, Nikou MH. The effect of back massage on blood pressure in the patients with primary hypertension in 2012-2013: a randomized clinical trial. Int J Community Based Nurses Midwifery. 2014;2(4):251-258.
- Marjorie Hecht "Types and Stages of Hypertension". Healthline. 2019.