In the practice of therapeutic departments, pneumonia is considered one of the most frequently diagnosed pulmonary diseases. More than 60% of the population suffer from various diseases of the respiratory system, which, when the immune system is weakened, are often complicated by pneumonia. At the Yusupov Hospital, great attention is paid to the treatment of the inflammatory process in the respiratory organs; treatment is carried out using modern methods using innovative drugs.
Causes
Congestive pneumonia often accompanies angina pectoris, heart defects, coronary artery disease, hypertension, bronchial asthma, atrial fibrillation, diabetes mellitus, chronic pyelonephritis and many other diseases.
Predisposing factors for the development of congestive pneumonia are the age of patients over 60 years of age, prolonged forced passive position in bed due to bone injuries, cancer, spinal curvature, and chest deformities. Congestive pneumonia in bedridden patients occurs in the postoperative period after abdominal operations.
Congestive pneumonia develops against the background of congestion in the pulmonary circulation. Hemodynamic disorders are accompanied by impaired pulmonary ventilation and bronchial drainage function. Under conditions of hypoventilation and hypostasis, viscous and thick sputum accumulates in the bronchi, opportunistic and pathogenic microflora develops, which causes inflammation of the lung tissue.
Various bacteria cause congestive pneumonia: streptococci, pneumococci, Haemophilus influenzae, staphylococcus and other microorganisms. Most often, congestive pneumonia is diagnosed in the lower segments of the right lung; bilateral congestive pneumonia occurs.
Hypostatic pneumonia proceeds sluggishly, with a slight increase in low-grade fever. Little sputum is produced, breathing is weak. During blood tests, leukocytosis is rare; ESR does not increase in most cases. Congestive pneumonia can be early and late. Early hypostatic pneumonia develops in the first days of bed rest, late within several weeks.
Very often, early hypostatic pneumonia cannot be identified due to the lack of expression of symptoms and the masking of the disease as symptoms of the pathology for which the patient is being treated. With hypostatic pneumonia, symptoms similar to those of stroke or cardiovascular failure develop. Secondary congestive pneumonia very often leads to the development of pericarditis and exudative pleurisy.
Make an appointment
Aspiration pneumonia
Aspiration pneumonia was first described by Hippocrates, and until the 19th century it was called “chest disease,” which was accompanied by fever. For palliative patients, aspiration pneumonia is a terrible diagnosis. It kills up to 40% of patients. But fortunately, aspiration pneumonia is preventable.
Interestingly, aspiration of nasopharyngeal contents often occurs in healthy people, for example, at night. But this does not always cause pneumonia, including in palliative patients.
This happens because for the development of aspiration pneumonia certain conditions must exist:
- Pathological nature of the aspiration material (increased acidity, decreased acidity while taking H2 blockers and proton pump inhibitors, a large number of microorganisms and their virulence);
- Large volume and special nature of the aspirated material (more than 25 ml, large particles in the aspirate);
- Reduced factors of local respiratory tract protection.
Important
The diagnosis of “aspiration pneumonia” is made when there is an episode of massive aspiration documented by a bronchoscopy protocol, as well as in patients with risk factors for the development of aspiration.
Aspiration pneumonia does not always have a fulminant course. The rate of its development and the variability of clinical manifestations depend on the nature of the material aspirated into the respiratory tract.
The main consequences that develop in patients against the background of aspiration pneumonia:
- Mechanical obstruction of the airways;
- Chemical (aspiration) pneumonitis: non-infectious lung damage associated with the “direct” action of gastric juice;
- Bacterial pneumonia.
Complications of aspiration pneumonia:
- Necrotizing pneumonia. Formation of foci of destruction less than 1 cm in size, without fluid levels;
- Lung abscess. Single or multiple cavities larger than 2 cm;
- Empyema of the pleura.
Features of the treatment of aspiration pneumonia:
- The recommended duration of therapy without infectious complications is 14 days;
- Parenteral administration of antibacterial drugs is preferable;
- In the presence of purulent complications, fever persists for a long time (5-10 days), despite adequately selected empirical antibacterial therapy;
- Efficiency assessment should be carried out not after 72 hours, but later - on days 5-10. Therapy continues throughout this time;
- When a clinical effect is achieved, transfer to oral forms is possible (step therapy).
Methods for assessing dysphagia and preventing aspiration in palliative patients. What nuances should be taken into account when conducting the “three sips test” in palliative patients, what are the predictors of dysphagia, how to assess and prevent the risk of aspiration
Varvara Brusnitsyna
Symptomatic treatment
Prevention of aspiration pneumonia
- Minimize the “lying on your back” position;
- Change body position more often, give the patient a semi-sitting position;
- Planned rather than emergency gastrostomy (for dysphagia): the moment of gastrostomy placement is determined individually;
- Correction of sedative therapy if it leads to impaired consciousness;
- Careful oral hygiene;
- Compliance with feeding rules in patients with dysphagia:
- The head of the bed should be raised 45 degrees when feeding;
- Slow, drip administration of the mixture, rather than a bolus;
- Compliance with the rules of care when a nasogastric tube is installed.
Important What needs to be taught to relatives of patients with dysphagia:
- Follow feeding rules;
- Monitor the position of the person’s body in bed during eating and sleeping;
- Carry out oral hygiene regularly and thoroughly;
- Monitor swallowing function, pay attention to choking, difficulty swallowing, and promptly contact medical personnel.
Clinical example 1
From the anamnesis:
A 54-year-old woman has been suffering from multiple sclerosis for about 20 years with gradual progression of the disease - with limitation of motor activity, loss of self-care skills, increasing cognitive impairment, decreased self-criticism, and the appearance of dysphagia over the last year.
December 2021 - hospitalization for symptomatic therapy. The patient is fed by medical staff and relatives.
Before planned discharge, there was a progressive deterioration of the patient’s condition with an increase in respiratory symptoms, low-grade fever.
Prescription of antibacterial therapy (3rd generation cephalosporin). Increasing respiratory failure, febrile fever, pulmonary edema. Calling the resuscitation team, intubation, transfer to the intensive care unit of City Clinical Hospital No. 40.
Upon admission to the hospital of City Clinical Hospital No. 40, the condition was extremely severe, depression of consciousness to the point of coma, respiratory failure, intoxication, increasing neurological deficit.
In the hospital, the patient underwent fiberoptic bronchoscopy, purulent endotracheobronchitis of the 2nd degree was detected, the tracheobronchial tree was sanitized and food masses were aspirated. X-ray examination and CT scan of the chest revealed bilateral pneumonia: lower lobe pneumonia on the right, polysegmental pneumonia on the left, and minimal right-sided hydrothorax.
Complete blood count Leukocytes 20 x10⁹, neutrophil shift 85%
Treatment
- Sanitation bronchoscopy;
- Antibacterial therapy (meropenem, vancomycin);
- Anticoagulant therapy.
Features of the clinical case
- Rapid development of severe pneumonia with pulmonary edema;
- Clinical and radiological resolution of severe bilateral aspiration pneumonia in a short time;
- No purulent complications.
In February 2021, a planned gastrostomy was performed
. The patient continues to be monitored by the palliative care service.
Conclusions:
- The rules of feeding a patient with dysphagia were violated;
- The doctor on duty made the right decision to call the resuscitation team and urgently transfer the patient with a good life prognosis to the intensive care unit of a multidisciplinary hospital;
- The resuscitation team and the doctor on duty provided emergency medical care in a timely manner;
- Adequate initial empirical antibacterial therapy was prescribed.
It is necessary to discuss the issue of timely gastrostomy placement with the patient and his relatives as early as possible!
Clinical example 2
From the anamnesis:
Male 45 years old . He has been suffering from multiple sclerosis for about 15 years with gradual progression of the disease and disability.
From 2021 - complete loss of self-care skills , weight loss, increase in cognitive impairment.
In October 2021, difficulties appeared when swallowing solid food, frequent choking, and periodic coughing.
On November 25, 2021, he was hospitalized at the Palliative Care Center of the Moscow Health Department, and already on the third day there was an episode of aspiration while eating.
On November 29, one day after the episode of aspiration, negative dynamics with the appearance of respiratory symptoms, shortness of breath, hyperthermia, intoxication symptoms, a decrease in saturation to 88% and hypotension.
An X-ray examination of the chest organs revealed polysegmental pneumonia in the lower lobe of the right lung.
A clinical blood test revealed leukocytosis with a neutrophil shift and an increase in ESR.
A diagnosis of aspiration pneumonia was made.
Treatment
- Initial empirical antibacterial therapy (cefepime + metronidazole);
- Mucolytics;
- Oxygen therapy;
- The OVD diet is pureed with strict adherence to the rules of feeding patients with dysphagia;
Conversation with relatives about compliance with feeding rules and planned gastrostomy.
Features of this clinical case
- Rapid development of pneumonia with severe intoxication syndrome and respiratory failure;
- Persistence of fever (6 days) with positive clinical dynamics during antibacterial therapy;
- Without purulent complications;
- The duration of antibacterial therapy is 14 days.
conclusions
- The rules for feeding a patient with dysphagia were violated;
- Adequate initial empirical antibacterial therapy was prescribed;
- The duration of antibacterial therapy is 14 days;
- No infectious complications;
- It is necessary to inform and discuss with the patient and his relatives the possibility of developing dysphagia and its symptoms against the background of the underlying disease;
- It is necessary to teach relatives the rules of feeding for dysphagia;
- It is important to promptly decide on the need for elective gastrostomy.
Mechanisms of disease development
The pathophysiological mechanism of congestive pneumonia in bedridden patients is associated with passive overflow of venous vessels due to impaired blood outflow. Initially, venous hyperemia of the lung tissue develops, which is accompanied by expansion and elongation of the capillaries with subsequent compression of the alveoli. X-rays show an enhanced pulmonary pattern and reduced transparency of the lung tissue.
In the second phase of stagnation, the liquid part of the blood sweats from the vessels into the interstitial tissue and alveoli. On radiographs you can see a picture of parenchymal pneumonia or bronchopneumonia. In the third phase of congestive pneumonia, pronounced interstitial edema occurs, fibrous tissue grows, followed by the development of pneumosclerosis and hardening of the lung.
Classifications of pneumonia in palliative patients
Pneumonia can develop both at the outpatient stage (community-acquired pneumonia) and at the inpatient stage (nosocomial pneumonia). Each of these pneumonias has characteristics of pathogens.
In palliative practice, secondary pneumonias are distinguished:
- aspiration (related to aspiration),
- paracancrosis pneumonia (associated with compression of the bronchi),
- congestive (hypostatic) pneumonia (associated with circulatory disorders),
- heart attack-pneumonia.
Symptoms
The severity of clinical manifestations of congestive pneumonia depends on the severity of the underlying pathology, the degree of ventilation and hemodynamic disturbances, and the addition of the inflammatory process. But in general, the symptoms of congestive pneumonia do not differ from the symptoms of ordinary pneumonia. Hypostatic pneumonia manifests itself with the following symptoms:
- wheezing in the lungs;
- cough;
- low-grade fever;
- weakness and excessive sweating;
- chills;
- shortness of breath, which worsens with physical exertion;
- a small amount of sputum, there may be purulent discharge, blood in the sputum.
The severity of symptoms depends on the duration and severity of the disease. The danger of congestive pneumonia is the cessation of participation of the affected alveoli and lung tissue in the respiratory process. In a bedridden patient, the cough reflex does not work, sputum does not come out - the patient’s condition worsens, and larger and larger areas of the organ cease to participate in breathing. The active activity of microorganisms leads to intoxication, the patient loses appetite, experiences headaches, pain in muscles and joints.
Congestive pneumonia can be early (in the first 2-3 days of bed rest) and late (from the second to the sixth week). Early congestive pneumonia often occurs under the guise of the underlying pathology. Thus, during a stroke, patients have severe breathing disorders (noisy, bubbling, arrhythmic) and impaired consciousness. In patients suffering from cardiovascular diseases, a manifestation of congestive pneumonia may be an increase in signs of heart failure.
Make an appointment
Antibacterial therapy for pneumonia
Antibacterial therapy can be empirical and targeted etiotropic. In palliative practice, empirical is used in most cases.
Features of antibacterial therapy in palliative practice
If nosocomial pneumonia is suspected in a palliative patient, initial empirical antibacterial therapy is prescribed. This can be monotherapy or combination therapy if there is a high probability of multidrug-resistant pathogens. Intravenous administration of antibacterial drugs is preferable. If the patient's condition improves and he has normal gastrointestinal function, he can be switched to oral medications. Routinely prescribing combination regimens of antibacterial drugs in palliative practice is considered inappropriate.
Solving complex issues of prescribing antibacterial therapy
Diagnostics
Due to the low specificity of clinical symptoms and the predominance of the severity of symptoms of the underlying disease, the diagnosis of congestive pneumonia in most cases presents a certain difficulty. The Yusupov Hospital employs pulmonologists, cardiologists, neurologists, and traumatologists who are wary of bronchopulmonary complications in bedridden patients.
During auscultation of the lungs with congestive pneumonia, hard breathing and moist fine bubbling rales are heard in the posterior lower parts of the lungs. In this case, doctors at the Yusupov Hospital prescribe an X-ray of the lungs. It allows you to detect a unilateral or bilateral decrease in the transparency of the lung fields, increased pulmonary pattern, focal and focal shadows, linear shadows in the basal sections, expansion of the shadow of the roots of the lung, hemosiderin nodules.
Using ultrasound examination of the pleural cavity and pericardium, the presence of effusion in the pleural cavity and cardiac sac is determined. Patients with congestive pneumonia must have an electrocardiogram recorded and echocardiography performed. In the blood test for congestive pneumonia, the changes are minimal: there is a slight leukocytosis with a neutrophilic shift to the left, an increase in the erythrocyte sedimentation rate. During a microscopic examination of sputum in patients with congestive pneumonia against the background of heart defects, laboratory assistants detect groups of cells containing hemosiderin.
Study design
A prospective cohort study included 4988 adult patients with pneumonia without HF seen at 6 Canadian medical centers from 2000 to 2002.
Patients were matched by gender, age and place of treatment (outpatient treatment or hospitalization) in a ratio of 1 to 5 with individuals without pneumonia (n=23,060).
The primary endpoint of the study was the risk of hospitalization due to HF and a composite endpoint of HF and death.
The Cox model was used as a statistical analysis method.
Treatment
Congestive pneumonia is a dangerous disease that can lead to various complications and death of the patient. Therefore, if symptoms appear, it is important to seek medical help promptly. The treatment algorithm for congestive pneumonia, which is used by doctors at the Yusupov Hospital, includes fighting bacterial infections, reducing swelling, regulating ventilation and oxygen supply to the lungs. Pulmonologists provide complex therapy, which includes:
- antibiotics;
- diuretics;
- expectorants, immunomodulatory and antioxidant drugs;
- agents that improve the metabolism of the heart muscle;
- cardiac glycosides.
Patients are prescribed oxygen therapy, inhalation therapy, back and chest massage, and therapeutic exercises. To remove sputum from the tracheobronchial tree, bronchoalveolar lavage and sanitation bronchoscopy are performed. In the presence of pericardial pleural effusion, thoracentesis and pericardial puncture are performed. In parallel with the treatment of congestive pneumonia, the background conditions that contributed to the development of secondary inflammation in the lungs are corrected.
To treat congestive pneumonia, physiotherapeutic methods of treatment are used: UHF electric field, inductothermy, decimeter wave therapy, magnetic therapy, ultraviolet irradiation, electrophoresis. Patients are given inhalations of bronchodilators, drugs that dilute sputum.
Heart attack-pneumonia
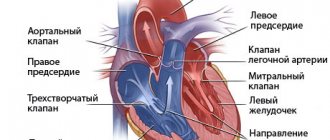
Infarction-pneumonia is secondary pneumonia against the background of a local persistent circulatory disorder in the pulmonary tissue due to thromboembolism of the branches of the pulmonary artery.
Pulmonary embolism can be massive and lead to severe hemodynamic compromise, which can result in the death of the patient.
Thromboembolism can be submassive when lobar and segmental branches are involved. It may also involve damage to small branches of the pulmonary artery. This leads to local infarctions of the pulmonary parenchyma and the development of pulmonary infarction and infarction-pneumonia.
It is important to remember: when hospitalized in older patients, thromboembolism is the cause of death in 10% of patients.
Features of the clinical course of infarction-pneumonia are an acute onset, often with pain and inspiratory shortness of breath, a feeling of tightness in the chest, and frequent hemoptysis. Infarction-pneumonia has a tendency to abscess formation, pleurisy and may be accompanied by hyperbilirubinemia.
Important In half of elderly patients, infarction-pneumonia may be asymptomatic. Classically it occurs only in 10% of patients. Therefore, doctors need to pay attention to patient complaints of discomfort and pain in the chest, tachypnea and dyspnea, tachycardia and pleural effusion. Pleural effusion in patients is often hemorrhagic in nature.
In a palliative care hospital setting, it is quite difficult to diagnose pulmonary embolism with infarction-pneumonia. Indeed, according to clinical data, it is impossible to either confirm or refute pulmonary embolism with sufficient confidence.
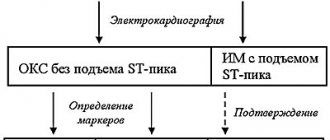
Diagnosis of infarction-pneumonia:
- X-ray of the chest organs;
- ECG, ECHO-CG;
- General blood analysis;
- D-dimer;
- Doppler ultrasound of the veins of the lower extremities;
- Computed tomography with angiopulmonography.
Important Features of infarction pneumonia are darkening of the lung tissue of a triangular shape, the base of which is directed towards the periphery.
Treatment tactics for infarction-pneumonia:
- Etiotropic therapy (antibacterial);
- Anticoagulant therapy;
- Symptomatic therapy (relief of pain, shortness of breath with the prescription of non-narcotic and narcotic analgesics);
- In case of respiratory failure - respiratory support (oxygen concentrator);
- Correction of therapy for the underlying disease.
Prevention of heart attack-pneumonia:
- Monitoring the condition of peripheral veins - ultrasound examination of the veins of the lower extremities;
- Timely administration of anticoagulant therapy according to indications;
- If possible, activate bedridden patients;
- Combating venous stagnation in the lower extremities - eliminating drugs that cause hypercoagulation;
- Timely correction of therapy for diseases with a high risk of developing pulmonary embolism;
- Individual prevention of venous stagnation in the lower extremities using compression stockings and elastic bandaging.
Prevention
The Yusupov Hospital uses a set of measures aimed at preventing congestive inflammation in bedridden patients. For this purpose, the patient’s position is often changed and he is asked to perform active movements in bed and breathing exercises. Percussion chest massage and cupping massage are performed. Patients are provided with a balanced, varied and vitamin-enriched diet. If you have signs of congestive pneumonia, call. The contact center of the Yusupov Hospital is open 24 hours a day, seven days a week.
Make an appointment