Thrombophilia is a congenital or acquired pathological condition that is characterized by impaired blood clotting and an increased risk of blood clots. It is distinguished by its duration and sudden complications such as the formation of a blood clot in a vein, its fixation to the wall with the development of inflammatory processes (phlebothrombosis) or blockage of blood vessels by a blood clot (thromboembolism). Such conditions pose a danger to the health and life of the patient and require professional medical care.
At the same time, it is worth noting that thrombophilia cannot always lead to complications in the form of thrombosis or thromboembolism - however, the risk of their occurrence with this pathology increases significantly.
Thrombophilia - what kind of disease is it?
Thrombosis is the process of forming blood clots where the vascular wall is damaged; its purpose is to ensure the safety of the vascular system.
This process itself is physiologically normal; it prevents excessive blood loss at the sites of injury. But if the thrombotic process is excessive, then pathological thrombosis occurs. When answering the question of what thrombophilia is, we can give a clear example in the form of a photo that shows increased activity of blood cells and the formation of a blood clot. The disease is not always accompanied by thromboembolism or thrombosis, but the risk of blood clots in various places of the circulatory system greatly increases. Now modern medicine is concerned about the problem of this disease, since deaths quite often occur due to blockage of a blood vessel. The most commonly diagnosed hereditary thrombophilia is hereditary thrombophilia. According to statistics, in Europe about 15% of people suffer from this disease.
Do not confuse concepts such as thrombophilia and trypophilia. These are completely unrelated terms. But sometimes you can hear the question: trypophilia, what is it? The concept means phobia, fear of accumulation of objects with a rounded shape, cluster holes. So tripophilia is fear and discomfort associated, for example, with lotus seeds, honeycombs, and not a disease that manifests itself as pathologies in the body.
Symptoms and clinical picture
Symptomatically, thrombophilia is expressed in the following manifestations:
- Infarction of internal organs at a young or relatively young age;
- Multiple (recurrent) thrombosis;
- Tendency to pulmonary embolism (PE).
Vascular thrombosis does not always appear immediately. The patient may not suspect that he has a blood clot for a long time until a serious complication occurs.
Complications of thrombosis:
- Ischemic stroke;
- Myocardial infarction;
- Chronic venous insufficiency;
- Pulmonary embolism;
- Necrosis of intestinal tissue and the development of acute peritonitis against its background;
- Gangrene of the lower extremities (subject to appropriate localization of the blood clot);
- Spontaneous abortion (in pregnant women suffering from thrombophilia).
In almost all cases, thrombophilia is discovered accidentally, due to patient complaints of one or more of the listed complications.
Signs of thrombophilia
The disease often has no symptoms. Sometimes thrombosis occurs in the veins of the leg. This causes redness, swelling and discomfort. Such signs of thrombophilia are called deep vein thrombosis. Blood clots or blood clots must be treated with special blood thinners. This disease can be diagnosed in thrombophilia using devices that allow you to take photos, for example, to conduct an ultrasound examination.
Blood clots are not only dangerous to health, they can be fatal if they break off and enter the bloodstream to vital organs.
When a blood clot appears, the following symptoms appear:
- difficulty breathing;
- numbness of the feet and legs;
- chest pain when inhaling;
- heart attacks at a young age;
- swelling, pain at the site of thrombus formation - these are the most obvious symptoms of thrombophilia;
- cardiopalmus;
- coughing up blood;
- pregnancy disorders, constant miscarriages.
Types of disease
When answering the question of what thrombophilia is, it is necessary to understand that the development of the disease can depend on many factors. Its carriers, according to statistics, are almost two-fifths of the Earth's population. The disease is growing every year. There are two main types of pathology - congenital and acquired thrombophilia. With a hereditary disease, various abnormalities are found in genes. The most common factors are:
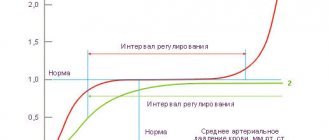
- deficiency of protein S and C, as well as antithrombin III. Proteins regulate the intensity of clotting, so if they are insufficient, excessive thrombus formation occurs. Antithrombin III creates compounds with thrombin, this leads to mutual inactivation. The component is one of the most important in the anticoagulant system;
- molecular abnormalities of fibrinogen;
- polymorphism of the V factor gene. A defect appears in the gene that carries information about the fifth blood clotting factor. This factor is also called the Leiden mutation;
- single nucleotide substitution G20210A;
- increased lipoprotein levels.
Thrombophilias that occur as a result of taking medications, injuries, or concomitant diseases are acquired. They do not arise unexpectedly and spontaneously; there is always a reason for the appearance of pathology.
- There are some other types of disease:
- hematogenous thrombophilia. Due to disturbances in blood composition, abnormalities in the coagulation system or platelet hemostasis, there is a tendency to repeated thrombosis of blood vessels of various locations. This is one of the most dangerous types of disease. The photo shows how a blood clot forms due to disorders caused by thrombophilia. It can cause thromboembolism, i.e. acute blockage of the vessel will occur. There are two types of hematogenous thrombophilias. The first group is associated with changes in the cellular composition of the blood and its rheological properties. The second group is associated with primary disorders in the hemostatic system;
- hemodynamic thrombophilia is associated with disorders of the circulatory system;
- Vascular thrombophilia includes diseases such as vasculitis and atherosclerosis.
Thrombophilia during pregnancy
It often coincides that hereditary thrombophilia and pregnancy manifest themselves simultaneously. This is due to the fact that a woman who is expecting a child develops an additional circle of blood circulation - the placental one, which has its own specific characteristics and puts an additional burden on the body. Thrombophilia is a disease in which the blood coagulation system is disrupted, leading to the possibility of serious complications, so pregnancy and thrombophilia are a dangerous combination that requires increased attention from women and doctors.
During pregnancy, a woman's body undergoes major changes, in particular, blood clotting increases. This is due to a decrease in blood loss during childbirth or such pathological conditions as placental abruption and miscarriage. With thrombophilia, the risk of blood clots is high, therefore, when it is also accompanied by physiological features of pregnancy in the form of increased coagulability, an even greater danger arises.
Often pregnant women experience a hematogenous type of disease associated with antiphospholipid syndrome. However, the course of the disease is usually unpredictable and there is no universal treatment regimen. Typically, thrombophilia may not manifest itself in any way, but during pregnancy the risk of thrombosis increases sixfold. The main danger can be a miscarriage at a short stage of pregnancy. This condition is fraught with the fact that blood clots can form in the vessels that lead to the placenta, which causes hypoxia and developmental delay in the fetus. The child’s body stops receiving nutrients, which leads to placental insufficiency, placental abruption, malformations, miscarriages and premature birth.
It is believed that the disease does not manifest itself in any way until ten weeks. There is no data on the effect of pathology on the development of pregnancy in the early stages. In the second trimester, thrombophilia usually also behaves calmly, and unpleasant consequences rarely occur. The risk of complications increases after 30 weeks, when placental abruption may occur.
If you are able to carry a child to term due to the disease, the birth usually occurs ahead of schedule, at 35-37 weeks. This scenario is considered favorable.
When making a diagnosis during pregnancy, the doctor should tell the woman what thrombophilia is and immediately prescribe treatment. The course of therapy consists of medications, a special diet and exercise. If you strictly follow all medical recommendations, the chances of carrying and giving birth to a healthy child are great. It is important to remember that preterm labor is likely to occur before 40 weeks. But with the modern level of medicine, babies born at earlier stages are cared for, so thrombophilia is not a death sentence for a woman who wants to have children. If you have a diagnosis of genetic thrombophilia, it is important to plan your pregnancy in advance, and then the risks of possible complications will be reduced.
If you notice similar symptoms, consult a doctor immediately. It is easier to prevent a disease than to deal with the consequences.
Causes
In recent decades, there has been an increase in the number of patients who suffer from congenital and acquired forms of thrombophilia. Scientists explain this by the following factors:
- deterioration of the environmental situation in the world;
- "population aging;
- failure to seek professional medical help in a timely manner.
At CELT you can get advice from a phlebologist.
- Initial consultation – 3,000
- Repeated consultation – 2,000
Make an appointment
The division into genetic and acquired thrombophilia is carried out based on the cause of the disease. Thus, genetic thrombophilia is the result of structural features of certain genes that lead to disturbances in the functioning of the blood clotting system. The most common hereditary thrombophilias are:
- polymorphism (Leiden mutation) of blood clotting factor V;
- polymorphism in the prothrombin II blood clotting factor gene;
- protein S deficiency;
- protein C deficiency;
- antithrombin deficiency.
They arise due to:
- increased levels of lipoproteins in the blood;
- lack of antithrombin III;
- lack of prothrombins S and C;
- thalassemia;
- factor V gene mutations;
- prothrombin mutations.
Unlike congenital thrombophilia, acquired forms develop against the background of other diseases, including cancer, as well as when taking certain medications. It is customary to highlight the following reasons:
- long-term venous catheterization;
- heart defects;
- cancerous tumors, the treatment of which involves massive chemotherapy;
- autoimmune diseases;
- dehydration of the body, accompanied by an increase in the number of red blood cells.
Diagnosis of the disease
Typically, diagnosing thrombophilia has a number of difficulties. This mainly happens because the disease may not manifest itself in any way and not give any symptoms. To clarify the disease, you need to contact a phlebologist; he uses a visual examination of the patient, hardware and laboratory diagnostics.
During the initial examination, the doctor determines the location of the damaged area and the degree of its changes. Typically, patients complain of swelling, hyperthermia in the area where varicose veins are located, and nagging pain after sitting or walking. On palpation, severe pain is determined. Based on these signs, the doctor prescribes a general blood test, tests for D-dimer content, and a coagulogram.
Laboratory analysis for thrombophilia includes the study of genes for platelet receptors, blood clotting factors, fibrinolysis, etc. In essence, genetic markers of thrombophilia are determined, which play an important role in the appearance of a congenital type of disease. There are two types of polymorphism - heterozygous and homozygous. The latter of these is considered more serious in terms of complications and treatment.
The need for testing for genetic markers is determined by a phlebologist individually and depends on the clinical picture. Indications for this laboratory diagnosis are:
- the presence of thromboembolic diseases at a young age;
- phlebeurysm;
- stroke and heart attack;
- cardiovascular diseases in close relatives;
- disorders associated with pregnancy: placental insufficiency, intrauterine growth retardation, fetal death, placental abruption, miscarriage, early miscarriages, toxicosis, severe forms of gestosis;
- use of oral contraceptives;
- recurrent thromboembolism;
- obesity.
Instrumental diagnosis of the disease is very informative. Computer programs provide detailed results on the condition of veins, valves, lumens, and thrombotic masses.
- Doppler ultrasound allows you to determine the speed and direction of blood flow in different parts of the vessel. This method does not provide the opportunity to study data on the structure and anatomy of veins.
- Ultrasound angiography of the lower extremities. The study is based on the ability of tissues to reflect and absorb ultrasound waves differently. The study is carried out only for serious indications, as it is an invasive diagnostic method. During the procedure, a contrast agent is injected into the vessel, the device tracks its movement, thereby creating a three-dimensional picture of all veins and arteries. It is recommended to perform angiography after Doppler sonography.
- Phlebography is an x-ray examination using an iodine-containing contrast agent.
- Phleboscintigraphy - the procedure is also based on the method of introducing a contrast agent, here it is a radioactive isotope with a short half-life.
- Spiral computed tomography is a new accurate diagnostic method. Allows you to create a volumetric 3D reconstruction and determine the condition and location of the veins. This procedure is indispensable for emergency diagnosis of thromboembolism.
- Magnetic resonance imaging.
After making a diagnosis, the doctor will tell you what kind of disease it is, thrombophilia, and prescribe the necessary treatment. Additionally, patients are prescribed a chest x-ray to prevent pulmonary embolism. Full diagnostics can be performed in any modern phlebological center
.
References
- Academician RAMS, prof. IN AND. Krasnopolsky, Doctor of Medical Sciences, Prof. V.A. Petrukhin, Ph.D. A.P. Melnikov: Management of pregnant women with thrombophilia. — Russian Bulletin of Obstetrician-Gynecologist 4, 2013
- R.G. Shmakov, P.A. Kiryushchenkov, A.V. Pyregov, M.A. Vinogradova, O.R. Baev, N.E. Kahn, O.G. Pekarev, N.I. Klimenchenko, N.K. Tetruashvili, V.L. Tyutyunnik, Z.S. Khodzhaeva, N.V. Dolgushina, Brief protocol: Study of the hemostatic system during pregnancy and after childbirth, 2015.
- Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy. American College of Chest Physicians evidence-based clinical practice guidelines 8th edition. American College of Chest Physicians – Medical Specialty Society. 2001 January.
- Tsantes AE, et al. Association between the plasminogen activator inhibitor-1 4G/5G polymorphism and venous thrombosis. A meta-analysis. Thromb Haemost 2007 Jun;97(6):907-13.
Thrombophilia - treatment
Treatment of thrombophilia begins with the choice of a qualified doctor, his goal is to eliminate thrombotic complications.
Medications prescribed:
- anticoagulants (low molecular weight heparins), which reduce blood clotting;
- antiplatelet agents for the prevention of thromboembolism;
- drugs that improve liver function;
- fibrinolytic agents;
- folic acid has indications for certain types of disease;
- If there is a risk of cerebral edema, glucocorticoid drugs (dexamethasone) are recommended.
To prevent complications, it is recommended to use preventive measures. This is especially true during pregnancy:
- physical therapy classes;
- no heavy lifting or prolonged standing;
- wearing medical compression stockings or elastic bandages;
- swimming;
- electromagnetic therapy;
- self-massage;
- proper nutrition;
- phytotherapy.
For thrombophilia, it is recommended to do the following exercise: lying on your back, raise and lower your legs without sudden movements. It is possible to use hirudotherapy, where special medicinal leeches are used.
Treatment of thrombophilia during pregnancy
Often, it is during the period of waiting for a child that genetic thrombophilia manifests itself, so treatment of pregnant women with this diagnosis should be started as early as possible. In this case, approximately the same drugs are used as for other categories. The following primary and auxiliary medications are used in practice:
- Aescin;
- Nadroparin calcium;
- Troxerutin;
- Mannol;
- Dexamethasone;
- Fraxiparine;
- Femibion-2;
- Wessel Due F;
- Sometimes with APS, aspirin is prescribed to prevent thrombosis, as well as to prevent gestosis.
During pregnancy, there are certain indications for hospitalization of patients:
- antenatal hospitalization in an obstetrics and gynecology hospital for cerebral vein thrombosis;
- varicose veins are observed, in this case the patient is sent to a surgical hospital, the issue of maintaining or terminating the pregnancy is decided;
- patients are hospitalized in a neurosurgical hospital if an unspecified venous complication occurs.
Thrombophilia - treatment with folk remedies
Folk experience has collected many recipes, some of which will be useful for reducing blood clotting.
- Tincture of Sophora japonica. You need to take 100 grams of seeds and pour half a liter of good vodka over them. Leave for two weeks in a dark place. The product is taken 3 times a day before meals, 10 drops of tincture are diluted in a quarter glass of water.
- Grape juice has proven itself well; its daily consumption reduces platelet activity.
- Infusion of meadowsweet. Pour 2 teaspoons into a glass of boiling water, strain and drink one third of a glass before meals.
- It is useful to use infusions, jams, compotes from berries and raspberry leaves.
- Garlic is one of the unique natural remedies that can thin the blood, so you can include 2-3 cloves in your diet.
- Ginkgo biloba leaf extract is used.
- Multicomponent infusion. Chereda, St. John's wort 20 grams; coriander fruits, licorice root, marsh grass, chamomile, flaxseed, sweet clover 10 grams each. The mixture of herbs is poured into 500 ml of boiling water and left for 2 hours. Then the infusion is filtered and drunk, you can add honey. The dosage is 200 ml twice a day an hour after meals.
Herbs that have a blood-clotting effect, such as water pepper and nettle, should not be used in case of illness. Before using folk remedies, you should definitely consult a doctor; many of them have contraindications.
Treatment
Treatment of thrombophilia is prescribed individually with the obligatory participation of a hematologist and directly depends on the factors that led to the onset of this disease. It is aimed at combating thrombosis and treating the underlying disease.
Conservative treatment methods provide an integrated approach, in which special attention is paid to eliminating the cause of the pathology. In addition, a general regimen for the treatment and prevention of thrombosis is used.
This is due to the fact that there is no specific therapy for the treatment of thrombophilia. Treatment is as follows:
- Prescribing a diet that limits the consumption of fatty and fried foods and completely eliminates foods high in cholesterol;
- Taking medications that inhibit platelet aggregation (Aspirin, Curantil), anticoagulants (Warfarin), drugs that have a strengthening effect on vascular walls (Papaverine, Trental);
- The use of traditional medicine: freshly squeezed grape juice, cranberry tea, tincture of Japanese sophora seeds.
Treatment of thrombophilia resulting from a deficiency of coagulation factors and antithrombin III involves the transfusion of large volumes of plasma, which are combined with the introduction of Heparin into the blood. Congenital thrombophilia, which occurs due to a lack of antithrombin III, requires the use of replacement therapy: the introduction of drugs with antithrombin III into the blood three hours after the administration of Heparin. Treatment of mild forms of thrombophilia is carried out by subcutaneous administration of lyophilized plasma and Heparin 4 times a day. Intravenous administration of antithrombin III can achieve good results.
In severe forms of the disease, direct-acting anticoagulants are used, which are combined with fibrinolytic agents. This treatment gives especially good results when the drug is administered at the level of the affected vessel.
Diet for thrombophilia
In case of illness, a special antithrombotic diet is prescribed. It is necessary to limit foods that can increase blood viscosity. The diet should exclude the following foods:
- lard, fatty meat, rich broth;
- chocolate;
- whole milk;
- legumes;
- beef liver;
- hard cheeses;
- coffee, large amounts of green tea;
- celery, parsley, spinach;
- Do not eat spicy or fatty foods.
It is advisable to consume foods that reduce blood clotting:
- cranberries, viburnum, lingonberries, chokeberries;
- seafood;
- ginger;
- seaweed;
- red fruit drinks and juices;
- cereal porridges - pearl barley, oatmeal, barley, buckwheat,
- dried fruits - dates, dried apricots, figs, raisins, prunes.
Danger and risk factors
The development of the disease is influenced by a hereditary factor (genetic thrombophilia). But there are also some acquired risks:
- blood diseases. Erythremia, atherosclerosis, varicose veins of the lower extremities, arterial hypertension;
- diseases that affect motor activity (Schlatter's disease), malignant tumors, autoimmune diseases (antiphospholipid syndrome, systemic lupus erythematosus), polycystic kidney disease can indirectly affect the development of pathology;
- infectious processes;
- suffered a heart attack or stroke;
- surgical interventions;
- venous catheterization;
- liver diseases;
- obesity;
- pregnancy period;
- nephrotic syndrome;
- some medications (oral contraceptives, prednisolone).
Forms and stages of the disease
Experts in the field of phlebology classify the disease into two main categories.
The first category includes thrombophilias provoked by pathological changes in the cellular composition of the blood and its normal rheology. Such violations result from the following processes:
- Blood thickening;
- Change in plasma viscosity;
- Defects in the natural shape of red blood cells.
The listed processes are often caused by exogenous triggers.
The second category is caused by primary disorders of coagulation and hemostasis. It includes congenital pathological conditions caused by a deficiency or excess of coagulation factors.
Thrombophilia can be vascular, hemodynamic and hematogenous.
Prevention of complications of thrombophilia
No matter how professional a doctor is, you cannot shift responsibility for your health only to the achievements of modern medicine; it is important to remember that each person himself must also take care of it. In order to prevent complications from thrombophilia, you need to follow a number of simple rules:
- reconsider your lifestyle. Today, everyone who sits a lot and moves little is at risk of illness. Moderate physical activity, exercise, physical therapy will only improve your health;
- proper diet, avoidance of excessive consumption of fatty and smoked foods, as well as industrial semi-finished products;
- reduce the amount of meat consumed;
- special drinking regime - you need to drink at least one and a half liters of clean water per day;
- preventive medical examinations.
This article is posted for educational purposes only and does not constitute scientific material or professional medical advice.
Diagnostics
Diagnosis of thrombophilia is not difficult for a qualified phlebologist.
It includes the following steps:
- Questioning the patient about current complaints;
- Study of anamnesis (patient medical history);
- Assessment of family history (questioning the patient regarding the tendency to thrombosis in close relatives - mother, father, brothers, sisters);
- Laboratory tests (blood tests for prothrombin time, APTT, coagulation factors, fibrinogen, plasminogen, VWF, D-dimers and other studies at the discretion of the doctor).
The results of the listed examinations are sufficient to make a correct and accurate diagnosis.
Once the diagnosis is established, some hardware manipulation may be required to detect the thrombus. Next, specialists decide on therapeutic tactics. It can be conservative and selected by a phlebologist, or operative (surgical removal of a blood clot) and performed by a vascular surgeon.