Arterial disease, known as atherosclerosis obliterans, is the irreversible growth of low-density lipoprotein plaques under the inner lining of the arteries.
The term “obliteration” means the gradual complete closure of the lumen of a vessel with the development of ischemia of organs and tissues where blood stops flowing. It reflects the most severe variant of the course of the atherosclerotic process with damage to large and medium-sized arteries. Such vessels include: the aorta, arteries of the kidneys, abdominal cavity, upper and lower extremities.
In medical practice, the diagnosis is more common when describing circulatory disorders in the legs, although it is possible to develop atherosclerosis in an obliterating form in the arms, in the renal and mesenteric arteries.
What does the ICD say?
The International Classification of Diseases (ICD-10) does not have a characteristic name for the disease. It is taken into account in the class “Diseases of the heart and blood vessels”, in the subclass “Diseases of the arteries”, in the group “Atherosclerosis” with code I70.
For atherosclerosis of the vessels of the extremities, the general code I70.2 is established. Separate codes take into account lesions of the renal, mesenteric and other peripheral arteries.
Obliterating atherosclerosis of the arteries of the legs is most clearly and often manifested. Let's consider the reasons for its development, possible approaches to diagnosis and treatment.
Atherosclerosis of the renal arteries
The formation of an atherosclerotic plaque at the mouth of the renal artery is a common cause of the development of renovascular hypertension. The pathology has characteristic symptoms that can help identify the disorder at an early stage:
- high blood pressure;
- headaches and dizziness;
- shortness of breath due to strain on the heart;
- kidney dysfunction;
- Laboratory tests reveal protein in the urine.
The danger of the disease is that vascular thrombosis can develop, and if both kidneys are affected, a malignant tumor can develop. Only timely diagnosis using modern methods will protect you from dangers.
Why does this form of atherosclerosis develop?
The reasons for the development of obliterating atherosclerosis of the legs include general factors that accelerate the atherosclerotic process, negatively affect the level of cholesterol in the blood, and typical conditions for damage specifically to the vessels of the lower extremities.
General factors:
- age-related characteristics - it has been established that in people over 40 years of age, immunity is significantly reduced due to the cessation of the activity of the thymus gland, this allows infectious agents to easily destroy the arterial wall, the help of cholesterol in “patching holes” becomes excessive and causes deposits in the form of plaques;
- the greatest changes in men are associated with the protection of the female body by sex hormones and changes during pregnancy;
- nicotine intoxication in smokers promotes spastic contractions of the vascular bed and disrupts the regulation of tone by the nervous system;
- stress, uncontrollable situations, stressful working conditions, nervous breakdowns lead to an increased role of arterial spasm;
- poor nutrition causes an excess intake of fats and light carbohydrates, which are not processed into energy, but are stored as excess weight or increase the level of cholesterol derivatives in the blood, from which plaques are built;
- passive sedentary lifestyle;
- presence of concomitant diseases (hypertension, diabetes mellitus);
- hereditary predisposition.
Local factors contributing to damage to the blood vessels of the legs include:
- frequent hypothermia, frostbite of the legs;
- wearing tight shoes that impede blood supply;
- previous injuries (bruises, fractures).
Conclusion
Atherosclerosis of the coronary vessels is a disease that results from an unhealthy lifestyle, so it is necessary to adjust your diet, establish a daily routine, and also introduce daily physical activity.
As noted earlier, it is extremely difficult to completely avoid this disease and standard treatment with statins inhibits the performance of the most important vitamins D and K2 for humans, which leads to a complete loss of vascular elasticity, so it is important to receive additional doses of these substances from the outside. For example, Osteo K2 completely covers the amount of vitamin D and K2 necessary for the elasticity of the vascular wall, even when taking statins.
Mechanism of arterial damage
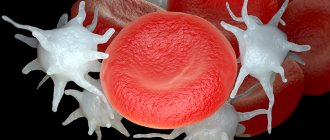
All of these reasons disrupt fat metabolism, namely the accumulation of low-density lipoproteins and triglycerides. These substances are normally carriers of molecules, but during illness they change, binding to antibodies, becoming accumulations of unnecessary reserves in cells.
The process intensifies with diabetes, hypertension, decreased thyroid function, gout, during menopause, and under the influence of stressful situations.
The other side is impaired utilization of lipoproteins by the liver. This depends on the loss of sensitivity of hepatocyte cells to the changed complexes. Nerve endings (receptors) do not recognize them, so they are not accepted for processing.
Heredity is explained by mutation of genes that control the fat metabolism of cholesterol compounds.
What are the reasons for the development?
The brachiocephalic vessels are a network of main arteries that arise directly from the aorta. The vascular branches are responsible for blood circulation in the right side of the shoulder girdle, as well as in brain cells.
Therefore, when atherosclerosis of the brachiocephalic vessels develops and atherosclerotic plaques gradually fill the lumen of the arteries, the brain, which experiences oxygen starvation and lacks the necessary substances, is the first to suffer. Damage to the extracranial parts of the BCA occurs due to the negative influence of many pathological factors, among which the most common are:
- genetic predisposition;
- violation of metabolic processes;
- hormonal and endocrine disorders;
- systemic diseases;
- liver dysfunction;
- arterial hypertension;
- poor diet, consumption of excessive amounts of animal fats;
- inactive lifestyle;
- constant stress;
- obesity;
- abuse of alcoholic beverages and cigarettes.
Return to contents
What do diseased leg arteries “look like” from the inside?
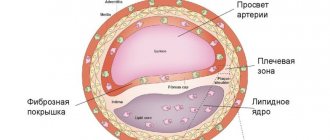
Plaques form more often in places of greatest blood flow pressure, in the area of vascular branches. From the inside, the artery wall is yellowish in color, dense, elasticity is lost, deformation and deposition of calcium salts are possible.
The femoral and popliteal arteries have five types of lesions according to location and extent:
- type 1 - limited areas of narrowing (occlusion) in individual segments;
- type 2 - widespread changes in the entire surface of only the external femoral vessel;
- type 3 - widespread occlusion of the external femoral and popliteal arteries, but preservation of patency at the site of the fork of the popliteal branch;
- type 4 - obliteration of the superficial femoral and popliteal arteries in combination with the level of the fork of the popliteal branch, but with preserved patency of the deep femoral artery;
- type 5 is the most severe lesion, since there is narrowing at the level of the superficial, deep femoral and popliteal arteries.
In combined lesions of the arterial vessels of the leg with the popliteal, 3 types are distinguished:
- type 1 - with complete obliteration of the popliteal segment and the initial parts of the tibial arteries, patency in the middle and lower part of the leg is preserved;
- type 2 - narrowing at the level of one or two arteries of the leg, but there is blood flow in the lower part of the popliteal and tibial arteries;
- type 3 - patency is preserved only at the level of small branches on the legs and feet.
Progressive atherosclerosis causes ulceration of the plaque with tissue breakdown. The detached masses migrate to more distant areas of the legs, cause thrombosis, and impair blood circulation.
Another outcome is the formation of an aneurysmal sac, thinning of the wall and internal bleeding from the damaged vessel.
Publications in the media
Atherosclerosis is a systemic disease that affects arteries of elastic (aorta and its branches) and muscular-elastic (arteries of the heart, brain, etc.) types. At the same time, pockets of lipid, mainly cholesterol, deposits (atheromatous plaques) are formed in the inner lining of arterial vessels, which causes a progressive narrowing of the lumen of the vessels until their complete obliteration. Atherosclerosis is a leading cause of morbidity and mortality in Russia, the USA and most Western countries.
• In chronic, slowly increasing obliteration, the clinical picture of atherosclerosis is determined by the degree of insufficiency of blood supply to the organ supplied by the affected artery.
• Acute occlusion of the arterial lumen by a thrombus and/or the contents of a disintegrated atheromatous plaque is possible, which leads to the formation of foci of necrosis (infarction) or gangrene of an organ or body part located in the basin of the affected artery.
• The area of carotid artery bifurcation, coronary arteries and abdominal aorta are most susceptible to atherosclerotic damage.
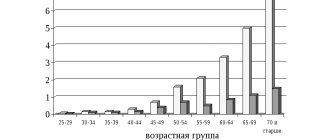
Frequency. 150:100,000 at age 50. The consequences of atherosclerosis are the main cause of mortality. The predominant age is elderly. The predominant gender is male (5:1).
Etiopathogenesis. The theory of damage and accumulation is based on the recognition of the damaging effect of various risk factors (see Risk Factors) on the vascular endothelium. SMC proliferation and macrophage migration into the vascular wall begin. Through the damaged endothelium, lipids and cholesterol penetrate into the inner lining of the vessel, forming an atheromatous plaque. Atheromatous plaque leads to vascular stenosis, induces platelet activation and thrombus formation, which leads to ischemia and/or necrosis of the affected organ.
Genetic aspects. Family predisposition to atherosclerosis is associated with inheritance of risk factors (excluding smoking and taking oral contraceptives, see also Apolipoprotein defects).
Risk factors • Smoking • Diabetes • Arterial hypertension • Obesity • Hypercholesterolemia (ratio of low-density lipoprotein [LDL] to high-density lipoprotein [HDL] more than 5:1) • Hypertriglyceridemia • Physical inactivity • Family history of strokes and cardiovascular diseases • Taking oral contraceptives .
Pathomorphology • I degree - preclinical period of the disease. On the unchanged inner lining of the arteries, single lipid spots and stripes are found (lipoidosis) • Degree II - mild atherosclerosis. On the unchanged inner lining of the arteries there is lipoidosis and single small fibrous and atheromatous plaques • Grade III - significantly pronounced atherosclerosis. In addition to lipoidosis, in the arteries on the thickened, wavy and deformed inner membrane there is a large number of small and large, merging fibrous and atheromatous plaques, atherocalcinosis • IV degree - pronounced atherosclerosis. On the thickened and deformed tuberous inner lining of the arteries there are numerous fibrous and atheromatous plaques with calcification and ulcerations.
The clinical picture varies depending on the predominant localization and extent of the process and in most cases is determined by the manifestations and consequences of tissue or organ ischemia.
• Atherosclerosis of the thoracic aorta •• Aortalgia (lasting up to several hours or days, periodically weakens and intensifies) •• Difficulty in swallowing due to compression of the esophagus •• Hoarseness due to compression of the recurrent laryngeal nerve •• Increased area of percussion dullness of the vascular bundle •• Systolic murmur • • Gradually increasing, predominantly systolic, arterial hypertension •• Accent of the second tone at the fifth point and above the aortic bifurcation •• Signs of moderate hypertrophy of the left ventricle •• Increased speed of propagation of the pulse wave on the tachogram •• Linear calcifications in the walls of the aortic arch on radiographs (in the lateral projections) is the most demonstrative, although late, diagnostic sign.
• Atherosclerosis of the abdominal aorta •• Abdominal pain of various localizations •• Linear calcifications in the area of the aortic bifurcation •• Leriche syndrome with damage to the terminal part of the abdominal aorta (thrombosis of the bifurcation area with acute disturbance of the blood supply to the lower extremities) ••• Intermittent claudication ••• Impairment sensitivity and movement in both legs ••• Pallor of the skin ••• Impotence ••• Systolic murmur over the femoral artery ••• Gangrene of the limb may occur.
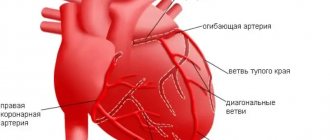
• Atherosclerosis of the coronary arteries.
• Atherosclerosis of the mesenteric arteries (see Atherosclerosis of the mesenteric arteries).
• Atherosclerosis of the renal arteries •• Vasorenal arterial hypertension resulting in arteriosclerotic nephrosclerosis and chronic renal failure •• Systolic murmur over the renal arteries.
• Atherosclerosis of the carotid arteries •• Murmur in the projection of the internal carotid artery •• High risk of stroke with severe hemodynamic disturbances and/or progression of stenosis.
• Atherosclerosis of peripheral arteries (see Atherosclerosis of peripheral arteries).
Laboratory Tests • Hypercholesterolemia • Hypertriglyceridemia • Increased LDL and very low density lipoprotein (VLDL) • Decreased HDL.
Special studies • Angiography • Dopplerography • Radionuclide research methods.
TREATMENT
The regimen is outpatient until complications develop.
Diet No. 10c • Fats: total amount - less than 30% of the total energy value of food; animal fats with a high content of saturated fatty acids - less than 7% • Carbohydrates - 50-60%, increased plant fiber content (fruits, vegetables) • Proteins - 10-20% • Cholesterol - less than 200 mg • Salt - 1650-2400 mg • Regular consumption of small amounts of alcohol can increase HDL levels.
Physical activity. Physical exercise for at least 30 minutes 3 times a week, active lifestyle.
Drug therapy
• Lipid-lowering drugs - with elevated cholesterol levels and signs of coronary heart disease and other diseases caused by atherosclerosis (secondary prevention), as well as in the absence of signs of coronary artery disease (primary prevention).
• Indications for starting drug therapy •• For primary prevention after 6 months of dietary therapy with an LDL cholesterol level of 190 mg% or more in the presence of at least one risk factor, a reduction to a level of 160 mg% is indicated; with an LDL cholesterol level of 160 mg% or more in the presence of two or more risk factors - reduction to a concentration of less than 130 mg% •• For secondary prevention after 6-12 months of dietary therapy for coronary artery disease and an LDL concentration of more than 130 mg% - reduction to a level of 100 mg% or less.
• Tactics of drug therapy •• After starting to take a lipid-lowering drug, the concentration of LDL should be determined after 4, 6 weeks, and then after 3 months •• If therapy is adequate (the desired level of LDL and triglycerides is achieved), repeated examinations are necessary every 4 months or more often for identifying possible side effects and subsequent possible changes in treatment tactics. With very long-term treatment, repeated examinations can be carried out in the future once a year if the drugs are well tolerated •• In case of inadequate therapy, the drug should be changed or a combination of drugs should be prescribed, for example, bile acid sequestrants with nicotinic acid or a statin, a statin with nicotinic acid •• If suspected for genetically determined dislipoproteinemia, controlled long-term therapy is prescribed with individually selected most effective lipid-lowering drugs • Duration of treatment: several years or throughout life.
• Basic lipid-lowering drugs
•• Statins (3-hydroxy-3-methyl-glutaryl-CoA reductase inhibitors) - fluvastatin, lovastatin, pravastatin or simvastatin 20-80 mg/day (preferably in the evening), in one or more doses with meals - reduce LDL concentrations , LDL, cholesterol. Most patients with familial hypercholesterolemia are resistant to statins. In cases of resistance to statins and concomitant triglyceridemia, statins are combined with other lipid-lowering drugs.
•• Nicotinic acid, starting at 500 mg/day and gradually increasing the dose to 3 g/day in 1-3 doses during or after meals, causes a decrease in the concentration of cholesterol and triglycerides and increases HDL levels.
•• Fibrates - gemfibrozil 300-450 mg 2 times / day (30 minutes before breakfast and dinner) - reduce the concentration of triglycerides and VLDL and increase HDL. Due to the fact that fibrates do not reduce LDL levels, they are not considered to be the most effective drugs.
•• Probucol 500 mg 2 times a day - moderately reduces the concentration of LDL and (!) HDL.
Complications account for 1/2 of all deaths and 1/3 of deaths in people aged 35–65 years • Angina • Myocardial infarction • Symptomatic renovascular hypertension • Heart failure • Stroke • Heart rhythm disturbances • Chronic renal failure • Dissecting aortic aneurysm • Arterial thrombosis and embolism • Sudden death.
The prognosis is uncertain. Working ability depends on the functional safety of organs and systems with affected arteries. Eliminating risk factors and increasing the cultural level of the population (as the US experience shows) can significantly reduce mortality rates.
ICD-10 • I70 Atherosclerosis • I67.2 Cerebral atherosclerosis
Note. With deficiency of the cholesteryl ester transfer protein (*118470, 16q21, CETP, r gene), the development of age-related atherosclerotic changes is significantly slowed down and life expectancy increases (the gene defect is common among the Japanese). Laboratory: low levels of LDL and triglycerides, high levels of HDL.
Clinical manifestations, classification of the disease
Symptoms of obliterating atherosclerosis depend on the degree of vasoconstriction and the severity of the disease. In accordance with these signs, clinical stages are distinguished.
Initial (asymptomatic) - from the name it is clear that the patient does not present any complaints, considers himself a healthy person, but a blood test reveals an increase in lipid levels.
Stage of primary signs. The following symptoms are of concern:
- numbness (patients say “as if my leg was sitting”);
- constant chilliness of the feet;
- rarely – muscle cramps;
- unexpressed pain in the legs.
Stage of clinical manifestations. Complaints:
- severe pain in the legs, worsening when walking and causing limping;
- the skin on the feet and legs is pale and cold;
- ulcers or non-healing wounds on the toes may appear.
Unlike endarteritis (thrombangitis), there is no such pronounced intermittent claudication, the pain is constant.
Stage of trophic disturbances. Manifestations:
- severe pain;
- atrophy of the muscles of the leg and thigh;
- trophic ulcers on the feet;
- the onset of gangrene.
The symmetry of the lesion is more typical of atherosclerosis
How does atherosclerosis of the coronary vessels manifest?
The atherosclerotic process can begin at a young age and last for decades, only with a combination of predisposing factors and a narrowing of the lumen of the vessel by half or more, can it make itself felt with the following conditions:
- stable and unstable angina. Characterized by cardiac and chest pain, shortness of breath when moving, and in the advanced stage and at rest, the heart works intermittently;
- myocardial infarction. Gives unbearable chest pain, pronounced fear of death, a sharp drop in blood pressure, reaching shock. The severity of the consequences depends on the location and size of the dead zone. The damaged part of the heart will no longer be able to recover.
The destruction of the arteries supplying the heart can be asymptomatic for a long time and the person will not complain of any abnormalities, which is why it is so important to undergo annual examinations and tests.
Diagnostics
Diagnosis of different stages of the disease usually does not cause difficulties for the doctor. Cold sweaty foot, decreased pulsation in the dorsal artery, muscle atrophy and trophic changes are beyond doubt.
In the clinic, therapists together with surgeons deal with the problems of atherosclerotic lesions of the blood vessels of the legs. For consultation, referral to a vascular surgery center or department is possible.
In addition to blood tests for cholesterol and lipoproteins, as well as glucose levels, the doctor needs to assess the degree of patency of the arteries.
For this use:
- angiography with the introduction of a contrast agent into the femoral artery - the technique is performed in a hospital setting;
- Vascular ultrasound, Doppler ultrasound in the clinic.
It is necessary to differentiate the diagnosis with obliterating endarteritis, Raynaud's disease, Monkeberg's disease, and sciatic nerve neuritis.
In the picture a) the radiograph shows the branches of the arteries below the knee on the right leg, color Doppler sonography b), taken from the front and back, confirms the obstruction of the vessels from the level of the middle of the shin on the left leg (S)
Raynaud's disease is more characterized by a paroxysmal nature and damage to the hands. Monckeberg's sclerosis is a rare genetic disease in which calcification of not only the peripheral but also the coronary arteries rapidly develops.
With neuritis of the sciatic nerve, the pain is shooting in nature, radiating along the outer surface of the thigh through the lower leg to the big toe. Positive symptoms of tension (Lassegue), pathological knee reflexes, increased pain when moving the spine, bending forward, and palpation at the nerve exit points are detected. There are no pulsation disorders in the arteries of the foot.
Complications
The main complication is acute or chronic vascular insufficiency of one or another internal organ. It leads to the gradual death or degeneration of part of its tissues. These phenomena are caused by a lack of oxygen and nutrients. Connective tissue grows in the organ, and sclerotic processes develop.
The second important complication is acute blockage of a vessel by an overgrown atherosclerotic plaque or its detached part - a thrombus. Consequences – acute organ ischemia, myocardial infarction.
At the site of plaque formation, an aneurysm may occur - a vascular formation in which the walls of the vessel bulge and become thinner. An increase in blood pressure caused by physical or psychological stress can provoke aneurysm rupture and intense internal bleeding.
In addition, certain types of pathology cause various complications:
- atherosclerosis of cerebral vessels - stroke, memory loss, dementia;
- atherosclerosis of heart vessels - angina pectoris, arrhythmia;
- atherosclerosis of mesenteric arteries – intestinal necrosis;
- atherosclerosis of the renal arteries - problems with urination and impotence;
- atherosclerosis of the arteries of the lower extremities - trophic ulcers, gangrene.
Treatment
Treatment of obliterating atherosclerosis is carried out taking into account the stage of circulatory disorders. Measures to change lifestyle and diet will be required.
- The patient is required to categorically quit smoking.
- In terms of nutrition, you will have to introduce a low-cholesterol diet with limited consumption of fatty foods, meat, and light carbohydrates.
- It is necessary to observe hygienic foot care (wash your feet twice a day, wipe with a disinfectant solution, change socks more often).
- You should wear comfortable loose shoes, use woolen socks for insulation, and avoid hypothermia. Even minor injuries (cuts, calluses, rubbing) can be dangerous.
You can read more about nutrition principles in this article.
The need for warmth is not a whim, but a real need for the patient
Medicines are conservative methods of therapy and are prescribed only by a doctor. They have to:
- cause dilatation of arterial vessels;
- promote the development of collateral (auxiliary) blood circulation;
- prevent further development of atherosclerosis;
- improve microcirculation at the tissue level.
Diagnosis of atherosclerosis
If there are signs of atherosclerosis of the brachiocephalic arteries, a person is usually prescribed a number of different diagnostic procedures, through which doctors can assess the stage, and, in addition, the severity of the existing pathology. First of all, for these purposes, ultrasound examination of the relevant arteries is performed. In addition, patients are prescribed Doppler examination of blood vessels.
Such methods make it possible to assess the degree of narrowing of the lumen, the size of plaques, and the speed of blood flow. Establishing an assessment of these indicators allows specialists to select the optimal treatment for each patient individually.
When is the use of conservative methods justified?
Vascular surgeons warn about the danger of delaying conservative methods in the presence of severe obliteration of blood vessels and the threat of trophic changes and gangrene.
A course of drug therapy is allowed for:
- stages of chronic arterial insufficiency;
- accompanying severe diseases (myocardial and cerebral ischemia, diabetes mellitus, chronic kidney and lung diseases);
- multilevel vascular lesions with occlusion of the main and terminal arteries.
Variable factors
The development of all types of disease is influenced by our lifestyle. In order to reduce risks as much as possible, you should:
- move more and exercise;
- do not abuse fatty foods;
- try not to expose yourself to stress;
- give up alcohol and smoking.
Potentially correctable causes include:
- diabetes mellitus (glucose levels must be monitored);
- arterial hypertension (pressure);
- hypercholesterolemia (cholesterol levels);
- obesity (waist more than 102 cm in men and more than 88 cm in women);
- frequent infections and intoxications.
Medicines and their action
To relieve pain, use:
- painkillers;
- novocaine blockades (intraarterial, paravertebral at the level of 2–3 lumbar vertebrae).
Vasospasm is relieved with No-shpa, Halidor, Nicotinic acid, Hexonium.
To prevent thrombosis, Trental, Pentoxifyline, Agapurin, and the aspirin group are used.
In hospital settings, Trental is administered intravenously by drip, then tablets are prescribed in a maintenance dosage
Indirect anticoagulants (reduced blood clotting) are prescribed.
You can stimulate metabolism in tissues with vitamins, Solcoseryl, Parmidine, Prodectin.
The antioxidant effects of vitamins A, C, E, and Probuctol are used.
To restore protective forces, immunomodulatory drugs, ultraviolet irradiation of blood, and hemosorption are used.
Taking into account the autoimmune component in the pathology, desensitizing drugs are prescribed (Pipolfen, Diphenhydramine, Loratadine).
If the diet continues to maintain high levels of lipids in the blood, medications are prescribed to eliminate excess cholesterol.
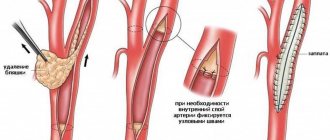
This is what a removed blood clot looks like along with cholesterol plaques during atherectomy surgery
Surgical methods of treatment
If success with conservative therapy has not been achieved, the level of cholesterol in the blood exceeds 7.5 mmol/l, then angiosurgeons routinely offer:
- performing bypass surgery (creating a bypass for blood flow);
- vascular plastic surgery with removal and replacement with a segment of one’s own vein or alloplast;
- installation of a stent in an artery.
These techniques help restore blood circulation in the affected limb.
In case of severe changes, tissue necrosis, gangrene of the fingers, emergency amputation of the limb is necessary. The level of amputation is determined by the pattern of preserved vessels on the angiogram.
The severe consequences of the disease require patients to take a responsible attitude towards their health. Any pain symptoms in the legs should be consulted with a specialist. Treatment cannot be delayed.
Atherosclerosis of the mesenteric arteries
Mesenteric arteries are responsible for the blood supply to the intestines, and the formation of atherosclerotic plaques in them leads to serious digestive disorders. As a result, the blood supply needs of the gastrointestinal tract cannot be satisfied.
The signs of vascular atherosclerosis in this case are quite obvious:
- pain in the upper abdomen;
- bloating, constipation, belching;
- nausea and vomiting with bile;
- retention of stool, gases;
- blood in the stool.
This type (popularly called abdominal toad) is similar in symptoms to peptic ulcers, but the pain goes away faster, especially if you take nitroglycerin, and is not relieved with soda. The pain can wander in different areas of the abdomen, often concentrating around the navel. Patients note a general deterioration in their condition, a slight increase in temperature.
Complications include thrombosis of mesenteric vessels, intestinal gangrene with signs of peritonitis.