Detailed description of the study
Thrombin is one of the key enzymes that influences the regulation of the blood coagulation system. It determines the stabilization of the blood clot, which is important for stopping bleeding. Changes in serum thrombin concentrations may reflect abnormalities in blood clotting (hemostasis). Thrombin is the main link in the last stage of coagulation (blood clot formation). The length of time required for a blood clot to form is called “thrombin time.”
Many components are involved in the formation of a blood clot, and the process itself takes place in several stages. At the final stage, fibrinogen dissolved in the blood plasma is converted into fibrin under the influence of thrombin, which stabilizes the blood clot.
This stage consists of three successive steps:
- First, thrombin cleaves parts (fibrinopeptides) A and B from fibrinogen;
- The remaining fibrin strands join together and form soluble complexes;
- Soluble complexes are converted into insoluble ones thanks to thrombin (it activates blood coagulation factor XIII and the enzyme plasma transglutaminase).
Insoluble fibrin is a more stable form that is practically indestructible.
The most common pathologies at the final stage of coagulation are various structural changes in the fibrinogen molecule, as well as changes in its functions. In the case of functional changes, they speak of dysfibrinogenemia (DFG).
Characteristic laboratory signs determined for dysfibrinogenemia:
- An extension of the final stage is observed, namely an extension of thrombin time, this is the main symptom characterizing such conditions;
- Increased platelet aggregation.
At the same time, the concentration of fibrinogen in the blood plasma remains within normal limits, and also does not change pathologically:
- APTT (activated partial thromboplastin time) is the period of time during which a blood clot forms);
- the amount of RFMC (soluble fibrinogen-monomer complexes, which are particles of blood clots);
- Concentration of D-dimers (fibrin breakdown products, which are determined in the blood after the breakdown of a blood clot).
Most often, dysfibrinogenemia develops against the background of acute and chronic liver diseases; hereditary pathologies are rare. Hereditary variants of disorders of the structure of fibrinogen and its functions: afibrinogenemia (complete absence of fibrinogen in plasma) and hypofibrinogenemia (the minimum amount of fibrinogen required for coagulation processes).
Clinical signs of decreased fibrinogen levels are increased bleeding or a tendency to thrombosis.
Patients usually complain of:
- Heavy bleeding that is difficult to stop;
- Poor wound healing;
- Menorrhagia (the amount of blood released during menstruation exceeds the norm);
- Spontaneous appearance of hematomas;
- Rash.
Most often, a person does not suspect the presence of hemostasis pathology for a long time, and dysfibrinogenemia is determined by chance among other laboratory tests or in preparation for surgery.
As a rule, a test to determine thrombin time is performed during anticoagulant therapy, as well as in women with pregnancy pathologies.
This is a laboratory test that detects quantitative and qualitative changes in fibrinogen.
Synonyms Russian
TV, antithrombin I.
English synonyms
Thrombin time, TT, Thrombin Clotting Time, TCT, antithrombin I, AT I.
Research method
Side scatter detection method, end point percentage determination.
Units
Sec. (second).
What biomaterial can be used for research?
Venous blood.
How to properly prepare for research?
- Do not eat for 12 hours before the test.
- Avoid physical and emotional stress and do not smoke for 30 minutes before the test.
General information about the study
Thrombin time is the time required for the formation of a fibrin clot when thrombin is added to the plasma - an enzyme (factor IIa), which appears as a result of the interaction of blood coagulation factors when a vessel is damaged. Thrombin is necessary for the final stage of the coagulation cascade - the transformation of the fibrinogen molecule into insoluble fibrin, which is able to polymerize and form a stable fibrin clot, which stops bleeding when small and medium-sized vessels are damaged and contains, in addition to fibrin polymers, cellular elements - platelets and erythrocytes. Qualitative or quantitative changes in fibrinogen lead to insufficient/excessive fibrin production, which is manifested by increased bleeding or a tendency to thrombosis. In laboratory conditions, the final stage of the coagulation cascade is reproduced by adding ready-made thrombin to plasma, and changes in the structure or concentration of fibrinogen are reflected in an increase or decrease in thrombin time.
Fibrinogen is a glycoprotein secreted by hepatocytes into the blood. In addition to being a blood clotting factor (factor I), it also provides some reactions of fibrinolysis, the process of dissolving blood clots, binds excess thrombin (therefore fibrinogen is also called antithrombin I) and activates plasminogen. In this regard, diseases with changes in the structure or concentration of fibrinogen can manifest themselves as bleeding, thrombosis, and in some cases a combination of both.
Pathologies that are accompanied by fibrinogen deficiency are called hypo- and afibrinogenemia, and those in which the structure and function of fibrinogen are impaired are called disfibrinogenemia. They can be hereditary or acquired. Acquired diseases include liver disease, disseminated intravascular coagulation (DIC), primary fibrinolysis, and drug reactions (eg, thrombolytic agents and L-asparaginase).
The most common cause of acquired dysfibrinogenemia is liver disease. In cirrhosis, chronic active hepatitis, acute liver failure, obstructive liver disease and hepatoma, too much sialic acid is added to the secreted fibrinogen. This modified fibrinogen has a greater negative charge, which prevents the polymerization of fibrin molecules. Patients with liver disease have multiple coagulation disorders that manifest as increased bleeding. Determination of thrombin time is the main screening test to suspect dysfibrinogenemia as one of the causes of bleeding. Abnormal fibrinogen is also produced by some tumors (some forms of squamous cell carcinoma of the cervix, adenocarcinoma of the breast, hypernephroma, hepatoma). In certain diseases accompanied by the synthesis of antibodies that interact with fibrinogen (systemic lupus erythematosus, multiple myeloma), its activity decreases, which is manifested by an increase in thrombin time.
The most common cause of acquired hypofibrinogenemia is DIC syndrome, a systemic thrombohemorrhagic disorder in which excessive formation of fibrin microthrombi and consumption of blood coagulation factors and platelets occurs. DIC always develops secondarily as a complication of any disease. There are acute and chronic DIC syndrome. The causes of acute DIC are infectious diseases (E. coli - sepsis, HIV, cytomegalovirus infection, malaria), acute myeloblastic leukemia, complications of pregnancy and childbirth (premature placental abruption, eclampsia, amniotic fluid embolism), extensive burns, massive blood transfusions and others . Causes of chronic DIC syndrome: solid tumors, chronic leukemia, pregnancy complications (intrauterine fetal death), myeloproliferative diseases, rheumatoid arthritis and Raynaud's disease, myocardial infarction, nonspecific ulcerative colitis and Crohn's disease, etc. “Triggers” the development of DIC syndrome in all In the listed conditions, a large amount of thromboplastin (tissue factor, factor III) enters the blood. At the same time, multiple microthrombi are formed in the vessels of the kidneys, brain, liver, and lungs, which determine the clinical picture of the syndrome in the form of multiple organ failure. As a result of massive consumption of fibrinogen and other blood coagulation factors, their secondary insufficiency develops and hypercoagulation is replaced by hypocoagulation and disseminated bleeding. It should be noted that hypercoagulation and hypocoagulation are often present simultaneously in the same patient, so the identification of successive periods of DIC is very arbitrary. The peculiarities of the clinical picture of DIC syndrome lead to the fact that the diagnosis of this condition remains one of the most difficult tasks of modern medicine. In this situation, monitoring thrombin time in combination with other laboratory tests is necessary to assess the risk and early diagnosis of DIC, as well as at the stage of monitoring its treatment.
Inherited fibrinogen disorders are quite rare. About 80 mutations are known to cause fibrinogen deficiency or absence. As a rule, such mutations lead to a complete stop in fibrinogen synthesis or the formation of altered fibrinogen, which cannot be secreted from hepatocytes and accumulates in them. With afibrinogenemia, there is no fibrinogen in the plasma; this is the most severe form of its deficiency. The disease is inherited in an autosomal recessive manner and occurs with a frequency of 1:1,000,000. As a rule, afibrinogenemia manifests itself already in the neonatal period (the first 28 days from birth). In this case, bleeding is observed when crossing the umbilical cord, hemorrhages in the skin, gastrointestinal and genitourinary tract, and intracranial hemorrhage. However, this disease may first appear later, in childhood and even in adulthood. Women with afibrinogenemia are characterized by metro-, menorrhagia, habitual spontaneous miscarriage, and bleeding in the postpartum period. In some patients with afibrinogenemia, along with increased bleeding, symptoms of thrombosis (more often venous than arterial) are observed.
Hypofibrinogenemia is much more common than afibrinogenemia (1:500). As a rule, it is asymptomatic, since the amount of fibrinogen that is still present is enough to stop minor bleeding from small and medium-sized vessels and carry the pregnancy to term. However, with extensive injuries, operations, as well as with concomitant pathology of blood coagulation, hypofibrinogenemia can be accompanied by life-threatening bleeding.
Hereditary dysfibrinogenemia is a heterogeneous group of diseases in which the structure of fibrinogen is disrupted. However, its plasma concentration remains normal or slightly reduced (hypodysfibrinogenemia). To date, about 400 mutations are known that lead to amino acid substitutions in the fibrinogen sequence. Such a replacement leads to a decrease in its activity, disruption of its interaction with thrombin, or the absence of further polymerization of fibrin. The majority of patients with dysfibrinogenemia (55%) do not have clinical manifestations of the disease. The disease is suspected on the basis of incidentally detected abnormalities in laboratory tests or when a diagnosis is made in one of the family members. 25% of patients with dysfibrinogenemia experience episodes of increased bleeding (usually after injury, surgery or in the postpartum period), 20% have a tendency to thrombosis (more often venous than arterial), and 27% have a combination of both conditions. In some cases, abnormal fibrinogen is deposited in the kidney tissue as amyloid. This form of hereditary amyloidosis is characterized by the early development of chronic renal failure.
While the main function of fibrinogen is the formation of fibrin thrombus, it is also involved in several other processes: inflammation, angiogenesis and wound healing. In addition, it is believed to promote the formation of atherosclerotic plaques in blood vessels, the proliferation of smooth muscle cells and the uptake of oxidized lipids by macrophages. It has been established that high concentrations of fibrinogen in the blood are associated with an increased risk of arterial thrombosis.
What is the research used for?
- For the diagnosis of acquired dysfibrinogenemia (in liver diseases, autoimmune diseases).
- For the diagnosis of hereditary dysfibrinogenemia.
- To find out the cause of recurrent miscarriage.
- To assess the risk of developing DIC, diagnose it and monitor its treatment.
- To assess the risk of arterial thrombosis.
When is the study scheduled?
- For liver diseases: cirrhosis, chronic active hepatitis, obstructive liver diseases, hepatomas.
- For symptoms of hypo(a)fibrinogenemia and dysfibrinogenemia: increased bleeding (metro-, menorrhagia, nosebleeds, soft tissue hematomas, bleeding in the postpartum or postoperative period) or a tendency to thrombosis (phlebothrombosis, thromboembolism of the branches of the pulmonary artery, arterial thrombosis), as well as with a combination of both conditions.
- With two or more spontaneous abortions up to 22 weeks.
- For diseases accompanied by a high risk of developing DIC: severe infectious diseases, acute and chronic leukemia, complications of pregnancy and childbirth, severe autoimmune diseases.
- With existing risk factors for arterial thrombosis: high concentrations of homocysteine and C-reactive protein.
What do the results mean?
Reference values: 14 - 21 sec.
Reasons for increasing thrombin time:
- liver cirrhosis, chronic active hepatitis, hepatoma;
- DIC syndrome;
- hereditary hypo(a)fibrinogenemia and dysfibrinogenemia;
- acute leukemia, polycythemia vera;
- amyloidosis;
- complications of pregnancy and childbirth (eclampsia, premature placental abruption);
- drug interactions: L-asparaginase, heparin, streptokinase, urokinase.
Reasons for decreased thrombin time:
- thrombocytosis.
What can influence the result?
- Transfusion of fresh frozen plasma masks qualitative and quantitative fibrinogen abnormalities.
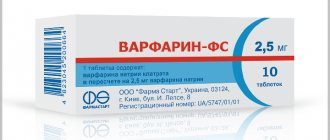
- Therapy with unfractionated heparin leads to an increase in thrombin time.
References
- Clinical guidelines for the diagnosis and treatment of rare blood clotting disorders: hereditary deficiency of factors X, II, VII, 2021.
- Volkova, P.O., Zolotavina M.L., Didenko S.N. and others. Dependence of polymorphism of blood coagulation genes and blood group and rhesus affiliations in women. — Scientific almanac, 2021. — No. 1-2(15). — P.455-458.
- Sturov, V.G., Plyushkin, V.A., Anmut, S.Ya. and others. The final stage of blood coagulation: modern clinical and laboratory diagnosis of dysfibrinogenemia syndrome. - Thrombosis, hemostasis and rheology, 2008. - No. 2 (34). — P.8-15.
- Undas, A. Determination of fibrinogen and thrombin time (TT). — Methods in molecular biology, 2021.
Prothrombin time during pregnancy
Monitoring the clotting rate is important during pregnancy, especially when taking medications that affect clotting. The normal rate for pregnant women is considered to be a clotting rate of 18-25 seconds.
Deviation from the norm can lead to complications during pregnancy, the most dangerous of which is DIC syndrome (disseminated intravascular coagulation). In pregnant women it occurs for two reasons:
- placental abruption, accompanied by bleeding;
- amniotic fluid embolism;
- endometritis.
Often, pregnancy ends spontaneously as a result of antiphospholipid syndrome, which causes blood clots to form in the arteries and veins. These deviations lead to disruption of intrauterine development.
Indications
- Identification of defective forms of fibrinogen or its deficiency (congenital/acquired);
- Diagnosis of hyper- and hypofibrinogenemia;
- The presence of fibrinogen and fibrin breakdown products in the blood;
- Diagnosis and treatment of DIC syndrome;
- Dysfunction or pathology of the liver structure;
- Pain in the liver area of unknown etiology;
- Deviations of pressure inside the vessels in one direction or another;
- Monitoring treatment with anticoagulants (heparin), thrombolytics and fibrinolytics;
- Pregnancy (pathological, spontaneous termination);
- As part of a comprehensive coagulogram.
A coagulogram test is prescribed and its results are interpreted by doctors: hematologist, resuscitator, anesthesiologist, gynecologist, pediatrician, therapist, etc.
How to prepare for a thrombin time test
The analysis does not require special preparation. It is recommended to donate blood on an empty stomach, in the first half of the day; you are allowed to drink only clean, still water. To ensure that the results are not distorted, it is recommended not to drink alcohol or fatty foods the day before the analysis, and also to avoid physical and emotional stress. If you are taking blood thinning medications, you need to notify the clinic representative about this, he will note the data in the client’s card.
The best solution is to analyze the entire blood coagulation system: in addition to thrombin time, it is also recommended to take prothrombin time, fibrinogen and APTT. These indicators are basic and allow you to evaluate the curtailment process from all possible angles.
Blood is taken from a vein: specialists from the Evermedic medical laboratory perform the manipulations as carefully and quickly as possible, even if the veins are thin and deep. The research is carried out in a modern, equipped laboratory with powerful microscopes, so the results are ready within the first 24 hours. They can be received either in person or by email.
Complexes with this research
Coagulogram Study of the functional state of hemostasis 2,080 ₽ Composition
Entry into IVF Examination when a woman enters the IVF procedure 23,500 ₽ Composition
Examination during pregnancy. 3rd trimester 9,840 ₽ Composition
IN OTHER COMPLEXES
- Female infertility RUB 16,470
- Examination during pregnancy. 1st trimester 17,040 RUR
- Pregnancy planning. Clinical indicators 6,800 ₽
- Extended coagulogram RUB 4,230
- Miscarriage RUB 40,440