Thrombin is one of the main enzymes involved in the regulation of the blood coagulation system. It is responsible for stabilizing the blood clot, which is vital during bleeding. When the amount of thrombin in the blood changes, clotting problems and hemostasis may occur, because thrombin is responsible specifically for the stage of blood clot formation. The time it takes for a clot to form under real conditions is called thrombin time.
Thrombin time in the laboratory is the period during which fibrinogen is converted into fibrin in plasma mixed with sodium citrate, calcium and thrombin. There may be several indications for prescribing an analysis:
- for liver pathologies;
- to identify a lack of fibrinogen in the body;
- to monitor heparin treatment;
- before operations and surgical interventions;
- with spontaneous termination of pregnancy up to 20 weeks.
Clinical signs of insufficient fibrinogen are increased bleeding and a tendency to form blood clots. Patients usually report the following symptoms:
- slow healing of the skin surface;
- heavy bleeding (including heavy menstruation);
- frequent occurrence of hematomas;
- rash.
Purpose of determining prothrombin time
The process is controlled by the protein prothrombin circulating in the plasma. Normal synthesis of this substance is possible only in the absence of vitamin K deficiency in the body.
In healthy men and women, prothrombin in the bloodstream is stable; an active surge in the concentration of the substance occurs only after contact with deformed tissues. The indicator is determined during a blood test. In practice it matters:
- PTI – prothrombin index: the ratio of normal prothrombin time to the test blood sample;
- INR (international normalized ratio) is a decoding of test results from any laboratory in the world based on any diagnostic methods.
Prothrombin time is determined to:
- determination of blood viscosity while taking antiplatelet agents or anticoagulants (Aspirin, Warfarin, Clopidogrel);
- research into the effectiveness and adequacy of treatment;
- assessing a woman’s health status when planning pregnancy;
- identifying the causes of liver dysfunction;
- diagnosis of vascular pathologies to prevent stroke, heart attack, early diagnosis of aneurysm;
- determination of vitamin K levels;
- prevention of thrombosis;
- hemophilia control;
- control of disseminated vascular coagulation syndrome;
- detection of anemia in chronic form;
- monitoring dysfunction of homeostasis.
The analysis is carried out by taking blood from a vein or finger and examining the material on an automatic analyzer. Despite its simplicity, this is an informative technique. It is suitable for accurate diagnosis.
Hemostasiogram (screening)
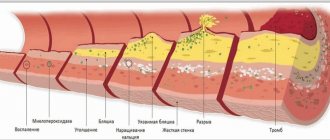
Hemostasis is the stopping of bleeding caused by damage to the vessel wall. Violation of its integrity can occur due to:
- physical impact;
- action of hemodynamic factors;
- exposure to chemicals;
- metabolic disorders;
- inflammatory process;
- actions of immune complexes;
- various diseases, etc.
The hemostasis system is a functional system of the body that is responsible for ensuring the constancy of its internal environment, preventing and stopping bleeding, dissolving blood clots that have completed their task, maintaining circulating blood in a liquid state, and normal resistance of the walls of microvessels. The hemostasis system is involved in the healing process of damaged tissues, in inflammatory processes, regulation of local blood flow and transcapillary exchange.
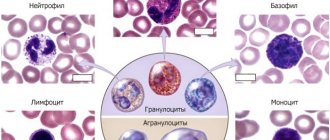
The hemostasis system includes two links - coagulation and anticoagulation, on the interaction and balance of which its functionality depends. Its structural components are:
- coagulation hemostasis;
- platelet-vascular hemostasis;
- anticoagulant system;
- fibrinolytic system;
- complement system, kallikrein-kinin system, proteins, blood plasma lipoproteins.
There are three ways of blood clotting:
- internal - realized exclusively due to enzymes and cofactors present in the blood plasma;
- external - realized as a result of the action of enzymes, blood cofactors + tissue factor (TF - blood coagulation factor III), which is normally absent in the blood;
- general, including the formation of fibrin and its stabilization.
Stopping bleeding takes place in several stages:
- spasm of the vessel wall;
- formation of aggregates by platelets (“white thrombus”);
- blood plasma coagulation (“red thrombus”);
- clot dissolution (fibrinolysis).
The complex study “Hemostasiogram” is a set of tests designed to study the state of the hemostasis system, and includes the determination of the following indicators:
- activated partial thromboplastin time (aPTT, item 512);
- prothrombin according to Quick, prothrombin time, INR (item 605);
- fibrinogen (item 606);
- thrombin time (item 683).
Description of the studied indicators
APTT
APTT (activated partial thromboplastin time) is an indicator whose value reflects the time of formation of a blood clot after the gradual addition of portioned thromboplastins, reagents that trigger the reaction, to the sample of platelet-free citrate plasma with a kaolin-kephalin mixture and calcium chloride. Kaolin, in contact with plasma, stimulates the synthesis of active factor XII - XIIa, providing a surface for the action of high molecular weight kininogen, kallikrein and factor XIIa. The role of phospholipids in this process is the formation of complexes with active factor X (Xa) and prothrombin. After a certain time, CaCl2 is added to the mixture, through which the initiation of coagulation along the internal pathway is simulated.
By determining APTT:
- the functionality of coagulation factors is assessed;
- a deficiency or impaired functionality of such coagulation factors and contact factors of the internal pathway as VIII, IX, XI, XII, prekallikrein, high-molecular kininogens, as well as factors of the general coagulation pathway (including I, II, V, X) is detected;
- The presence of coagulation inhibitors (substances that slow down/inhibit the blood clotting process) is determined.
The duration of the reaction and the time of clot formation are affected by changes in concentration:
- high molecular weight kininogen;
- prekallikrein;
- coagulation factors VIII, XI, XII;
- factors V, X (to a slightly lesser extent);
- prothrombin;
- fibrinogen.
A decrease in clot formation time is an indicator of the risk of thrombosis. A reduction in clot formation time by more than 5 seconds is an indicator of hypercoagulation (blood thickening).
Prolongation of the time of clot formation is a sign of hypocoagulation (a blood clotting disorder in which there is a tendency to repeated bleeding and hemorrhage, both spontaneous and due to injury). The development of hypocoagulation is promoted by:
- deficiency of factors II, V, VIII, IX, X, XI, XII;
- fibrinogen deficiency;
- liver pathologies;
- vitamin K deficiency;
- presence of heparin;
- lupus anticoagulant;
- pathological inhibitors of fibrin polymerization (these can be myeloma proteins, fibrin degradation products, etc.) or other blood clotting inhibitors.
The reason for the prolongation (increase in duration) of the APTT time may be a decrease of 30-40% of the norm in the level of any of the coagulation factors.
APTT reflects the influence of blood coagulation factors on clot formation and is most often performed to:
- determining the effectiveness of the internal blood coagulation pathway;
- monitoring the effectiveness of heparin therapy.
- identifying possible abnormalities in the functioning of the blood coagulation system before surgery in order to avoid subsequent complications;
- diagnosis of a number of blood diseases, liver pathologies that cause disruption of the production of proteins involved in blood clotting;
- diagnosis of DIC syndrome (in combination with other laboratory tests).
Prothrombin according to Quick
Quick prothrombin reflects the activity of the prothrombin complex of the patient's plasma in comparison with the measured prothrombin time of control plasma.
To determine the indicator, a calibration graph of the dependence of prothrombin time on the percentage of prothrombin complex factors is used (factors of the prothrombin complex are blood coagulation factors - II (prothrombin), VII, IX and X, and proteins SI and S, which take part in the activation reactions of precursor proteins leading to the formation of thrombin). Values at different dilutions of control plasma are used to construct the curve.
Prothrombin according to Quick allows you to get the most accurate result, especially in the area of low values, so this method is by far the most used.
Prothrombin time
Prothrombin time is measured in seconds and shows how long it takes for plasma to clot after adding a mixture of thromboplastin and calcium to it. Test results obtained in different laboratories are not suitable for comparison, since they use different equipment and thromboplastin of different activity and origin.
Quick's prothrombin and prothrombin time reflect the presence/absence of a deficiency of clotting factors (prothrombin complex) and the functionality of the extrinsic coagulation pathway (i.e., the ability of blood to form a clot when tissue is damaged). If the quantity and quality of fibrinogen, a soluble plasma protein that is directly involved in the formation of a blood clot (thrombus) after damage to the vessel wall, is normal, then the result of the study will depend on the content of factors II, V, VII, X. It is their presence that determines the activity of prothrombin complex. The liver is responsible for producing these clotting factors, so this test can be used to determine its ability to produce them. This process is directly dependent on the level of vitamin K. Since indirect-acting anticoagulants (ANDA) act as its antagonists, the analysis is also used to monitor treatment using them.
INR
INR (International Normalized Ratio) or in the Latin version of the abbreviation INR (International Normalized Ratio) is an additional method for obtaining the results of a prothrombin test, allowing for monitoring the condition of patients who are taking indirect anticoagulants.
INR is defined as the ratio of the patient's prothrombin time to the normal mean prothrombin time, raised to the power of the International Sensitivity Index (ISI - International Sensitivity Index of thromboplastin).
INR = (patient's prothrombin time/normal mean prothrombin time) ISI
MIC is the sensitivity coefficient of thromboplastin, which brings it to the international standard. INR is essentially a method of mathematical correction by which prothrombin time, measured using thromboplastins with different sensitivities, is standardized.
Reference INR values in various cases depend on the purpose of taking indirect anticoagulants and are determined by the attending physician. The use of indirect anticoagulants can be carried out:
- for the prevention of deep vein thrombosis;
- in the treatment of deep vein thrombosis and pulmonary thromboembolism (acute blockage of a blood vessel by a thrombus);
- with critical ischemia (insufficient blood supply) of the legs;
- for the prevention of thromboembolism in patients with atrial fibrillation (a heart rhythm disorder characterized by chaotic contraction of the muscle fibers of the heart) and heart defects (defects in the structure);
- when installing bioprosthetic heart valves;
- for secondary prevention of myocardial infarction, if the use of aspirin is contraindicated;
- for the prevention of thrombosis in persons with antiphospholipid syndrome (a pathology in which there is an increased production of antibodies to phospholipids - substances that are building materials for cells);
- when installing mechanical prosthetic heart valves.
At the same time, the reference INR values recommended by the World Health Organization are 2-3 for the first six cases, and 2.5-3.5 for the last two.
A significant increase in INR indicates hypocoagulation (tendency to bleeding), which is an indication for reducing the dose of anticoagulants used. An INR value below the established norm indicates that the risk of thrombosis remains increased, is evidence of the ineffectiveness of the treatment used, and is an indication for dose adjustment of the anticoagulant.
INR and prothrombin according to Quick are inversely proportional - the lower the prothrombin according to Quick, the higher the INR.
Fibrinogen
Fibrinogen (according to the international nomenclature - factor I of the blood coagulation system) is a two-component protein (glycoprotein), the molecular weight of which is 340,000 Da. It is an earlier form of fibrin, a protein that forms the basis of a clot when blood clots. Fibrinogen is produced in the liver, from which it then enters the blood with other components involved in blood clotting. The half-life of the protein is about 100 hours. The functions of fibrinogen as a blood clotting factor include:
- ensuring a number of fibrinolysis reactions (the process of dissolving blood clots) due to the binding of excess thrombin (this determines its another name - antithrombin I);
- activation of plasminogen - a circulating inactive proenzyme that is a precursor of the plasmin protein, which plays an important role in fibrinolysis, and, in turn, is a precursor of angiostatin - a protein that suppresses the formation and growth of blood vessels (angiogenesis).
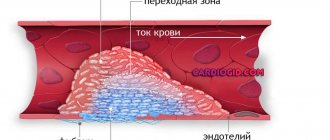
Fibrinogen is converted to fibrin, which is the basis of the blood clot that forms after damage to a blood vessel. The fibrin algorithm consists of the formation of its monomers, polymerization, and stabilization of the clot. As a result of these processes, insoluble fibrin I is formed. Its threads intertwine, forming a kind of framework, which, together with platelets, forms a clot (or thrombus). The blood clot remains in the damaged area until it is completely healed.
When blood clotting factors work correctly and there is a sufficient number of platelets, a stable blood clot is formed. In case of deficiency of factors or their incorrect interaction, thrombosis or bleeding may occur.
Determination of fibrinogen levels is included in a comprehensive analysis of blood clotting indicators. In addition, the study of protein concentration is part of a preoperative examination, prenatal diagnosis (comprehensive prenatal diagnosis, the purpose of which is to identify pathologies in a child during intrauterine development), diagnosis of heart and vascular diseases. It is important to know that an increase in fibrinogen concentration, even within normal limits, can cause a relapse of cardiovascular diseases. In pregnant women, the indicator goes beyond the upper limit for physiological reasons and can reach 6 g/l in the last trimester.
An increased level of fibrinogen does not require special treatment in two cases: during pregnancy and during inflammation, because after stabilizing the body’s condition, it returns to normal levels.
Thrombin time
Thrombin time (TT) is the time period during which fibrinogen is converted into fibrin in citrated plasma with thrombin and calcium introduced into it and a blood clot is formed. The rate of formation of a fibrin clot is directly influenced by the quantity and quality of fibrinogen and the presence of anticoagulants in the blood. This test monitors the final stage of blood clotting.
Thrombin (proteolytic (protein-splitting) enzyme, blood coagulation factor IIa) - is formed when a vessel is damaged as a result of the interaction of other coagulation factors. It is one of the main regulators of the blood coagulation process and the main reagent used in this study. Only under its influence does the conversion of soluble plasma fibrinogen into insoluble fibrin and stabilization of the blood clot occur, which is necessary to stop bleeding.
Blood thickening is a complex process that takes place in several stages involving a number of components. The sequence of blood clot formation is as follows:
- under the influence of thrombin, fibrinopeptides A and B are cleaved from the A alpha and B beta chains of fibrinogen, and fibrin monomer is formed;
- fibrin complexes in the form of filaments are spontaneously formed from fibrin monomer molecules;
- Due to the activation of blood coagulation factor VIII and the plasma transglutaminase enzyme by thrombin, the resulting soluble fibrin complexes become insoluble.
The form of fibrin obtained as a result of the reaction is stable and durable - it practically does not collapse. In addition to polymerized fibrin, the clot also contains blood cells - platelets and erythrocytes.
If the qualitative (structural and functional) or quantitative characteristics of fibrinogen are violated, excessive or insufficient fibrin production occurs, which can cause thrombosis, excessive bleeding, or a combination of both pathologies, and when laboratory tests are performed, prolongation (extension) or reduction of thrombin time.
The most common causes of bleeding disorders are:
- hypo- and afibrinogenemia – pathologies in which fibrinogen deficiency is observed;
- dysfibrinogenemia – pathologies in which the functions and structure of fibrinogen are impaired.
When conducting laboratory tests, characteristic signs of dysfibrinogenemia are:
- prolongation of thrombin time (the main symptom of these conditions);
- increased connection of platelets with each other (their aggregation).
These conditions do not affect the concentration of fibrinogen in the blood. With them, such laboratory parameters as:
- activated partial thromboplastin time;
- the level of soluble fibrinogen-monomer complexes (RFMC - item 681), which are fragments of blood clots;
- the level of D-dimer (position 679), a fibrin breakdown product found in the blood after cleavage of the fibrin network under the influence of plasmin.
The cause of hereditary dysfibrinogenemia may be:
- afibrinogenemia, characterized by the absolute absence of fibrinogen in the blood plasma;
- hypofibrinogenemia, characterized by a small amount of fibrinogen in the blood, but sufficient to carry out the blood clotting process.
As a result of research, about 400 mutations have been identified that cause a structural disorder in which amino acids are replaced in the fibrinogen sequence. With such a replacement, its activity decreases, interaction with thrombin is disrupted, or further polymerization of fibrin is stopped. In more than half of cases, dysfibrinogenemia is asymptomatic. The presence of a pathology is discovered by accidental detection of abnormalities in laboratory tests or by its detection in one of the family members. Cases of increased bleeding are detected in 25% of patients (their cause may be trauma, surgery, or the postpartum period). 20% of patients have a tendency to thrombosis (venous to a greater extent than arterial). In 27% of cases, a combination of both conditions is observed. Another form of hereditary pathology is hereditary amyloidosis, in which fibrinogen is deposited in the kidney tissues in the form of amyloid, leading to acute renal failure.
Acquired dysfibrinogenemia is often caused by liver pathologies:
- cirrhosis;
- chronic active hepatitis;
- acute liver failure;
- obstructive diseases;
- primary hepatocellular liver cancer (hepatocellular carcinoma, hepatoma).
In all of these diseases, an excess amount of sialic acids is added to fibrinogen. The resulting modification of fibrinogen has a significant negative charge, which creates an obstacle to fibrin polymerization.
Improper liver function is the cause of multiple bleeding disorders, manifested by increased bleeding. The thrombin time test can determine whether dysfibrinogenemia is the cause of bleeding.
The production of abnormal fibrinogen is also carried out by some forms of a number of tumors, such as:
- squamous cell carcinoma of the cervix;
- breast adenocarcinoma;
- hypernephroma (kidney cancer);
- hepatoma (liver cancer).
The activity of fibrinogen may decrease in diseases characterized by the formation of antibodies that interact with it (these include, in particular, systemic lupus erythematosus and multiple myeloma). Autoantibodies to fibrinogen or paraproteins (structurally abnormal and functionally defective proteins produced by tumors) also prolong thrombin time because they prevent fibrin monomers from polymerizing.
The most common cause of acquired hypofibrinogenemia (a decrease in the level of the coagulation factor fibrinogen in the blood) is disseminated intravascular coagulation syndrome (DIC syndrome or thrombohemorrhagic syndrome) - a systemic pathological process in which fibrin microthrombi are formed in the microcircular vessels in large quantities, and there is a high consumption of blood factors and platelets. The pathology is characterized by a combination of thrombosis with blood incoagulability, which causes multiple massive hemorrhages. DIC syndrome is not an independent disease. Its development is determined by the complication of other pathologies. DIC syndrome can be acute or chronic. The acute form of the syndrome can develop against the background
a) infectious diseases:
- sepsis caused by Escherichia coli (E. coli);
- human immunodeficiency virus (HIV infection);
- cytomegalovirus infection;
- malaria;
b) acute myeloblastic leukemia;
c) complications of pregnancy and childbirth:
- premature placental abruption;
- eclampsia;
- amniotic fluid embolism;
d) extensive burns;
e) transfusion of large quantities of blood or its components, etc.
Chronic DIC syndrome can develop:
- for solid tumors;
- for chronic leukemia;
- for myeloproliferative diseases;
- for rheumatoid arthritis;
- with Raynaud's disease;
- with Crohn's disease;
- with nonspecific ulcerative colitis;
- with myocardial infarction;
- in case of intrauterine fetal death, etc.
Clinically, a decrease in fibrinogen concentration may manifest itself as a tendency to thrombosis or increased bleeding. For example, pathology may manifest itself:
- difficult to stop heavy bleeding;
- poor wound healing;
- extremely heavy menstruation (menorrhagia);
- spontaneous appearance of bruises;
- rash.
The impetus for the development of DIC syndrome in all of the above pathological conditions is the excessive intake of tissue factor (blood clotting factor III; thromboplastin) into the blood, which causes the formation of multiple microthrombi in the vessels of various organs (in particular, lungs, liver, brain, kidneys) . Their presence leads to dysfunction of body systems and multiple organ failure, which manifests itself clinically. As the syndrome develops, the consumption of fibrinogen and other blood coagulation factors increases significantly, which leads to their deficiency and a change from a state of hypercoagulation (increased blood clotting) to a state of hypocoagulation (reduced coagulation) and massive bleeding. Medical practice shows that patients quite often experience the simultaneous presence of hyper- and hypocoagulation, which makes the division of DIC into periods quite relative, and its diagnosis very difficult. Therefore, determining the thrombin time and conducting other laboratory tests is necessary and important to determine the likelihood of development, early detection and monitoring of the progress of treatment of DIC syndrome.
Extension of clot formation time may indicate:
- low (less than 0.5 g/l) fibrinogen level;
- about the presence of fibrin degradation products in the blood (in DIC syndrome, in the process of restoring blood flow in the vessels, when defective fibrinogen appears in the blood due to hereditary or acquired pathologies).
The time for clot formation also increases in the presence of direct-acting anticoagulants in the blood, such as heparin, which neutralize the effect of thrombin introduced into the plasma. The presence of indirect anticoagulants does not have any effect on the test result.
Valid values
In domestic medicine, the prothrombin time method in seconds is used:
- children - from 14 to 18 seconds;
- adult men and women – from 10 to 15.
In practice, different laboratories use different reagents and therefore obtain different ranges of standards. To standardize the process, the result is assessed within the framework of the INR. In healthy men and women, the normal prothrombin time is the same:
- for a newborn, an interval of 14 to 18 seconds is considered normal;
- for children under six years of age – from 13 to 18;
- for adults – from 15 to 20.
If the analysis is carried out in a technical laboratory, then the optimal value for children is from 70 to 100%, for adults - from 95 to 105%.
The normal prothrombin time in pregnant women depends on the trimester:
- in the first and third trimester – from 0.8 to 1.3;
- in the second – from 0.8 to 1.1.
When using blood thinners, levels can increase to 3.5 units in the INR.
Content
- Indications for the purpose of analysis
- Increased thrombin time
- Changes in indicator during pregnancy
Thrombin time is an indicator that allows us to evaluate the final stage of the blood clotting process (coagulation), namely, the formation of fibrin from fibrinogen. That is, thrombin time is the time during which fibrinogen is converted into fibrin in citrated plasma after the addition of calcium and thrombin. In this case, the rate of formation of a fibrin clot mainly depends on the amount and usefulness of fibrinogen, as well as the presence of anticoagulants in the blood. Thrombin time is used to assess blood anticoagulant activity and identify dysfibrinogenemia.
Increasing the indicator
If the prothrombin time exceeds the norm, this indicates that blood clotting is too slow. It is liquid due to many reasons:
- liver dysfunction as a result of hepatitis, cirrhosis, when hepatocytes are gradually replaced by connective tissue, the synthesis of coagulation factors fades;
- taking medications: anticoagulants, antiplatelet agents (Aspirin, Clopidogrel, Warfarin);
- lack of vitamin K - impaired prothrombin synthesis;
- disturbances in the synthesis of fibrinogen and other clotting factors;
- hereditary pathologies;
- blood transfusions;
- hormonal imbalance;
- diabetes mellitus;
- tumor growth.
Indications for the purpose of analysis
- determination of fibrinogen deficiency or deficiency;
- monitoring the results of therapy with heparin, thrombolytic or fibrinolytic drugs;
- assessment of the patient’s condition with DIC syndrome;
- liver pathology;
- detection of the presence of fibrinogen/fibrin degradation products in the blood;
- in the presence of two spontaneous cases of pregnancy termination before 22 weeks.
Thrombin time depends on the level of fibrinogen in the blood: a decrease in the level of fibrinogen increases thrombin time and for this reason, the analysis of thrombin time is usually combined with the analysis of fibrinogen, as well as other coagulogram indicators. Thrombin time - the norm is 15-18 seconds. However, in various diseases, the thrombin time indicator goes beyond the normal range - the thrombin time is increased or decreased)
Preparing and conducting analysis
No special preparation is required for the test. To increase the reliability and accuracy of the testing, a couple of days before the upcoming manipulation you need to give up green tea, soy, liver, cabbage of any kind, leafy vegetables, beans, and alcohol.
Blood sampling for analysis is carried out in a laboratory in compliance with all rules of asepsis and antisepsis, on an empty stomach. The sequence is as follows:
- during intravenous sampling, a tourniquet is applied to the forearm to reduce the speed of blood flow and provide convenient access to the vein;
- the injection site is treated with an antiseptic;
- After drawing blood, the tourniquet is removed and the injection site is disinfected.
A blood sample taken from a finger or vein is submitted for testing: the required amount of blood is added to a test tube with sodium citrate so that the blood does not clot. To completely neutralize the effect of the clotting factor, the test sample is centrifuged by adding thromboplastin and calcium chloride. The time of clot formation is recorded - prothrombin time.
Today you can carry out such testing at home using a special analyzer. This is necessary for patients who are being treated with Warfarin against the background of thromboembolism, pre-infarction, when certain fluctuations in PTI or prothrombin time save a person’s life. The analyzer has a simple device and does not require special skills to operate.
References
- Clinical guidelines for the diagnosis and treatment of rare blood clotting disorders: hereditary deficiency of factors X, II, VII, 2021.
- Volkova, P.O., Zolotavina M.L., Didenko S.N. and others. Dependence of polymorphism of blood coagulation genes and blood group and rhesus affiliations in women. — Scientific almanac, 2021. — No. 1-2(15). — P.455-458.
- Sturov, V.G., Plyushkin, V.A., Anmut, S.Ya. and others. The final stage of blood coagulation: modern clinical and laboratory diagnosis of dysfibrinogenemia syndrome. - Thrombosis, hemostasis and rheology, 2008. - No. 2 (34). — P.8-15.
- Undas, A. Determination of fibrinogen and thrombin time (TT). — Methods in molecular biology, 2021.
What affects the accuracy of the result?
In some cases, the analysis result is inaccurate. The following can increase blood clotting time: alcohol, overeating, fatty foods, legumes, vegetables. Medicines reduce PTI: antibiotics, anticoagulants, anabolics, heparin, diuretics, laxatives.
The time period can be shortened by: eating foods rich in vitamin K (cabbage in all varieties, primarily spinach, beef liver), dehydration of various origins, antihistamines, contraceptives, caffeine-containing substances.
Price of a blood test for prothrombin
| Service | Price |
| Prothrombin (according to Quick) + INR | 250 rub. |
| APTT | 190 rub. |
| Thrombin time | 200 rub. |
| Fibrinogen | 190 rub. |
| Antithrombin III | 350 rub. |
| D-dimer | 1100 rub. |
| Protein S | 1700 rub. |
| Protein C Lupus anticoagulant | 1320 rub. |
Therapeutic measures
If the study reveals a decrease in prothrombin time compared to normal
, the patient is prescribed direct-acting anticoagulants (Heparin) or indirect (Warfarin), a special diet is recommended: fatty fish (halibut, herring, mackerel), oatmeal with olive or flaxseed oil, cranberries, figs, blueberries, plums, ginger. Drinks include green tea and cocoa.
When the PTI indicator is higher than normal
, you need to take coagulants or synthetic blood clotting accelerators (Vikasol). Dietary nutrition involves excluding from the diet fatty foods, buckwheat, greens, legumes, red currants, chokeberries, blackberries, wheat baked goods, and smoked meats.
Reduces blood viscosity by drinking clean drinking water in accordance with the age and weight drinking ration (40 ml per 1 kg of weight).
Prothrombin time is an indicator of coagulation, which literally saves a person’s life if determined in a timely manner.
Thrombin time is normal
To measure thrombin time, the following reference values are accepted:
- 10.3 – 16.6 seconds.
Factors influencing the result
Sometimes the results may be distorted. There are a number of reasons for this:
- Age (in newborns, thrombin time is normally prolonged);
- Violations of the rules for preparing for a coagulogram;
- Violations of the algorithm for blood collection, its transportation and storage;
- Incompetence of laboratory workers;
- Taking interfering drugs;
- Transfusion of frozen plasma shortly before the test (hides quantitative and structural fibrinogen abnormalities);
- Menstruation (reduces clotting rates);
- Acute febrile syndrome in a patient during venous blood sampling;
- Recent injuries, wounds, burns, surgery.
Prothrombin according to Quick
The Quick prothrombin test is the most accurate way to analyze the activity of this protein, which leaves the prothrombin index test far behind. This is not the most common type of analysis. As a rule, it is performed during screening tests, in the presence of blood diseases, and also as a monitoring measure when the patient is using anticoagulant drugs. Normally, the Quick prothrombin percentage of 30-40% corresponds to 50-60% of the prothrombin index.
Where to take a prothrombin test in St. Petersburg?
You can get tested for antibodies to prothrombin in St. Petersburg at our MRI center and RIORIT clinic. You can make an appointment and find out the cost of the examination by phone..
MRI and ultrasound center RIORIT
Area:
Kalininsky
Metro:
metro station Grazhdansky Prospekt, metro station Devyatkino, metro station Prospekt Prosveshcheniya
Address:
St. Petersburg, Kalininsky district, st. Rustaveli, 66 lit. G
Telephone:
Equipment:
Siemens, open type
Schedule:
Around the clock
Reasons for the decline
Taking into account the observed shifts, the formal prothrombin index is normally determined by the limit of up to 150%. This also includes some errors during the examination and individual characteristics of the body. Anything less clearly indicates problems.
PTI in the blood decreases as a result of the influence of pathological factors:
- Congenital anomalies in which insufficient fibrin protein is produced. This substance is involved in the binding and aggregation of platelets, its activation is provided by coagulation factors. With pathologies of this kind, the prothromboin index decreases. Depending on the nature of the process and the body’s ability to compensate for the violation.
- Congenital diseases, all forms of coagulopathies.
- Liver disorders. Which are not associated with the destruction of its tissues. These are mainly functional disorders. They are difficult to diagnose using routine tests such as ultrasound. Scintigration is required, laboratory tests may be performed.
- Often, a decrease in the prothrombin index is detected in the process of taking drugs to influence the rheological properties of the blood. Be it Aspirin and its analogues based on acetylsalicylic acid or modern medications for thinning. Especially often, abnormal results are obtained after finishing taking thrombolytics, which have an even more aggressive effect on fluid connective tissue.
- DIC syndrome.
- Other drugs also have a negative effect on the blood. For example, laxatives due to the active removal of fluid from the patient’s body.
It is not recommended to use nicotinic acid for a long time, as well as drugs to suppress the patient’s immune system. Methotrexate is especially aggressive.
Hormonal drugs and anabolic medications manifest themselves in the same way. If problems are detected, the course of therapy should be reconsidered.
If the deviations are purely laboratory in nature and do not manifest themselves objectively, moreover, there is no such tendency, it is possible to continue treatment.
A low prothrombin index indicates excessive blood thinning and prolonged clotting; spontaneous bleeding of varying degrees of intensity is possible.