What is cholesterol
To understand this issue in more detail, you should understand what cholesterol is and why the human body needs it.
Cholesterol is a substance without which the body cannot function normally. It performs a number of important functions:
- Contained in the membranes of all cells of the human body, which makes them more durable and resistant to external influences.
- Participates in the production of essential hormones, including sex hormones.
- Affects choleretic metabolism and fat absorption.
- Helps normalize the functioning of the nervous system, as it is contained in myelin cells that conduct nerve impulses.
Cholesterol is usually divided into “good” and “bad”. “Good” is produced by the human body itself, or more precisely by the liver, and makes up more than 80% of all cholesterol. It is very important for the functioning of all organs and cells. A person receives “bad” cholesterol from the outside, that is, through food.
There is an opinion that to lower blood cholesterol levels it is necessary to reduce the amount of animal fat consumed.
In other videos on Dr. Shishonin’s blog, you can learn more about this topic and find out why this statement is a myth leading to severe forms of atherosclerosis. Important:
Low cholesterol levels are worse than high cholesterol levels in the blood. This may indicate a variety of biochemical problems.
Reduced cholesterol levels
A decrease in cholesterol levels not only indicates internal problems of the body, but also increases the risk of developing various diseases several times. Among them are:
- stroke;
- liver cancer;
- emphysema and asthma;
- alcoholism and drug addiction;
- clinical depression.
There can be many reasons for low blood cholesterol, here are some of them:
- Limiting the consumption of foods containing animal fats. Dr. Shishonin in his blog dispels the myth that vegetarianism is a great way to lower cholesterol and become healthier. This diet can lead to metabolic disorders and abnormal cholesterol levels.
- Liver diseases. As mentioned above, the liver is involved in the production of cholesterol, which is so necessary for the functioning of all systems and organs. If there are problems with it, the balance is upset.
- Genetic predisposition.
- Poisoning.
- Anemia.
- Overactive thyroid gland and many others.
You can find out more information about this and many other important aspects of health related to blood pressure, osteochondrosis, atherosclerosis by becoming a member of the Club of Former Hypertensive Patients
.
Join our community, download gymnastics, which has already helped hundreds of thousands of people overcome blood pressure surges and hypertension. Get the most up-to-date and correct information, ask your questions to Dr. Shishonin and just communicate.
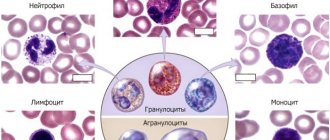
Lipids are organic substances that, together with proteins and carbohydrates, make up the bulk of the body's organic substances. They accumulate in adipose tissue in the form of triglycerides (TG), being the main energy substance. Lipids are part of cell membranes and participate in the synthesis of steroid hormones.
Physiology of lipid metabolism
Lipids without a protein connection are insoluble or poorly soluble in water, but as part of lipoprotein complexes consisting of lipids and proteins, they easily go into solution. In this state, they provide transport of lipids in the plasma for delivery of the latter to the body tissues.
The components of lipids are fatty acids (saturated, monounsaturated, polyunsaturated), triglycerides, free cholesterol (CS), cholesteryl esters (CE), phospholipids (PL, complex lipids).
TG are chemical compounds of glycerol with three molecules of fatty acids. In everyday life they are called fats. When TG is hydrolyzed in adipocytes in the presence of lipoprotein lipase (LPL), fatty acids are released from them, which are used by the body for energy purposes.
Cholesterol (chole - bile, sterol - fatty) is produced in the liver and is used for the construction of cell membranes, the synthesis of steroid hormones and bile acids. In the intestine, bile acids are necessary for the emulsification and absorption of exogenous fat.
The main form of cholesterol circulating in plasma is its esters (cholesterol bound to a fatty acid). They are in the form of highly soluble complexes with transporter proteins. Their formation requires the enzyme lecithin cholesterol acyltransferase (LCAT).
PL are lipids that contain glycerol, fatty acids, phosphoric acid, and nitrogen-containing compounds. They are an integral part of cell membranes.
In the blood, TG, cholesterol, and PL are transformed in the form of lipoproteins (LP), and free, non-fat, non-esterified fatty acids (NEFA) are transformed in the form of complexes with albumin [1].
In the process of ultracentrifugation, individual fractions of drugs are isolated: chylomicrons (CM) - the lightest particles, very low-density lipoproteins (VLDL), transition-density lipoproteins (TDLP), low-density lipoproteins (LDL), high-density lipoproteins (HDL).
The proteins that make up the drug are referred to as apolipoproteins (apo). They are necessary for the transport of various lipids (mainly triglycerides and cholesteryl esters) from sites of synthesis to the cells of peripheral tissues, as well as for the reverse transport of cholesterol to the liver. Apoproteins regulate the activity of enzymes - LCAT, LPL, hepatic triglyceride lipase (TGL).
There are six main classes of apolipoproteins, designated by letters (A, B, C, E, D, H). Their synthesis occurs mainly in the liver and intestines.
The main lipids of chylomicrons are TG, and their structural apoprotein is B48. VLDL consists of 55% TG, 20% cholesterol, and the transport protein is apo-B100.
DILI is formed from VLDL, contains 35% cholesterol and 25% TG and is transported by apo-B100. The LDLP fraction is an intermediate product, a precursor to LDL, which is formed during the conversion of VLDL with the participation of hepatic lipase. It is characterized by a short plasma lifetime and is rapidly metabolized into LDL.
LDL is the end product of VLDL hydrolysis. They are the main carriers of cholesterol to tissues. The half-life is 3–4 days. Approximately 70% of total cholesterol is associated with LDL. LDL catabolism occurs predominantly in peripheral tissues. In humans, 70–80% of LDL is removed from the plasma every day by receptor-mediated pathways. The rest is captured by phagocytic cells of the reticulohistiocytic system. It is believed that this is the main atherogenic lipoprotein. Apo-B100 makes up more than 95% of total LDL protein.
HDL is formed mainly in the liver, but also in the intestine from exogenous lipids. It is a heterogeneous group of molecules with distinct metabolic roles. HDL absorbs free PL cholesterol, which is formed in plasma under the influence of LCAT. High levels of HDL have a protective effect against atherosclerosis. HDL consists of 50% protein apo-A1, apo-E, apo-C, 25% PL, 20% cholesterol and 5% TG.
The formation of a lipid-protein complex occurs through many receptors. Changes in genes encoding apoprotein receptors can disrupt lipoprotein function [2].
A variety of fatty acids in the composition of chemicals are supplied with food, which are processed with the participation of hepatic lipase. The main lipids found in blood plasma are NEFA, PL, TG, cholesterol and EC. In a healthy person, CMs after consuming fats disappear from the blood 12 hours after eating.
An important source of fatty acid formation is carbohydrates. A significant portion of essential fatty acids is synthesized in the liver, less in adipocytes from acetyl-coenzyme A, formed during the conversion of glucose.
Insulin is a potent inhibitor of the activity of hormone-sensitive LPL and, consequently, lipolysis in the liver and adipose tissue. In adipocytes, high levels of glucose and insulin promote the deposition of FFAs in the form of TG. Insulin and glucose also stimulate the biosynthesis of FFAs in the liver when consumed in excess. FFAs are converted into TG with subsequent formation of VLDL. FFAs are captured by various cells and used as energy material, and when in excess they are deposited in the form of triglycerides in tissue.
Energy expenditure (lipolysis) occurs under the control of adrenaline, norepinephrine, glucagon, and adrenocorticotropic hormone (ACTH). The resulting FFAs capture working organs.
The content of cholesterol and TG in the blood plasma can be used to judge the nature of lipoprotein particles. An isolated increase in TG levels indicates an increase in the concentration of cholesterol or VLDL. On the other hand, an isolated increase in cholesterol levels almost always indicates an increase in LDL concentrations. TG and cholesterol levels often increase simultaneously. This may reflect a sharp increase in the concentration of cholesterol and VLDL [1, 2].
Hyperlipidemia
Plasma lipid levels vary among children due to genetic and dietary factors. Hyperlipoproteinemia (dyslipidemia) is a syndrome complex accompanied by excessive levels of lipids and/or lipids in the blood plasma.
Hyperlipidemia (HLP) occurs in 2–10% of children and 40–60% of adults [2]. HLP is an important factor in the development of cardiovascular diseases. LPs of one or more classes may accumulate in the blood due to increased formation or secretion or increased administration of exogenous lipid components or decreased excretion from the body. In some cases, all of these processes take place.
Disturbances in fat metabolism may be associated with changes in proteins involved in fat metabolism (LP, apoproteins) and in the LP receptor apparatus. The mechanism of these disorders may be due to a deficiency or block of apoproteins and LP receptors, which are the most important cofactors of LPL activity and endocytosis by macrophages. The synthesis of LDL receptors is inhibited by glucocorticoids.
GLP is divided into primary (1/3) and secondary (2/3). According to the mechanism of development, HLPs are grouped into nutritional, retention, and transport. In most cases they are combined.
According to the WHO classification, various combinations of drugs, the level of which is elevated in pathology, are divided into six types or categories. Most of them can be caused by various genetic diseases. Types of hyperlipoproteinemia should be considered as evidence of a disorder of lipid metabolism, and not as the name of a specific disease.
Primary SDP
Primary HLP type 1 (familial lipoprotein lipase deficiency) occurs in 1% of cases with autosomal recessive inheritance resulting from a mutation in the LPL gene. The defect is associated with congenital or acquired LPL deficiency. As a result of this disorder, the metabolism of CMs is blocked, which leads to their extreme accumulation in the plasma. With insufficient blood LPL activity, the transition of fatty acids from blood plasma chylomicrons to fat depots is disrupted (TGs are not broken down). The excretion of TG-rich drugs is blocked. Severe triglyceridemia develops.
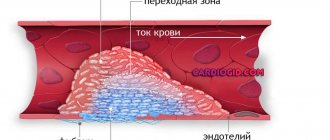
The pathology usually manifests itself in early childhood with recurrent attacks of abdominal pain. They are caused by pancreatitis, which develops due to the formation of toxic products during the partial hydrolysis of TG and PL of chylomicrons. Excess CM can cause microthrombosis in various organs.
In the clinic, patients are found to have yellow papules with an erythematous rim in different areas of the skin and xanthoma as a result of the deposition of large quantities of chylomicron triglycerides in histiocytes. THs are also deposited in phagocytes of the reticulohistiocytic system, causing hepatomegaly, splenomegaly and bone marrow infiltration by foam cells. When examined with an ophthalmoscope, a whitish retina and white vessels in it can be detected, allowing the diagnosis of retinal lipemia. Despite the sharp increase in plasma TG levels, the development of atherosclerosis does not accelerate.
The diagnosis of familial lipoprotein lipase deficiency should be assumed when milky yellow, creamy blood plasma is detected upon standing. The diagnosis is confirmed by the absence of an increase in plasma lipoprotein lipase activity after heparin administration and a sharp increase in the levels of cholesterol and triglycerides.
Symptoms become less pronounced if the patient is switched to a low-fat diet. Since medium-chain TGs are not included in HM, these are the fats that should be used in the diet to ensure its normal calorie content. The patient must also receive fat-soluble vitamins.
HLP type 2 (familial hypercholesterolemia) is the most common form. It is an autosomal dominant disorder caused by a mutation in the gene for apo B100, a protein that binds LDL to the LDL receptor.
Due to the reduced activity of LDL receptors, the catabolism of these drugs is blocked, and their amount in the plasma increases in proportion to the decrease in receptor function. The liver is unable to effectively capture LDLP, which should be converted into LDL. This leads to impaired uptake, impaired LDL excretion and accumulation of total cholesterol in the blood plasma. As a result, their concentration increases by 2–6 times.
This form of HLP is divided into subtypes 2a and 2b. The first is characterized, along with an increase in LDL and cholesterol, by normal levels of VLDL and TG. With subtype 2b, described in 1973, combined lipidemia is typical: increased LDL, VLDL, TG, cholesterol.
Heterozygous familial hypercholesterolemia type 2a should be assumed when an isolated increase in plasma cholesterol levels is detected in children against the background of unchanged triglyceride concentrations. An isolated increase in cholesterol levels is usually caused by an increase in the concentration of LDL cholesterol only. In familial hypercholesterolemia, only half of first-degree relatives have elevated plasma cholesterol levels. The presence of skin xanthomas helps in diagnosis. When collecting anamnesis from relatives, early manifestations of coronary heart disease can be identified.
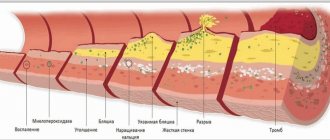
HLP type 2b is much more common in children. High levels of cholesterol, TG, LDL, and VLDL are detected. Excess LDL infiltrates the vascular wall, leads to unregulated accumulation of cholesterol in cells, their foamy transformation, and contributes to the development and early progression of atherosclerosis and coronary heart disease.
Relatives are often diagnosed with hyperinsulinism, insulin resistance, arterial hypertension, uricemia, and early development of atherosclerosis. With familial hypercholesterolemia, the incidence of obesity and diabetes mellitus does not increase. In patients, body weight, as a rule, is even less than normal.
This form of HLP occurs already in newborns. With homozygous carriage, such patients die in childhood from myocardial infarction. In cases where very high levels of cholesterol in the blood plasma are detected, parents should be examined to exclude familial hypercholesterolemia.
Since atherosclerosis in this disease is caused by a prolonged increase in plasma LDL levels, patients should be switched to a diet low in cholesterol and saturated fat and high in polyunsaturated fat. You should exclude butter, cheese, chocolate, fatty meats and add polyunsaturated oils (corn, olive, fish oil, etc.). In this case, the plasma cholesterol level in heterozygotes decreases by 10–15% [1].
Familial HLP type 3 is a rare form. In this congenital disease, plasma levels of both cholesterol and TG are elevated. This is due to the accumulation of residues in the plasma resulting from the partial destruction of VLDL. The mutation that determines the disease affects the gene encoding the structure of apoprotein E, a protein that is normally found in DILI and remnants of chylomicrons. It binds both the chylomicron remnant receptor and the DILI receptor with very high affinity. VLDL, LPPP, and TG increase in the blood plasma. The conversion of VLDL to LDL is disrupted, and the level of HDL decreases. These drugs accumulate in large quantities in plasma and tissues, causing xanthomatosis and atherosclerosis.
HLP manifests itself after 20 years. In the clinic, accelerated sclerosis of the vessels of the heart, carotid arteries, and vessels of the lower extremities is typical, and, consequently, early myocardial infarctions, strokes, intermittent claudication and gangrene of the legs.
The disease may be accompanied by obesity, type 2 diabetes mellitus, and hepatosis. Tuberous xanthomas, which are localized in the area of the elbow and knee joints, are considered pathognomonic. The plasma becomes cloudy when standing.
Primary type 4 HLP, or familial triglyceridemia, is characterized by high TG concentrations with normal or slightly elevated fasting cholesterol levels. It is a common (17–37%) autosomal dominant disorder. It appears in various periods of childhood, but more often in older years.
The pathogenesis of primary triglyceridemia is not entirely clear. It is believed that there is excess production of TG in the presence of normal levels of apo-B lipoproteins, causing the formation of TG-rich VLDL in the liver. There is not enough data on the atherogenicity of these lipoproteins [2].
Familial triglyceridemia can be suspected if the patient has high levels of TG, VLDL and a normal amount of cholesterol. The disease should be confirmed by studying the lipid profile of close relatives. When the blood taken is left standing for 8 hours, flakes can be detected in the plasma. In some patients, HDL is elevated, which may be due to the low atherogenicity of this form of HLP. Xanthomas are not typical for familial hypertriglyceridemia.
This variant of secondary HLP occurs in metabolic syndrome, type 2 diabetes mellitus and other endocrinopathies.
HLP type 5, or familial combined HLP, is inherited as an autosomal dominant trait. This form, combining an increase in TG and CM, has signs of types 1 and 4 of HLP. Close relatives may have only a mild form of the disease with moderate hypertriglyceridemia without hyperchylomicronemia, hypercholesterolemia, i.e., it may be characterized by hyperlipidemia of various types. When standing, the plasma forms a cloudy layer. The mutant gene is unknown.
Increases in plasma cholesterol and/or triglyceride levels are detected at puberty and persist throughout the patient's life. The increase in lipid and lipid levels is not constant: during different periods of the examination, high indicators may decrease, while others, on the contrary, may increase significantly.
Family history often suggests early coronary artery disease. Mixed type HLP is found in approximately 10% of all patients with myocardial infarction. The incidence of obesity, hyperuricemia and impaired glucose tolerance is increased [1].
Mild or moderate hypertriglyceridemia can sharply increase under the influence of various provoking factors (decompensated diabetes mellitus, hypothyroidism, taking medications containing estrogens). Plasma triglyceride levels may increase. During periods of exacerbations, patients develop mixed hyperlipidemia, i.e., the concentration of both VLDL and CM increases. After eliminating the provoking factors, chylomicron-like particles disappear from the plasma and the concentration of triglycerides returns to the original level.
Secondary SLP
There are basal and induced HLP. Basal HLP is detected in fasting blood tests and is more severe and indicates profound disturbances in fat metabolism. Induced (postprandial) HLP are detected after taking carbohydrates, fats, hormonal drugs, and severe physical activity. These include nutritional HF, which develop after excessive consumption of fats in food.
Secondary HLP are often manifested by increased levels of several classes of drugs in the blood plasma. The change in lipid spectrum may be similar to the primary types of HLP. Clinical changes are determined by the underlying disease. Often (primarily at the beginning of the development of the pathological process), quantitative and qualitative changes in the composition of drugs in the blood plasma are adaptive in nature [3].
Diabetes mellitus type 1
Insulin-dependent diabetes mellitus (DM) significantly affects lipid metabolism. Hypertriglyceridemia occurs in most patients. It is associated with the role of insulin in the formation and removal of lipid-rich drugs from plasma [1, 3].
With insulin deficiency, the synthesis of TG and the content of apo-B lipoproteins increase. Due to impaired LPL activity, the excretion of TG-rich particles is reduced. Insulin deficiency increases lipolysis in adipose tissue, resulting in a high flow of FFA to the liver. It enhances the synthesis and secretion of TG into the blood as part of VLDL as a secondary reaction to the increased mobilization of free fatty acids from adipose tissue.
The cholesterol content of LDL increases, but to a lesser extent. In decompensated diabetes, the plasma concentration of FFA is increased and correlates with the level of glucose in the blood.
As the duration of hypoinsulinemia increases, the rate of removal of VLDL and cholesterol from the blood decreases due to a decrease in lipoprotein lipase activity, since insulin is necessary for the synthesis of LPL in adipocytes. Diabetic lipimia develops. This is facilitated by glucagon, which increases sharply during decompensation, increasing the release of FFA into the blood.
Some of the FFA is metabolized to acetyl-CoA, which is then converted into acetoacetic and B-hydroxybutyric acids. These lipid metabolism disorders resemble the phenotype characteristic of primary type 4 or 5 HLP.
Severe lipidemia leads to fatty liver and pancreas, creamy appearance of retinal vessels, and abdominal pain.
According to V.M. Delyagin et al. In children with type 1 diabetes, dyslipidemic disorders were manifested by changes in the pattern of the liver parenchyma, thickening of the vascular walls, changes in the media/intima ratio, and a decrease in vascular elasticity [4].
The blood has a milky color and a creamy layer appears when standing. This is due to acquired LPL deficiency. But, given the prevalence of diabetes, a combination of primary hereditary disorders of lipid metabolism and HLP associated with absolute insulin deficiency is possible. Hormone replacement therapy quickly reduces the severity of lipoproteinemia.
So, hypertriglyceridemia, increased VLDL cholesterol levels, and non-enzymatic glycosylation of apoproteins are risk factors for the development of atherosclerosis in patients with type 1 diabetes and type 2 diabetes. Compensation of diabetes reduces the severity of HLP and, therefore, inhibits the development of atherosclerosis.
Obesity
Among all forms of obesity in childhood, a simple form occurs (85–90%). The constitutional factor is leading in the genesis of this form of the disease. Genetic predisposition to obesity may be associated with central dysregulation of energy balance, with an increase in the number of adipocytes and increased metabolic activity of the latter.
In adipose tissue, the synthesis and hydrolysis of lipids, the synthesis of fatty acids, including from carbohydrates, their esterification into neutral fats (TG), their deposition and breakdown with the formation of fatty acids, and their use for energy purposes constantly occur.
LPL activity in adipose tissue is regulated by insulin, i.e. insulin stimulates the uptake and accumulation of circulating FFAs in adipocytes.
Another mechanism for lipid deposition in adipose tissue involves the conversion of glucose and other carbohydrates into fats, which is controlled by insulin. Under physiological conditions, one third of dietary glucose is used for the synthesis of endogenous fat, in obese patients up to two thirds.
In the blood of obese patients, increased levels of cholesterol, TG, LDL and decreased HDL are detected. Such patients have reduced tolerance to exogenous lipids—in response to a fat load, they experience a pronounced prolonged hyperlipidemic reaction. CMs in these patients are broken down slowly, and lipolytic activity appears late [3].
Hyperinsulinemia is important in the pathogenesis of obesity. Increased insulin secretion causes increased appetite. The liver begins to synthesize more TG.
Metabolic syndrome
Obesity with excess visceral fat, accompanied by insulin resistance (IR) and hyperinsulinemia (HI), disorders of carbohydrate, lipid, purine metabolism, and arterial hypertension, is systematized under the term “metabolic syndrome (MS)” [5].
Abdominal obesity increases the release of FFAs from adipocytes into the blood plasma and their uptake by the liver. The synthesis of TG and apo-B lipoproteins increases in it, and small LDL particles dominate. The production of HDL decreases, the removal of excess cholesterol from the body is impaired, the level of glucose in the blood increases, and the tendency to blood clots and inflammation increases. Conditions are created for the formation of the atherosclerotic process. This is predisposed by glycation of apoproteins, which impairs their binding to lipids. Glycated VLDL cholesterol and LDL cholesterol circulate in the blood longer. The risk of developing cardiovascular diseases increases.
The pathogenetic cause of MS is still unknown, but a close relationship has been noted between increased body weight and IR and GI. Abdominal obesity contributes to increased IR, causing an increased influx of FFA from adipocytes to the liver. Adipocytes of visceral adipose tissue, having increased sensitivity to the lipolytic action of catecholamines and low sensitivity to the antilipidic action of insulin, secrete FFAs, which prevent the binding of insulin to the hepatocyte, which leads to HI [6].
Risk factors for metabolic syndrome in a child are the presence of abdominal obesity, type 2 diabetes, arterial hypertension, myocardial infarction, stroke and other vascular disorders in relatives [2].
To diagnose MS, it is necessary to evaluate anthropometric measurements, blood pressure, determination of glucose, insulin, fasting C-peptide levels, and lipid spectrum. A simple indicator is the IR ratio of fasting TG concentration to HDL cholesterol level. If this index is 3.5 or more, then this indicates IR.
Hypothyroidism
Dyslipidemia accompanying hypothyroidism is accompanied by an increase in atherogenic drugs and a decrease in the content of antiatherogenic drugs.
Thyroid hormones influence all stages of lipid metabolism. They promote the uptake and synthesis of lipids in the liver, the oxidation of TG from adipose tissue, the transport of FFAs, the absorption and excretion of cholesterol in the composition of bile acids, and an increase in the activity of hepatic lipase.
Apparently, thyroid hormones exert their effects by stimulating genes responsible for the synthesis and lipolysis of lipids and lipids. With a deficiency of thyroid hormones, the amount of apo-B and apo-E proteins and LDL receptors in the liver decreases, the excretion of cholesterol is impaired, and the level of VLDL and LDL in the blood increases. A decrease in hepatic lipase activity disrupts the conversion of VLDL into LDLP, and from the latter the formation of HDL. A decrease in the activity of cholesterol transport protein leads to disruption of the reverse transport of cholesterol to the liver.
A high level of LDL cholesterol with a reduced concentration of HDL is associated with a high risk of atherosclerosis [7].
If hypothyroidism is detected, levothyroxine is prescribed. This treatment is accompanied by normalization of the patient's lipid levels within a month.
In subclinical hypothyroidism, the presence of atherogenic dyslipidemia is also indicated, which requires corrective therapy. Opinions are divided on thyroid hormone replacement therapy for subclinical hypothyroidism [7, 8]. Some authors believe that the administration of L-thyroxine more often normalizes the lipid spectrum in such patients. Others believe that the administration of lipid-lowering drugs is sufficient to correct dyslipidemia.
Somatotropic insufficiency
Growth hormone (GH) plays an active role in the regulation of basal metabolism. It is an anabolic hormone and has lipolytic activity. In adipose tissue, GH increases the number of preadipocytes and suppresses the activity of LPL, an enzyme that hydrolyzes TG in lipoproteins to NEFA, which are re-esterified in the liver and deposited in adipocytes [9].
Most patients with somatotropic insufficiency (STI) exhibit excess adipose tissue, decreased muscle mass and strength, osteoporosis, and early atherosclerosis. GH deficiency in adults increases the risk of death from cardiovascular diseases (myocardial infarction, stroke, etc.). One of the factors that provoke changes in blood vessels during STN is a disorder of lipid metabolism. An increase in the level of total cholesterol, LDL, and apoprotein B is detected. Other studies have revealed an increase in TG levels and a decrease in HDL [10]. More significant changes in lipid metabolism were observed in patients with multiple pituitary hormone deficiency.
Long-term replacement therapy with recombinant growth hormone led to a decrease in the levels of total cholesterol and LDL, but did not affect the content of HDL and TG [11].
Cushing's syndrome
Glucocorticoids (GCs) play important roles in energy homeostasis and have complex but unclear effects on lipid metabolism. GCs modulate the expression of about 10% of human genes. They regulate the differentiation, function and distribution of adipose tissue.
Under the influence of GCs, FFAs in the blood increase, since these hormones accelerate lipolysis, disrupt the formation of glycerol, and reduce glucose utilization. The effect of GC on fat metabolism depends on the localization of subcutaneous fat. With an excess of HA, the fat layer on the extremities is reduced, and on the face and torso it is overdeveloped.
With an excess of glucocorticoids in the blood, total cholesterol and TG increase, while the level of HDL may vary. Insulin resistance plays a key role in this dyslipidemia. In vitro, cortisol increases lipoprotein lipase levels in adipose tissue, especially visceral fat, where lipolysis is activated and FFAs are released into the circulation.
Impaired glucose tolerance or steroid diabetes, IR, hypercoagulation determine an increased risk of cardiovascular pathology in this group of patients. However, the degree of dyslipidemia in the clinic is very variable in patients with exogenous and endogenous excess GC [1, 2].
A study of 15,004 patients found that GC use was not directly associated with an unfavorable lipid profile. In Cushing's syndrome, there is an increase in VLDL, but not HDL, with a subsequent increase in triglycerides and total cholesterol. The prevalence of hepatic steatosis among patients receiving GCs and patients with Cushing's syndrome is not the same. In the latter, it primarily depends on the volume of abdominal and visceral fat [12].
These changes are normalized or significantly improved after correction of hypercortisolism.
Kidney diseases
HLP in renal diseases is common. Changes in the spectrum of lipids occur already in the early stages of glomerulonephritis and are aggravated during chronic course. In the acute period of the disease, an increase in TG, represented by cholesterol and VLDL, is characteristic, i.e., dyslipidemia develops, similar to primary type 4 HLP. The cholesterol content in VLDL also increases with a relative decrease in TG. Opposite ratios are typical in LDL.
In chronic kidney disease, dyslipidemia is manifested by an increase in TG. This is due to an increase in the content and decrease in clearance of VLDL and accumulation of LDL [13]. The experiment showed that in case of renal failure, the formation of receptors for VLDL in adipose tissue is disrupted, which increases their concentration and, consequently, maintains hypertriglyceridemia. This is facilitated by a decrease in LPL activity in adipose tissue. Deficiency of hepatic lipase impairs the hydrolysis of TG in LDLP with the formation of LDL and HDL phospholipids.
With renal failure, the content of the most atherogenic LDPP increases, which accelerates the atherosclerotic process.
With nephritic syndrome, a mixed form of HF is often detected with an increase in both cholesterol and TG, which is similar to type 2 of HF. The concentration of LDL increases with normal or decreased amount of HDL. HLP is associated with hypoalbuminemia. Remission of the disease is accompanied by normalization of lipidemia.
Treatment
Etiological treatment for primary HLP has not yet been developed. Some forms of secondary HLP are well corrected by replacement therapy (type 1 diabetes, hypothyroidism, somatotropic insufficiency).
Pathogenetic treatment of HF is primarily aimed at reducing plasma cholesterol levels. A diet low in cholesterol and saturated fat and high in polyunsaturated fat. Exclude butter, cheese, chocolate, pork. The diet uses corn and sunflower oil.
When metabolic syndrome is detected, it is recommended to limit or eliminate easily digestible carbohydrates. The amount of fat is reduced by up to 70%, mainly due to animals, which are replaced by 50% with vegetable ones.
Physical activity along with diet for HLP is the most important factor in treatment. Physical activity increases metabolism and accelerates the mobilization of fat from the depot.
The use of lipid-lowering drugs in childhood is limited due to many side effects [14].
Literature
- Kronenberg G. M. et al. Obesity and lipid metabolism disorders / Trans. from English edited by I. I. Dedova, G. F. Melnichenko. M.: Read Elsiver LLC, 2010. 264 p.
- Endocrinology and metabolism. T. 2. Per. from English / Under. ed. F. Fehling, J. Baxter, A. E. Broadus, L. A. Fromen. M.: Med., 1985. 416 p.
- Turkina T.I., Shcherbakova V.Yu. Features of dyslipidemia in children // Rational pharmacotherapy in cardiology. 2011, no. 7 (1), 65–69.
- Delyagin V.M., Melnikova M.B., Serik G.I. Dyslipidemia syndrome in children with chronic diseases // Practical Medicine. 2014, No. 9 (85), p. 7–10.
- Bokova T. A. Metabolic syndrome in children. Tutorial. M., 2013. 21 p.
- Gurina A. E., Mikaelyan N. P., Kulaeva et al. The relationship between the activity of insulin receptors and blood ATP against the background of dyslipidemia in children with diabetes mellitus // Fundamental Research. 2013, no. 12–1, p. 30–34.
- Biondi B., Klein I. Cardiovascular abnormalities in subclinical and overt hypothyroidism/The Thyroid and cardiovascular risk. Stuttgart; New York, 2005. 30–35.
- Budievsky A.V., Kravchenko A.Ya., Feskova A.A., Drobysheva E.S. Dyslipidemia in subclinical hypofunction of the thyroid gland and the effectiveness of its correction with L-thyroxine replacement therapy // Young scientist. 2014, 17, p. 138–141.
- Dedov I. I., Tyulpakov A. N., Peterkova V. A. Somatotropic insufficiency. M.: Index Print, 1998. 312 p.
- Volevodz N. N. Systemic and metabolic effects of growth hormone in children with various types of short stature. Diss. Doctor of Medical Sciences 2005.
- Volevodz N. N., Shiryaeva T. Yu., Nagaeva E. V., Peterkova V. A. The state of the lipid profile in patients with somatotropic insufficiency and the effectiveness of correction of dyslipidemia during treatment with the domestic recombinant growth hormone “Rastan”. https://umedp.ru |articles|sostoyanie_lipidnogo_profilya.
- Arnaldi G., Scandali VM, Trementino L., Cardinaletti M., Appolloni G., Boscaro M. Pathophysiology of Dyslipidemia in Cushing's Syndrome // Neuroendocrinology. 2010; 92(suppl 1): 86–90.
- Rudenko T. E., Kutyrina I. M., Shvetsov M. Yu. State of lipid metabolism in chronic kidney disease. Clinical nephrology. 2012, no. 2, p. 14–21.
- Vasyukova O. V. Federal clinical guidelines for the diagnosis and treatment of obesity in children and adolescents. M.: Institute of Pediatric Endocrinology ENC, 2013. 18 p.
V. V. Smirnov1, Doctor of Medical Sciences, Professor A. A. Nakula
State Budgetary Educational Institution of Higher Professional Education Russian National Research Medical University named after N. I. Pirogov Ministry of Health of the Russian Federation, Moscow
1 Contact information
Symptoms and consequences
Not every disease actively manifests itself with symptoms. A person can live for a long time with low cholesterol levels in the blood and not even suspect it. Nevertheless, there are a number of signs that may indicate that, against the background of low cholesterol levels in the blood, a person develops pathologies and diseases:
- loss of appetite and its complete absence for no apparent reason;
- constant weakness;
- fatty stools;
- enlarged lymph nodes;
- mood swings;
- decreased sexual desire.
Low cholesterol levels can lead to serious diseases, including:
- deterioration of vascular elasticity and, as a result, hemorrhagic stroke;
- the development of obesity, since the metabolism of fat cells is disrupted and incoming fats cannot be absorbed normally;
- problems of the reproductive system, since cholesterol is involved in the synthesis of sex hormones;
- impaired body resistance to insulin and, as a result, diabetes mellitus;
- disorders of the nervous system, because with a lack of cholesterol, serotonin receptors cannot function normally. Because of this, anxiety, depression and even degradation develop.
Symptoms
It is impossible to determine hypocholesterolemia by external manifestations. To determine cholesterol levels, the patient must take a biochemical blood test performed on an empty stomach. In cases where you cannot visit the hospital for some reason, you should pay attention to your own well-being.
Symptoms such as lack of appetite for a long time, decreased sensitivity, systematic weakness, fatigue, and the presence of fatty loose stools can signal low cholesterol.
Enlarged lymph nodes, rapid mood swings, and decreased sexual activity appear. The listed symptoms may indicate hypocholesterolemia, so it is important to urgently consult a doctor and get tested!
What to do?
Since a person receives only 5-10% of the total cholesterol contained in the body from the outside, we can conclude that a low level indicates serious failures of internal metabolic processes in the body. There are situations when the patient takes certain drugs that reduce his levels. In other cases, the problem should be resolved immediately.
To improve your cholesterol levels, you first need to understand why your cholesterol levels have dropped. This can only be done by a competent specialist, so if the test shows low cholesterol in the blood, you should immediately go to the doctor.
It is impossible to give a general recommendation, since it is completely specific for each person. Low blood cholesterol levels indicate serious problems in the body.
Dr. Shishonin argues that if cholesterol levels drop, it is necessary to contact a competent specialist, otherwise there is a risk of seriously suffering from metabolic disorders.