Vascular malformations is a general term that includes congenital vascular anomalies: veins only - venous malformations (VM) lymphatic vessels only - lymphatic defects of both veins and lymphatic vessels: veno-lymphatic malformations anomalies of arteries connected directly to veins without a capillary network between them: arteriovenous malformations (AVMs)
general description
Arteriovenous malformation is a condition in which pathologically tortuous shunt vessels appear between arteries and veins instead of a network of capillaries. It can occur anywhere, but the most clinically significant is cerebral arteriovenous malformation. As a result of replacement of the capillary bed, the exchange of oxygen and nutrients between tissues and blood is disrupted, and the brain experiences oxygen starvation. In addition, vessels with arteriovenous malformation of the brain have a thinner wall than normal, so they can rupture. The risk of rupture reaches 4% per year. Mortality from AVM rupture in non-operated patients reaches 30%, disability – 50%.
Radiosurgery
During this procedure, precisely focused radiation is directed at the abnormal vessels. Accurate focusing requires several hours of preparation; The irradiation itself takes another hour. The patient is discharged on the same day. Over the next 6 to 24 months, the vessels gradually close and are replaced by connective tissue. The advantages of this method are that the skull is not opened and the procedure is painless. The disadvantages of the method are that the best results are obtained only with small AVMs, and the therapeutic effect is achieved after a long time. During this time, the risk of hemorrhage remains. In a recent long-term experiment conducted in one of the large clinics in America, 73% of patients showed excellent or good results after radiosurgery. In these patients, the risk of future bleeding was reduced to almost zero.
Symptoms
Arteriovenous malformation can be asymptomatic, in which case the patient will never know that he had this pathology. In half of the diagnosed cases, the disease manifested itself with bleeding. Rupture of a deformed vessel threatens hemorrhagic stroke, disability and death. In another quarter of cases, the malformation causes epileptic seizures. Large and distended vessels can cause persistent and intractable headaches, and if their size is so large that it leads to compression of brain tissue, focal neurological deficits can occur.
Tests and diagnostics
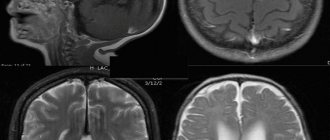
The diagnosis is established after a complete clinical examination and radiological examination methods (ultrasound or MRI).
When examining the patient, attention is drawn to increased sweating , pulsation , hyperpigmentation of the skin , and hypertrichosis over the area where the malformation is located. External localization is also characterized by varicose veins, vascular nevus, tissue hypertrophy (tumor-like vascular formation). It is very important to find out whether there have been previous injuries and bleeding in this area.
The following instrumental diagnostic methods are used:
- Doppler ultrasound;
- MRI (including with dynamic contrast enhancement);
- Angiography;
- Scintigraphy.
Treatment of brain AVM
Treatment consists of surgical removal of pathological vessels. Classical open excision of a malformation is used mainly only in emergency cases, when a vessel ruptures, when it is necessary not only to remove it, but also to aspirate the resulting hematoma.
In case of uncomplicated malformation, one can resort to angioembolization, when an embolic substance is injected into the pathological vessel, its lumen is permanently closed and the vessel functionally disappears.
The most modern method is radiosurgery, during which the malformation is irradiated, leading to complete closure of the lumen of the vessel.
How is the diagnosis made in Israel?
Seeing a doctor about an AVM is usually associated with either its rupture or the intention to begin treatment for an AVM that was previously discovered. In any case, the doctor reviews symptoms and other medical problems, family history, a list of medications taken on an ongoing basis, and also conducts a physical examination. Next, the patient will be referred for additional tests to determine the type and size of the AVM, its location and interaction with other structures.
- Computed tomography (CT) is a non-invasive technique that takes detailed X-ray images of the brain to detect the presence of blood inside or outside the brain tissue. A relatively new modification of CT is called CT angiography. In this case, contrast is injected into the general bloodstream to visualize the cerebral arteries. The combination of standard CT and angiography makes it possible to assess the condition of brain tissue and blood vessels.
- Magnetic resonance imaging (MRI) is a non-invasive test that uses a magnetic field and radio frequency waves. Its type, magnetic resonance angiography (MRA), allows you to obtain detailed images of the vascular bed in a non-invasive way.
- Angiography is also used as an invasive procedure, when a catheter is inserted into a peripheral artery and passed into the vessels of the brain. After this, contrast is injected into the blood and a series of x-rays are taken.
Arteriovenous malformations of the vein of Galen (AVMvG) are a special type of arteriovenous malformations (AVMs), characteristic mainly of pediatric patients. AVMvH account for approximately 30% of AVMs detected in childhood. The pathology is congenital and is characterized by the formation of an arteriovenous shunt in the area of one of the main venous collectors - the great cerebral vein (vein of Galen) [3-5, 7, 9, 11].
The main clinical manifestations of AVMvH are: 1) hypertensive-hydrocephalic syndrome, which develops as a result of occlusion of the cerebral aqueduct, impaired cerebrospinal fluid resorption; 2) focal neurological symptoms caused by secondary disorders of cerebral circulation of the ischemic type; 3) delayed psychomotor development of a child of a younger age group [5-7, 10, 12].
At the first stages of the development of vascular neurosurgery, treatment of AVMvH was palliative and limited to shunt operations for occlusive hydrocephalus, which did not solve the problem of the underlying disease. In cases of the natural course of the disease, i.e. without medical support, up to 90-96% of children died during the 1st year of life [14].
In connection with the modernization and fundamental changes in approaches to the treatment of AVMvH, the issue of early diagnosis of this pathology is of particular relevance. Currently, the standard for diagnosing AVMvH is ultrasound examination, which makes it possible to establish an accurate diagnosis already in the third trimester of pregnancy [1, 2, 15].
Attempts at open interventions for AVMvH, carried out before the era of endovascular surgery, were associated with high postoperative mortality, reaching 60%. Currently, this option of open interventions is performed only for thrombosed vein of Galen, which has a volumetric effect on the midbrain [8].
The question of the need, timing, and clear indications for performing CSF shunt operations as part of the complex treatment of this pathology remains debatable; This refers to the combination and sequence of endovascular and liquor shunt operations [16].
The small amount of data in the world and domestic literature and the inconsistency in approaches to complex treatment became the reason for conducting this study, the purpose of which is to develop an optimal algorithm for the diagnosis and treatment of patients with AVMvH.
Material and methods
The work is based on an analysis of the results of examination and treatment of 90 patients with AVMvH at the Research Institute of Neurosurgery named after. acad. N.N. Burdenko RAMS for the period from 1987 to 2009. Over the entire analyzed period, there was a gradual annual increase in the number of patients with AVMvH, mainly children of the younger age group, which is associated with improved early diagnosis and expanded opportunities for effective treatment of this pathology. The largest number of observations (38) occurred in the period from 2006 to 2009. Patients examined and operated on during this period constituted a prospective group.
The age of the patients ranged from 3 weeks to 38 years. All patients (27 (30%) female and 63 (70%) male) were divided into four age groups: group 1 (≤1 year) - 35 (39%), group 2 (1- 3 years old) - 15 (17%), 3rd group (3-10 years old) - 19 (21%), 4th group (over 10 years old) - 21 (23%), including 11 aged up to 16 years old, 10 - adults. The average age of patients under 16 years was 3.5 years, for adults - 22.9 years.
The examination of patients included the collection of anamnesis and general clinical data (term and method of diagnosis, the presence of hydrocephalus, delayed psychomotor and speech development, epileptic seizures, a history of hemorrhages, cerebral symptoms), indicators of physical development (weight, height, head circumference), ophthalmological, otoneurological , cardiac examination (echocardiography), CT and MRI of the brain at the pre- and postoperative stages. Angiographic examination (AG) was performed in all 90 patients; in most cases, 75 (83.3%) were performed directly during endovascular surgery. The division of AVMvH into angioarchitectonic types - mural and choroidal - was carried out according to total selective cerebral angiography in accordance with the classification of P. Lasjaunias et al. [10].
Anesthesia for all operations in patients of younger age groups (younger than 10 years) was carried out under endotracheal anesthesia and constant monitoring of ECG, blood pressure, partial pressure of CO2 and respiratory rate. In patients older than 10 years, intravenous sedation or neuroleptanalgesia was most often used.
Of the 90 patients, 78 (86.7%) used various treatment options for AVMvH. In 12 (13.3%) patients, the tactics of dynamic observation were chosen. In this group, 3 patients underwent only cerebrospinal fluid shunt surgery.
Endovascular treatment was performed in 75 (94.9%) patients out of 78 operated on. They performed a total of 131 endovascular operations. In the vast majority of cases - 129 (98.5%) - operations were performed using transarterial access; in a few cases - 3 (2.3%) transvenous access was used. The tactics of endovascular treatment depended on the type of AVM, the caliber of afferents and the age of the patient.
Microsurgical treatment of AVMvH was performed in 4 (5%) patients. The purpose of direct surgical interventions was the excision of the thrombosed ampulla of the vein of Galen after endovascular occlusion or after spontaneous thrombosis of the dilated vein of Galen, which had a local volumetric effect on the adjacent brain structures, in combination with occlusive hydrocephalus.
Radiosurgical treatment was performed in 8 (10.1%) patients.
CSF shunt operations were performed in 24 (26.7%) patients. In 20 patients, ventriculoperitoneostomy was performed, in 4 cases endoscopic perforation of the floor of the third ventricle was performed. In 3 cases, endoscopic ventriculostomy of the third ventricle and ventriculoperitoneostomy were performed sequentially.
The natural history group included 12 (13.3%) patients. In 9 cases there was a functioning AVMvH; in 3 (3.3%) patients, according to hypertension, spontaneous thrombosis of the AVMvH was detected.
The dynamics of the disease picture was assessed on the basis of clinical and radiological examination of patients in the immediate postoperative period, as well as 3 and 6 months after endovascular surgery, depending on the age, dynamics of psycho-speech and motor development of the child in a prospective group of patients. In the retrospective group, the analysis was carried out using records of control examinations of patients in the clinic of the Institute of Neurosurgery.
Clinical picture and angioarchitecture
The primary diagnosis of AVMvH was established on the basis of fetal ultrasound in utero in 22 (22.2%) patients, in newborns - according to neurosonography - in 16 (17.8%), CT - in 23 (25.5%), MRI - in 30 (33.3%), hypertension - in 1 (1.1%).
The leading clinical picture in children of all age groups with AVMvH was hydrocephalic syndrome; in the group of children aged 1 to 3 years, it was detected in 80% of cases. Hydrocephalus was the result of hyporesorption of cerebrospinal fluid due to impaired venous circulation, or was of an occlusive nature due to compression of the cerebral aqueduct by the dilated ampulla of the vein of Galen. An increase in head circumference occurred mainly in patients of the younger age group - up to 3 years (60%). Among patients over 10 years of age (47%) who were diagnosed with hydrocephalus, according to CT data, craniomegaly was found in 4% of patients. In group 1, hydrocephalus was detected in 59% of children under 6 months of age, and in 75% of children aged 6 months to 1 year (Table 1).
Other symptoms were less common: symptomatic epilepsy - in 19 (21.1%), dysfunction of cranial nerves (II, III, VI, VII) - in 19 (21.1%) and intracerebral hemorrhages - in 8.9% . Congenital heart defects were observed in 34.4% of patients, of which 3 underwent surgical treatment for this pathology.
According to angiography, AVMvH of the choroidal type was detected in 67 (74.4%) patients, the mural type of AVM was verified in 20 (22.2%) patients (Fig. 1, a, b).
Figure 1. Angiogram of patients with AVMvH. a — choroidal type; b - mural type.
In 3 (3.3%) patients, spontaneous thrombosis occurred at the time of AG.
The afferents of AVMvH were most often the arteries of the vertebrobasilar system, less often - the arteries of the carotid system. In most cases, adjacent blood supply was detected (Table 2).
Results and its discussion
Results of endovascular treatment
The main goal of endovascular intervention was to stop or reduce the discharge of arterial blood into the cerebral venous system, which was achieved mainly through occlusion of afferent vessels using transarterial access. Only 3 patients had occlusion of the great cerebral vein due to the complete failure of transarterial embolization for the choroidal type of AVM. To occlude the afferents of AVMs of the mural type, microcoils and balloon catheters were used; for the choroidal type, microcoils, adhesive compositions, or a combination thereof were used.
Microspirals were used as occluding materials in 45 (60%) cases, detachable balloon catheters were used in 21 (28%) patients, adhesive compositions were used in 19 (24.9%) cases, including ONYX composition in 2 cases ( MTI, EV3, USA). In some observations - 10 (13.3%) a combination of different occlusive materials was used.
According to control cerebral hypertension, complete cessation of arterial inflow was achieved in the mural type of AVMvH in 61% of cases, while in choroidal type malformations this figure did not exceed 7%.
Complications after endovascular operations were noted in 10 (16%) cases. Of these, clinically significant complications - persistent neurological deficit caused by ischemic cerebral circulatory disorders in the choroidal arteries - occurred in 6 (10.7%). In 3 patients, intraventricular hemorrhage developed, in 1, a retroperitoneal hematoma was detected after endovascular surgery.
Death in the early period after endovascular surgery occurred in 2 (2.7%) cases. In one case, the cause of death was massive intraventricular hemorrhage, in the second - acutely developed occlusion at the level of the Sylvian aqueduct. Despite urgent external drainage of the lateral ventricles, the child died from axial herniation of the brain stem.
When assessing the dynamics of clinical symptoms 3 and 6 months after endovascular treatment, approximately the same results were obtained in all age groups; in the vast majority of observations, a positive result was noted (Fig. 2).
Figure 2. Dynamics of the clinical picture in different age groups 1 year after endovascular treatment.
In the long-term period (follow-up from 1 to 15 years) after endovascular treatment, improvement occurred in all age groups, the best result (82.8%) was observed in the group of patients under 1 year (Fig. 3).
Figure 3. Disease outcome in different age groups after endovascular treatment.
The “recovery” group included patients who had no clinical symptoms of the disease, and neuroimaging data did not reveal signs of functioning AVMvH and hydrocephalus (Fig. 4).
Figure 4. AVMvH of mural type. Endovascular occlusion of afferents by microspirals. Patient M. 4 months of age. a — MRI before surgery; b — initial hypertension of the vertebral artery; c — MRI 1 year after surgery; d — control hypertension of the vertebral artery. A comparative analysis of the outcome of the disease in different age groups found that improvement occurred in all age groups. The rate of recovered patients is significantly higher in groups 1-2 compared to groups 2-3. These trends reflect the degree of influence of endovascular operations on the clinical course of the disease. Thus, even a partial decrease in the degree of arteriovenous discharge creates conditions for improving cerebral hemodynamics, as a result of which the clinical status of patients improves (Fig. 5).
Figure 5. Choroidal type AVMvH. Occlusion of AVMvH afferents with microspirals (2 stages). Patient G. 3 months of life. a — MRI before surgery; b — initial hypertension of the vertebral artery; c — MRI 2 years after the 2nd stage of the operation; d — control hypertension of the vertebral artery. Total switching off of the pathological arteriovenous shunt (more often with mural-type AVMvH or with continued thrombosis after embolization of choroidal-type malformations) creates conditions for complete normalization of cerebral blood flow and leads to recovery of patients. Moreover, the earlier the endovascular operation is performed, the more obvious the overall positive effect. In addition, it is technically easier to perform endovascular interventions at an earlier age, when there is still no pronounced hypertrophy of afferent vessels and the volume of arteriovenous shunting is relatively low.
The probability of an increase in neurological symptoms is greatest in group 2 - 23.1%, and in the group of patients under 1 year of age the negative result was minimal - 3.2%.
The overall mortality rate among all 90 patients with AVMvH was 6.7%. In the early period after endovascular surgery, 2 (2.7%) patients died. In the long-term period, after partial occlusion of the afferents of the malformation, 2 (2.7%) patients died. Among patients who did not receive any treatment for AVMvH, 2 (16.7%) patients died from intraventricular hemorrhage.
Results of microsurgical and radiosurgical treatment
Microsurgical total excision of the thrombosed vein of Galen was performed in 4 patients. 3 of them experienced disability with the development of severe pyramidal symptoms.
Radiosurgical treatment was performed in 8 patients over 5 years of age with choroidal AVMvH. In 7 (87.5%) cases, radiation therapy was preceded by endovascular partial occlusion of accessible AVM afferents. When analyzing the long-term results of radiosurgical treatment, stabilization in the clinical and radiological picture of the disease was revealed in the majority of patients. In 2 patients, an increase in symptoms in the neurological status was noted. In 7 cases, according to control CT and MRI data, performed at different times after irradiation, the x-ray picture remained unchanged. Only in 1 observation during control hypertension was complete thrombosis of the AVM detected. However, this patient, a year after proton irradiation, developed symptoms of damage to subcortical structures, hemiparesis, paresis of the third nerve on the left, and emotional and personal disorders caused by the development of radiation necrosis.
Results in the natural history group
The natural course of the disease group included patients with spontaneous thrombosis of AVMvH, patients who at the time of treatment did not have the technical capabilities to perform endovascular surgery, as well as patients who refused surgical intervention, a total of 12 (13.3%) observations. When assessing the neurological status after 1 year of observation, stabilization of the clinical symptoms of the disease was noted in 8 (66.7%) cases. In 4 (33.3%) there was an improvement in neurological status. It should be noted that in 3 of these 4 patients spontaneous thrombosis of AVMvH was detected according to hypertension.
When analyzing the frequency of cases of stabilization and improvement in the groups of endovascular treatment and the natural course after 1 year, a statistically significant (p < 0.05) increase in positive results was shown in the group of patients who underwent endovascular treatment.
Evaluation of long-term results in the group with the natural course of the disease revealed a high mortality rate - 16.7% (2 observations) - in comparison with the endovascular treatment group (5.3%). Recovery occurred only in 3 patients with spontaneously thrombosed malformation; in the remaining 5 (41.7%) cases, the clinical status remained relatively stable.
Results of treatment of AVMvH against the background of liquor shunt operations
CSF shunt operations were performed in 24 patients. In 9 cases, shunt surgery was performed before endovascular treatment, in 13 patients - after partial occlusion of AVMvH, in 2 cases - with spontaneously thrombosed malformation. In no case was there any intracranial hemorrhage during CSF shunt surgery.
Complications after bypass operations developed in 9 (37.5%) patients. They were not specific in nature and were associated with inflammatory changes, as well as hyperdrainage syndrome and the development of subdural accumulations of cerebrospinal fluid.
Thus, AVMvH has a complex angioarchitecture, which is largely individual for each patient. There is no doubt that it is on the basis of a thorough study of angioarchitecture that adequate planning of all stages of surgical treatment of patients with AVMvH is possible.
Summarizing the results of our work, it should be noted that the most effective method of treating AVMvH is the endovascular method. The high percentage of satisfactory results obtained indicates the correct selection of optimal types of treatment depending on the anatomical type of AVMvH and the age of the patient.
A wait-and-see approach for asymptomatic AVMvH is unjustified, since successful endovascular treatment in the first year of life, before the onset of irreversible neurological disorders, allows one to achieve good clinical results. The natural history of AVMvH is associated with a higher risk of intracranial hemorrhage.
With mural-type AVMvH, endovascular treatment can achieve complete recovery of the patient, while with choroidal-type AVMvH, by occlusion of the largest afferents, stabilization of the clinical manifestations of the disease can be achieved by improving cerebral circulation.
Radiation therapy for AVMvH with large afferents and high shunting rates is ineffective. Indications for radiosurgical treatment can be determined in patients with AVMvH of the choroidal type with numerous small-caliber afferents and a relatively low volume of arteriovenous discharge, as well as after partial embolization upon achieving maximum blood flow reduction.
The assumption existing in some literature sources [1, 13] that CSF shunt operations against the background of a functioning AVMvH are associated with a high risk of hemorrhagic complications was not confirmed in our observations. For progressive occlusive hydrocephalus, the method of choice is endoscopic ventriculostomy, for aresorptive hydrocephalus - ventriculoperitoneal shunting.
conclusions
1. Prenatal diagnosis of AVMvH using ultrasonography and fetal MRI makes it possible to establish a diagnosis already in the third trimester of pregnancy, which allows adequate planning of delivery and further treatment of the child.
2. The endovascular method is a highly effective and low-traumatic method of treating AVMvH with a low level of disability and mortality. Microsurgical excision of AVMvH is associated with a high risk of complications and disability for the patient.
3. The optimal age for treatment is 4-5 months. Heart failure is not an absolute contraindication for endovascular surgery, except for decompensated heart failure requiring surgical treatment.
4. The presence of progressive hydrocephalus with corresponding symptoms is an indication for CSF shunt surgery before endovascular treatment.
Review
Treatment of patients with arteriovenous malformations of the vein of Galen (AVMvG) continues to be one of the important problems of modern neurosurgery. Due to its relatively rare occurrence, there is no uniform standard for the treatment of this pathology.
The article provides convincing data in favor of the endovascular method of treating this pathology, based on retrospective and prospective analysis of a large number of patients, even according to global data. At the same time, the authors prove the low effectiveness of radiation therapy and justify performing CSF shunt operations for progressive occlusive and aresorptive hydrocephalus.
The work shows that endovascular treatment of AVMvH in the first year of life makes it possible to achieve complete recovery in a large number of patients, so wait-and-see tactics for this pathology are unjustified.
Undoubtedly, the presented article contains novelty and certain value in solving the problem of treating AVMvH and will be useful for both scientific and practical neurosurgeons.
V.E. Ryabukhin
(Moscow)
Causes of venous malformation
The human circulatory system is formed during the embryonic period of his life. There are many reasons why the circulatory system develops pathologies. These include:
- Infections in the mother's body;
- Abdominal injuries received during pregnancy;
- Taking medications not prescribed by a doctor;
- Undergoing medical treatment without a doctor’s recommendation;
- Alcohol addiction of the mother.
The most dangerous period is from the 5th to the 20th week of pregnancy, when the formation of the bloodstream in the embryo occurs. When a child is born, some types of angiodysplasia may appear, while other types will appear within 3 months after birth.