On average, 7-10% of Russians have chronic heart failure (CHF), 4.5% suffer from clinical symptoms of heart failure that reduce quality of life and ability to work, and among people over 65 years of age, half of patients with cardiovascular diseases have symptoms of CHF, and These numbers are increasing every year.
Heart failure is a syndrome caused by abnormal structure and decreased function of the heart. It can be the outcome of diseases such as arterial hypertension, coronary heart disease, heart defects, arrhythmias, kidney and thyroid diseases, cardiomyopathies, hereditary or as a result of infections, intoxications, metabolic and other disorders.
Classification
There is a classification of CHF according to the stages of development of the disease (N.D. Strazhesko, V.Kh. Vasilenko):
Stage I (initial) - signs of deficiency appear only during physical activity, there are no symptoms at rest.
Stage II is divided into two periods:
- period A – clinically pronounced disorder of the right or left side of the heart, congestion in the pulmonary or systemic circulation, shortness of breath and symptoms occur with little physical effort;
- period B – stagnation in both circles of blood circulation (manifested by shortness of breath, swelling), performance is sharply reduced.
Stage III (final) - changes in the structure of organs and tissues, due to impaired blood supply and trophism, shortness of breath at rest.
The severity of the disease is determined by the functional class (FC), which shows how limited the patient’s physical activity is.
- I FC - no restrictions on physical activity. Normal physical activity does not cause excessive shortness of breath, fatigue, or palpitations;
- FC II - minor limitation in physical activity. Feel comfortable at rest, but normal physical activity causes shortness of breath, fatigue, or palpitations;
- III FC is a clear limitation of physical activity. Feeling comfortable at rest but doing less physical activity than usual causes excessive shortness of breath, fatigue, or palpitations;
- IV FC - inability to perform any physical activity without discomfort. Symptoms may be present at rest. With any physical activity, discomfort increases.
The disease should not be allowed to develop; timely diagnosis will help prevent the occurrence of pathology. Our cardiology center of the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency invites you to undergo a comprehensive heart examination. Timely identification of the cause of heart failure and its treatment will help maintain your quality of life.
Types and symptoms
There are two types of CHF: systolic and diastolic with preserved blood ejection function. Even 20 years ago, the second type was difficult to diagnose, since the heart muscle did not weaken, and symptoms of CHF still occurred. Thanks to the advent of cardiac ultrasound and echocardiography, the diagnostic problem was solved.
A characteristic feature of the second type of CHF is increased pressure in the left ventricle. Because of it, the muscle thickens and becomes rigid - unable to relax. When circulation occurs, the heart must not only eject blood and contract, but also come to a state of rest so that the next portion can enter it. If this does not happen, blood stagnation occurs. And it turns out that the heart seems to pump blood well, but cannot relax.
There are four stages of chronic heart failure:
- The appearance of mild ailments during physical activity, but there are no structural changes in the heart yet.
- The occurrence of structural changes in the heart.
- Manifestation of the first symptoms.
- The manifestation of pronounced symptoms that are difficult to treat.
The first stage of the disease can appear decades before symptoms and therefore often goes undetected. Basically, it makes itself felt in the form of rapid fatigue and rapid heartbeat during vigorous activity. It does not appear in a calm state.
At the second stage of the disease, structural changes in the heart appear - the first signs of hemodynamic disturbances and blood stagnation, which lead to an enlargement of the chambers of the heart. Symptoms appear the same as in the first stage.
The first symptoms of the disease - shortness of breath and constant heart rhythm disturbances - appear only in the third stage. They are felt during physical activity and are long-lasting.
In older people, shortness of breath can also occur at rest due to stagnation of blood in the venous bed of the pulmonary circulation. Subsequently, shortness of breath begins to be accompanied by a cough, which appears at night or during physical activity. It appears due to stagnation of blood in the vessels of the lungs and gives rise to further swelling of the bronchial mucosa - at this moment the period of the last stages of CHF begins.
With severe circulatory failure, the patient has:
- constant shortness of breath;
- wheezing in the lungs;
- chronic fatigue;
- severe swelling of the limbs;
- enlarged heart;
- accumulation of fluid in the abdominal cavity.
Such symptoms indicate a severe case and, in some cases, require surgical intervention.
Causes of heart failure
The causes of heart failure may lie in concomitant diseases:
- arterial hypertension;
- cardiac ischemia;
- myocardial infarction;
- cardiomyopathy;
- heart defects;
- diabetes.
Experts identify a number of factors that can affect the development of the disease:
- arrhythmia;
- hypertensive crises;
- pneumonia;
- psycho-emotional or physical stress;
- ARVI;
- long-term use of certain medications;
- significant weight gain;
- alcoholism.
Eliminating risk factors will help avoid and prevent the onset of heart failure.
2.What causes the disease?
Heart failure can be caused by many factors and pathological processes occurring in the heart, including:
- Cardiac ischemia
. Coronary heart disease (CHD) is a disease of the arteries that supply blood and oxygen to the heart, in which blood flow to the heart muscle is reduced. As a result, the heart lacks oxygen and nutrients. - Heart attack
. A heart attack can occur when a coronary artery suddenly blocks and stops the flow of blood to the heart muscle. All or part of the heart muscle is no longer supplied with oxygen and may become damaged. A heart attack can cause an area in the heart that then does not function properly. - Cardiomyopathy
, or damage to the heart muscle. The causes of cardiomyopathy can range from problems with the arteries or circulation, infections, or alcohol or drug abuse. - Common factors leading to fatigue
. This may include high blood pressure, heart valve disease, thyroid disease, kidney disease, diabetes, or congenital heart defects. All this can lead to heart failure. In addition, heart failure can result from a combination of several of these conditions.
Visit our Cardiology page
Symptoms of heart failure
The symptoms are associated with the inability of the heart to provide adequate blood circulation and the development against this background of congestion in the pulmonary and systemic circulation (in the vessels of the lungs and the vessels of other organs and systems). Stagnation of blood in the lungs interferes with its normal saturation with oxygen and is manifested by shortness of breath. Edema - stagnation in the systemic circulation disrupts the functioning of almost all organs. Patients feel:
- increased fatigue;
- shortness of breath;
- swelling of the legs and feet;
- pain or discomfort in the abdominal cavity due to liver enlargement.
Symptoms of heart failure develop gradually and can sometimes go unnoticed for a long time, so it is necessary to undergo regular medical examinations. At the cardiology center of the Federal Medical and Clinical Center of the Federal Medical and Biological Agency, you can undergo a comprehensive heart examination in order to promptly recognize this syndrome and the diseases that accompany it.
1.What is heart failure?
Heart is a serious and, unfortunately, very common disease. This disease is one of the main reasons for hospitalization in people over 65 years of age.
Heart failure does not mean the heart stops working. Rather, it means that the heart becomes weaker than usual and pumps blood less well. In heart failure, blood moves through the heart and body at a slower rate. As a result, the heart cannot pump enough oxygen and nutrients
to meet the body's needs.
The heart responds to this by stretching the chambers
so more blood can pass through them, and this helps for a while.
But over time, the walls of the heart muscle weaken, unable to work at such a strenuous rhythm. This affects the kidneys, which cause the body to accumulate more fluid and salt. Fluid can accumulate in the arms, legs (ankles and feet), lungs and other organs, leading to edema. This condition is also called congestive heart failure .
A must read! Help with treatment and hospitalization!
Diagnostics
When collecting anamnesis, the doctor pays special attention to the presence of complaints of shortness of breath and fatigue. Collects information about the existence of other diseases. If heart failure is suspected, the patient is referred for instrumental studies and laboratory tests.
The Cardiology Center of the Federal Medical and Clinical Center of the Federal Medical and Biological Agency carries out a full range of diagnostic measures:
- ECG in 12 leads;
- ECHO-KG;
- Holter monitoring;
- ECG with dosed physical activity;
- transesophageal ECHO-CG;
- ABPM (24-hour blood pressure monitoring);
- Ultrasound of the abdominal organs;
- general blood analysis;
- biochemical blood test (lipid spectrum, blood glucose, liver and kidney function indicators);
- thyroid hormones;
- coagulogram (a test to determine blood clotting);
- general urine analysis;
- spirometry (respiratory function test);
Treatment of heart failure
When treating heart failure, the main focus is on eliminating the cause of the disease. Depending on the nature of the disease, its course and the general condition of the patient, the doctor chooses a treatment method.
On the basis of our cardiology center, the Federal Scientific and Clinical Center of the Federal Medical and Biological Agency, there are therapeutic and surgical departments. You may be required to undergo examination and selection of drug therapy in our hospital. If drug treatment is not effective enough, the cardiologist may recommend surgery. Specialists of the Cardiac Surgery Department of the Federal Scientific Center for Medical and Biological Agency successfully use advanced methods of treating heart failure. This could be an operation to correct valve disease, coronary heart disease, or arrhythmias. Our clinic performs unique minimally invasive surgeries.
Chronic heart failure (CHF) is a disease in which the heart is unable to pump enough blood to supply the body with oxygen. It can occur as a result of many diseases of the cardiovascular system, among which the most common are coronary heart disease, hypertension, rheumatoid heart defects, and endocarditis. A weakened heart muscle is unable to pump blood, releasing less and less of it into the vessels.
Heart failure develops slowly and in the initial stages appears only during physical activity. Characteristic symptoms at rest indicate a severe stage of the disease. As CHF progresses, it significantly worsens the patient’s condition, leading to decreased performance and disability. The result can be chronic liver and kidney failure, blood clots, and strokes.
Timely diagnosis and treatment can slow down the development of the disease and prevent dangerous complications. An important role in stabilizing the condition is given to a correct lifestyle: weight loss, low-salt diet, limiting physical and emotional stress.
Synonyms Russian
Congestive heart failure, heart failure.
English synonyms
Heart failure, congestive heart failure.
Symptoms
Clinical manifestations of heart failure depend on its duration and severity and are quite varied. The development of the disease is slow and takes several years. If left untreated, the patient's condition may worsen.
The main symptoms of chronic heart failure include:
- shortness of breath during physical exertion, when moving to a horizontal position, and then at rest;
- dizziness, fatigue and weakness;
- lack of appetite and nausea;
- swelling of the legs;
- accumulation of fluid in the abdominal cavity (ascites);
- weight gain due to edema;
- fast or irregular heartbeat;
- dry cough with pinkish sputum;
- decreased attention and intelligence.
General information about the disease
By contracting, the heart ensures continuous circulation of blood through the vessels. Together with the blood, oxygen and nutrients are supplied to all organs and tissues, and the end products of metabolism, including fluid, are removed. This is achieved by alternating two phases: contraction of the heart muscle (called systole) and its relaxation (diastole). Depending on which phase of cardiac activity disrupts its functioning, we speak of systolic or diastolic heart failure.
- Systolic heart failure is a consequence of weakness of the heart muscle and is characterized by insufficient ejection of blood from the chambers of the heart. Its most common causes are coronary heart disease and dilated myocardiopathy. More often observed in men.
- Diastolic heart failure occurs when the heart muscle loses its ability to stretch. As a result, much less blood enters the atria. The most common causes: arterial hypertension, hypertrophic myocardiopathy and stenotic pericarditis.
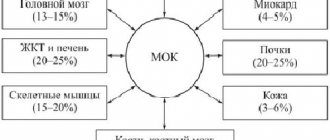
The human heart can be roughly divided into right and left halves. Pumping blood into the lungs and saturating it with oxygen is ensured by the work of the right parts of the heart, and the left ones are responsible for delivering blood to the tissues. Depending on which departments fail to cope with their task, they speak of right ventricular or left ventricular heart failure. When the functioning of the left sections is impaired, shortness of breath and cough come to the fore. Right-sided failure manifests itself as systemic edema.
To select the necessary medications, it is very important to determine the mechanism of heart failure and its type.
Who is at risk?
The presence of at least one of the following risk factors is sufficient for the development of chronic heart failure. The combination of two or more factors significantly increases the likelihood of disease.
Patients at risk include:
- high blood pressure;
- coronary heart disease;
- myocardial infarction in the past;
- heart rhythm disturbances;
- diabetes mellitus;
- congenital heart defect;
- frequent viral diseases throughout life;
- chronic renal failure;
- alcohol addiction.
Diagnostics
The diagnosis of chronic heart failure is made based on the medical history, characteristic symptoms and results of laboratory and other tests.
Laboratory research
- There are most often no changes in the general blood test. In some cases, moderate anemia may be detected.
- The erythrocyte sedimentation rate (ESR) may be elevated, especially when heart failure is the result of rheumatic heart disease or infective endocarditis.
- A general urinalysis is important to diagnose renal complications and exclude the renal origin of edema. One of the possible manifestations of chronic heart failure is high levels of protein in the urine.
- Total protein and protein fractions in the blood may be reduced due to their redistribution into the edematous fluid.
- Blood glucose. Important for excluding diabetes mellitus as a risk factor for heart failure.
- Cholesterol, high and low density lipoproteins. There is a clear relationship between elevated cholesterol levels and the development of atherosclerosis, coronary heart disease, and hypertension. High levels of cholesterol and lipoproteins in heart failure may indicate a more severe course of the disease.
- Sodium and potassium in the blood. In chronic heart failure, their level in the blood serum can change significantly due to edema. Monitoring blood composition is especially important when prescribing diuretics.
- Brain natriuretic propeptide (NT-proBNP) is a protein produced in the heart muscle in response to excessive stretching and overload. It circulates in the blood for quite a long time and can be easily determined during laboratory testing. The stronger the cardiac overload, the more active its secretion, therefore, an increase in the level of brain natriuretic propeptide in the blood reflects the severity of heart failure and helps to predict the disease. In addition, the higher the NT-proBNP level, the more severe the cardiac dysfunction. That is why this analysis is considered the “gold standard” in the diagnosis of chronic heart failure.
Additional Research
The scope of additional examination is determined by the attending physician.
- Chest X-ray. X-ray images allow you to assess the position and size of the heart, exclude or confirm concomitant changes in the lungs.
- Electrocardiography (ECG). Shows heart rhythm disturbances, as well as the consequences of a myocardial infarction.
- An echocardiogram allows you to differentiate systolic and diastolic heart failure, see the work of all parts of the heart, evaluate its size, muscle thickness, and examine the valves. The most important parameter is the ejection fraction. It reflects the efficiency of the heart and is expressed as the percentage of blood volume entering the aorta during contraction and remaining in it. Normally, this figure corresponds to 60-70%; in case of heart failure, it can decrease to 40%. The lower the ejection fraction, the more severe the degree of cardiac dysfunction. An indicator below 35% indicates a high risk of rhythm disturbances.
- Load tests. Designed to study the heart's response to increased physical activity.
- Coronary angiography. An X-ray examination in which a special contrast agent is injected through a catheter directly into the vessels of the heart. Helps establish the diagnosis of coronary artery disease.
Treatment
Heart failure is a chronic disease in which patients require constant medication. Properly selected therapy can slow down the progression of the process, and most often improve the condition. In some cases, surgical treatment is required.
An effective treatment method is the placement of pacemakers, or artificial heart rate regulators.
In the treatment of chronic heart failure, lifestyle also matters:
- complete cessation of alcohol and smoking,
- weight control,
- following a salt-free diet rich in protein and vitamins
- walks in the open air.
Prevention
- Lifestyle that prevents coronary heart disease:
- blood pressure control,
- regular physical activity,
- hardening procedures,
- normalization of metabolism (loss of excess weight, control of cholesterol levels, limited salt intake),
- quitting smoking, alcohol, coffee.
Clear and consistent implementation of the cardiologist’s recommendations can significantly slow down the pathological process and improve the patient’s quality of life.
Recommended tests
- Erythrocyte sedimentation rate (ESR)
- General blood analysis
- General urine analysis with microscopy
- Total protein in urine
- Serum albumin
- Total protein in whey
- Protein fractions in whey
- Total bilirubin
- Serum creatinine
- Urea in serum
- Rheumatoid factor
- C-reactive protein, quantitative (highly sensitive method)
- Potassium, sodium, chlorine in serum
- Serum calcium
- Serum magnesium
- NT-proBNP (quantitative)