Quick transition Treatment of gastritis
Gastritis is a general term that combines several pathological conditions characterized by inflammation and degeneration of the gastric mucosa.
The mucous membrane covers the entire surface of the stomach and plays an important role in digestion. Its glands produce gastric juice, the enzyme pepsin, hydrochloric acid, lipase, hormone-like components, mucus and bicarbonate. These substances are responsible for the breakdown of proteins and fats, protect the body from pathogenic bacteria, and activate metabolic processes.
When inflamed, the mucous membrane produces less acid, enzymes, mucus and other substances that are necessary for the proper functioning of the gastrointestinal tract. There is a risk of developing gastritis.
Gastritis can occur in acute and chronic forms. It is important to see a doctor in time to get a diagnosis and treatment, and to prevent complications.
Forms and complications of gastritis
In the absence of adequate and timely treatment, gastritis can cause complications. These include:
- Stomach ulcer. Peptic ulcers affecting the mucous membrane of the stomach or duodenum. Peptic ulcer disease is provoked by excessive use of painkillers (NSAIDs), and gastritis caused by H. pylori. It is difficult to say where gastritis ends, especially with erosions, and peptic ulcer disease begins. Apparently these are different forms of the same process.
- Atrophy of the gastric mucosa - atrophic gastritis. It occurs due to thinning of the mucous membrane, the formation of fibrosis (microscars) of the membrane during chronic gastritis. With atrophy, the number of active cells in the gastric mucosa that produce enzymes and acid decreases. The absorption of some vitamins is impaired. Atrophic gastritis is a risk factor for oncological transformation and therefore requires special attention.
- Gastric bleeding with erosive gastritis and ulcers. It is characterized by shortness of breath, weakness, dizziness, blood in the vomit and stool, black stools, and pale skin. If these symptoms occur, you should immediately seek medical help.
- Anemia. Most often it occurs due to acute (as described above) or chronic blood loss, for example, with multiple repeated erosions of the stomach. Research suggests that H. pylori-associated gastritis and autoimmune gastritis can affect the body's absorption of iron and vitamin B12 from food, which can also cause anemia.
- Vitamin B12 deficiency and pernicious anemia (pernicious anemia). Autoimmune gastritis does not produce a certain protein that helps absorb vitamin B12, which is necessary for the production of red blood cells and nerve cells. Insufficient absorption of vitamin B12 can lead to the development of pernicious anemia. The same changes occur in the advanced stage of atrophic gastritis of any origin.
- Stomach cancer. Chronic gastritis increases the likelihood of developing benign or malignant neoplasms in the gastric mucosa. For example, gastritis associated with H. pylory increases the risk of adenocarcinoma and lymphoma of the gastric mucosa.
Why are gastroprotectors needed?
To prevent complications such as peptic ulcers and malignant tumors, it is important to keep the structure of the mucous membrane intact. Gastroprotectors are used for these purposes:
They should be taken when signs of gastritis appear. The doctor will determine which medications will fit into the selected treatment package. For prevention purposes, you do not need to drink them.
The stomach contains natural gastroprotectors - prostaglandins. They stimulate the formation of mucus, improve microcirculation and protect cells from destruction. If they are not produced enough, the gastroenterologist may prescribe their synthetic analogues. If the patient is being treated with non-steroidal anti-inflammatory drugs, drugs with prostaglandins prevent ulcerative lesions of the mucous membrane.
Causes and risk factors of gastritis
- Bacterial infection Helicobacter pylori. It is one of the most common types of infections and is transmitted through the fecal-oral route, for example through contaminated food and water. For the development of gastritis, the presence of Helicobacter pylori infection alone is not enough. It is believed that vulnerability to the bacterium is inherited or occurs due to an unhealthy lifestyle (smoking, poor diet), medications.
- Painkillers (non-steroidal anti-inflammatory drugs, NSAIDs). Regular and excessive use of aspirin, ibuprofen or naproxen can cause both acute and chronic gastritis, their toxic effects reduce the production of the main protectors of the gastric mucosa. To distinguish this situation from other types of gastritis, it is called NSAID gastropathy.
- Alcohol. Irritates and gradually destroys the gastric mucosa, exposing it to the aggressive effects of gastric juice. Alcohol most often provokes acute gastritis.
- Age. Older people are at increased risk of developing gastritis because the lining of the stomach thins with age. Older people are also most vulnerable to infections (H. pylori) or autoimmune disorders.
- Stress. Severe stress associated with injuries, burns, severe operations and infections can trigger acute gastritis.
- Exposure to radiation or radiation therapy (due to another medical condition).
- Bile reflux after gastric resection.
- Allergies to foods such as cow's milk and soy (especially in children).
- Autoimmune diseases. As a result of autoimmune processes, the body produces antibodies that attack the cells that form the gastric mucosa. Autoimmune inflammation occurs, and the functions of the protective barrier of the mucous membrane decrease. Gastritis associated with autoimmune disorders is called autoimmune gastritis. It is more common in people with other autoimmune disorders, including Hashimoto's disease and type 1 diabetes. Autoimmune gastritis may also be associated with vitamin B12 deficiency.
- Other diseases. The risk of gastritis may be increased by other medical conditions, including Crohn's disease, sarcoidosis, parasitic infections, and HIV/AIDS.
Diagnostic measures
If any suspicious symptoms appear (for example, nausea, bloating, heartburn, belching, pain), it is very important to visit a gastroenterologist in a timely manner. One of the main methods for studying the condition of the mucosa is a procedure called esophagogastroduodenoscopy. It is performed using an endoscope - a special probe with a camera at one end to view the internal state.
Using this method, you can accurately assess the condition of the body and the internal walls of the stomach, take a piece of tissue for analysis (biopsy), visualize the presence of a pathological process, and prescribe the correct course of therapy.
A competent specialist will easily determine the presence of pathology in hyperemic epithelium, since healthy tissue looks shiny and produces mucus normally. During the examination, when inflated with air, the folds are straightened, the surface is smooth, the epithelial cover is intact and clean, without wounds or ulcerations. The color is pink, there may be a yellowish coating.
As the disease develops, the symptoms worsen, redness of the epithelial layer appears, the folds increase, do not straighten when inflated, and swelling is observed.
Stages of gastritis
- Hyperemia. At the first stage of gastritis development, hyperemia (redness) of the gastric mucosa is observed. This is a protective vegetative-vascular reaction - dilation of blood vessels and increased blood flow in response to a negative effect on the mucous membrane. Hyperemia is accompanied by edema, this is a sign of the development of inflammation.
- Chronic inflammation, metaplasia, dysplasia. The production of hydrochloric acid decreases, the mucous membrane thickens. Hypertrophy is typical for people who abuse alcohol. Inflammation is characterized by the accumulation of leukocytes in the stomach wall; prolonged inflammation can change the structure of the gastric epithelium, it can become similar to intestinal epithelium, this phenomenon is called metaplasia and may be associated with an increased risk of cancer. But the risk is especially high if a biopsy reveals a violation of the structure of the tissue and cells of the stomach - dysplasia.
- Atrophy. Prolonged inflammation causes thinning of the gastric mucosa, recovery processes slow down, atrophic changes in the mucosa are observed - epithelial cells die and are replaced by scar tissue.
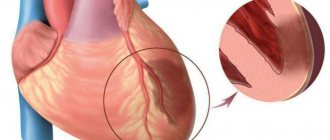
- Erosion and ulcers are a frequent companion to gastritis. Focal and profound changes develop due to a decrease in the performance of the mucous glands, thinning of the protective layer, in most cases this is a consequence of exposure to H. pylori.
Clinical manifestations
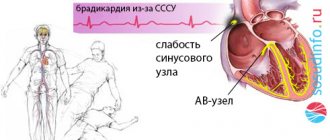
Patients whose gastric mucosa is severely hyperemic rarely realize this. Some symptoms may not be related to the gastrointestinal tract at all. At the initial stage, the heart rate increases. Drowsiness or problems with urination appear. Depending on where the foci of severe hyperemia are localized, the patient experiences:
- fatigue;
- obesity;
- swelling of the face.
Treatment of gastritis
Treatment for gastritis depends on the cause. Acute gastritis caused by taking NSAIDs or alcohol abuse does not require drug therapy; it is enough to exclude these triggers.
In other cases, your doctor may recommend:
- Antibiotic therapy against H. pylori.
- Drugs that block the production of hydrochloric acid (a component of gastric juice) and promote healing of the mucous membrane (proton pump inhibitors* - omeprazole, lansoprazole, rabeprazole, esomeprazole, dexlanzoprazole, pantoprazole.
- Antacids** (neutralize stomach acid, relieve pain).
* - Long-term use of proton pump inhibitors, especially at high doses, may increase the risk of hip, wrist and spine fractures, and an osteoporosis prevention program may be required. ** - Side effects - constipation, diarrhea.
Features and advantages of the gastritis treatment method at the Rassvet clinic
Diagnosis and treatment of gastritis at the Rassvet clinic is carried out in the gastroenterology department. We use evidence-based methods based on international clinical guidelines. Your primary treatment will begin only after a physical examination and all necessary tests and diagnostic tests have been completed.
Important. The influence of certain foods or dietary systems on the risk of gastritis has not been proven by research.
At the Rassvet Clinic, we first of all distinguish gastritis from functional dyspepsia. Gastritis is often asymptomatic, but it is necessary to treat it, since it is a slow but sure road to stomach cancer. Functional dyspepsia, on the contrary, is accompanied by many complaints, but endoscopic examination and biopsy do not reveal pathology.
How gastritis is treated at the Rassvet clinic
To clarify the diagnosis, we use the most modern and accurate equipment and logistics methods. For example, we have built a system for diagnosing gastritis and determining cancer risk according to the OLGA classification. Our endoscopes allow you to perform gastroscopy with multiple magnification and examine the mucous membrane through light filters, taking a biopsy from the most suspicious areas. The biopsy samples themselves are also assessed by the histologist using the OLGA scale, and as a result we obtain a figure that reflects the risk of oncological transformation in the coming years. Further treatment tactics depend on the value of this figure.
We value the comfort of patients, so in Rassvet you can undergo an examination under anesthesia in the shortest possible time.
Recommendations from a gastroenterologist at the Rassvet clinic for patients with gastritis
Timely consultation with a doctor and proper treatment will help keep the disease under control. A strict diet is not needed. However, the rules of a healthy diet should be followed - do not overeat, avoid foods that irritate the mucous membranes (smoked, fried, fatty), and give up alcohol. If you are forced to take painkillers that increase the risk of gastritis, check whether they can be replaced with a drug that is less aggressive on the gastric mucosa (acetaminophen, paracetamol).
Author:
Amelicheva Alena Aleksandrovna medical editor
Symptoms
Any type of hyperemia leads to a decrease in barrier function, inflammation, and corresponding symptoms. Patients complain of pain, burning in the epigastric region, and indigestion. As the disease progresses, heartburn, nausea, and vomiting may appear.
If hyperemia of the inner layer of the stomach is caused by somatic diseases (heart disease, kidney disease), the patient may experience:
- swelling;
- high blood pressure;
- difficulty urinating;
- drowsiness, etc.
In such situations, additional examination is required. Hyperemia is often observed in patients with unstable mental health and under stressful conditions.
How to treat
Arterial hyperemia is not treated in 85% of cases. In such a situation, intensive blood supply to tissues begins as a consequence of independent regeneration of damage. The cells of the stomach receive the necessary amount of oxygen and nutritional components, due to which metabolic processes are accelerated. As a result, cells begin to divide rapidly, and healthy tissues replace damaged structures. In the arterial form of the pathology, doctors only prescribe proper nutrition and help balance the diet.
In the remaining 25% of cases, active hyperemia, as well as venous blood filling, indicate the presence of gastritis. In case of inflammation of the mucous membrane, complex treatment is carried out. The patient must follow a strict diet, take antibiotics to suppress the growth of Helicobacter pylori and other medications to accelerate tissue regeneration. You are allowed to drink herbal infusions and eat honey.
Recommendations for nutrition in pathology
If hyperemic mucosa is detected, the patient is advised to follow a diet. Substances that irritate the mucous membrane should be excluded from the diet: spicy, salty, sour, fatty foods, smoked meats and marinades, alcohol, strong coffee. Fried foods are not recommended. For heat treatment, food should be boiled or steamed.
In the diet you can use:
- chicken, rabbit, turkey, veal, low-fat sea fish;
- a small amount of vegetable fats;
- skim milk, cottage cheese;
- non-acidic fruits and vegetables;
- cereals (rice, oatmeal, buckwheat);
- eggs, no more than 1 per day;
- wheat bread 1-2 grades, crackers.
Meals should be fractional (5-6 times a day), small portions. It is also necessary to observe the temperature regime; the dishes should not be too hot or cold. The optimal temperature is between 15 and 60 degrees Celsius.
Diseases due to gastric hyperemia
In gastroenterology, mucosal hyperemia is associated with stomach diseases such as gastritis and peptic ulcers. In various forms of gastritis, in addition to focal hyperemia, the following signs are observed:
- Spicy . It is characterized by severe hyperemia and swelling of the folds, petechiae, erosions, and copious amounts of thick mucus.
- Chronic . The mucous membrane is pale, dull, grayish in color. Sometimes there are thinned areas (atrophy) with translucent vessels. This is the so-called false hyperemia.
- Superficial gastritis is characterized by diffuse hyperemia, the formation of foamy white mucus, swelling of the folds that do not level out when inflated. Submucosal hemorrhages are sometimes observed.
- Hypertrophic gastritis is characterized by thickening and pronounced diffuse hyperemia of the folds; they acquire a cherry color. Proliferative processes (nodules, warts) are revealed on the surface.
Hyperemia is also present in other forms of gastritis (phlegmonous, necrotic), as well as ulcers. It indicates an inflammatory process. When infected with Helicobacter Pylori, hyperemic manifestations are more pronounced.
Diagnostic methods
Hyperemic changes can only be diagnosed using endoscopy. For diagnosis, fibrogastroduodenoscopy or endoscopic video capsule is used. ultrasound , radiography , CT , MRI visually determine the appearance of the inner layer only indirectly, by identifying swelling of the mucous membrane.
Diagnostics
Having looked at the statistics, we can conclude that almost 90% of people need consultation with a gastroenterologist. To make a correct diagnosis, a specialist prescribes an examination, which is divided into laboratory and instrumental diagnostics.
Laboratory methods include: studies of gastric juice, blood, urine and feces. With their help, you can determine the secretory function, bacterial composition of the gastrointestinal tract, enzyme activity and other important functions. But without instrumental methods, the analysis results are uninformative.
Laboratory methods include: studies of gastric juice, blood, urine and feces. With their help, you can determine the secretory function, bacterial composition of the gastrointestinal tract, enzyme activity and other important functions. But without instrumental methods, the analysis results are uninformative.
- gastroscopy or esophagogastroduodenoscopy (EGDS) is a type of examination that is carried out using special equipment (gastroscope) with a flexible hose, equipped with viewing optics and a camera. Contraindications for manipulation are: heart disease, hypertension, mental disorders, severe respiratory failure. Before performing the procedure, the patient must refuse to eat food no earlier than 8 hours, and water 3 hours before, not take medications, smoke, or even brush their teeth;
- Symptoms of hyperemia of the gastric mucosa The gastric mucosa is focally hyperemic, there is a coating with whitish foamy mucus on the surfaces of the organ in “mucus lakes”, the folds are compacted and are not completely smoothed out with the help of air.
- As cells die, the surface becomes thinner and turns pale. In this case, the foci of the disease do not become hyperemic, and the vascular web is clearly visible.
- In the superficial form of gastritis, the mucous surface of the stomach is hyperemic throughout or only in the body and antrum of the stomach. Sometimes hyperemia is focal in nature or can be diffuse.
- If there is fibrous gastritis, hyperemia is most pronounced, while it is focal and characterized by the presence of pus. This inflammation can be caused by measles or scarlet fever infection. The patient may vomit blood frequently.
- The phlegmous form of the disease can be triggered by trauma to the stomach with sharp objects, such as fish bones. In such cases, this indicates possible hyperemic foci.
- Bulbit is characterized by swelling and redness, thickening of folds in the antrum. Among the reasons are Helicobacter pylori infection of the antrum of the stomach and unhealthy diet.
- Renal dysfunction (various degrees of swelling).
- Depression and permanent stress also provoke hyperemia.
To detect the disease - even if there are almost no problems with the stomach - make an appointment with a gastroenterologist. Gastroscopy is an excellent diagnostic option. Diagnostics involves a procedure carried out by a probe, camera and inspection optics. Using this method, you can assess the condition of organs, take a tissue biopsy, find out the diagnosis and prescribe therapy.
A gastroenterologist will help diagnose the problem. He first examines the patient and collects anamnesis.
After a medical examination, a gastroscopy is performed. It is performed using a special device - an endoscope. It is equipped with viewing optics and a camera.
This diagnosis is an unpleasant and painful procedure, but it allows you to accurately determine the condition of the organ, identify the causes of hyperemia, thanks to which the doctor prescribes the appropriate treatment tactics. In addition, using this method, a biopsy is performed, i.e., tissue is taken for examination.
For preventive purposes, as well as at the slightest suspicion of gastrointestinal diseases, you should seek help from a gastroenterologist. The most accurate and reliable research method is gastroscopy. This procedure involves attaching a camera and optics to the probe, as well as the use of other auxiliary instruments that are inserted deep into the esophagus and stomach.
Gastroscopy allows you to accurately determine the condition of the internal organs of the gastrointestinal tract, identify pathological changes and, if necessary, take a tissue sample for further study.
A doctor can easily notice pathological changes in the epithelium, since in a healthy state they are characterized by transparent mucus, as well as a shiny pink surface. Diagnosis is made on an empty stomach, which allows you to notice the slightest changes not only in the epithelium itself, but also in its thickness.
Gastric hyperemia is characterized by redness of the mucous membrane and indicates the onset of the development of many gastrointestinal diseases. Early diagnosis allows you to determine the cause of its development, as well as eliminate it as quickly and effectively as possible.