Typical symptoms of ketoacidosis
Thirst, weakness, lethargy (many call this condition “cotton-blooded body”), drowsiness, dry lips, frequent urination, nausea, vomiting, diarrhea.
In severe cases, DKA is accompanied by increased blood pressure and pulse, as well as rapid, heavy breathing. These are harbingers of hypersmolar hyperglycemic coma. Call an ambulance urgently!
DKA can develop slowly (due to a relative lack of insulin) and rapidly (for example, on a pump, when for some reason the insulin supply is disrupted). Some medications can also cause DKA (eg, corticosteroids, diuretics).
2. Symptoms of the disease
Acute diabetic ketoacidosis causes breathing problems and swelling of the brain. There is a risk of coma and even death.
Your blood sugar may become quite high before you notice symptoms of ketoacidosis, which include:
- Skin redness (hot and dry skin).
- Visual impairment.
- Feeling thirsty.
- Drowsiness or difficulty waking up. Young children may not be interested in their usual activities.
- Frequent and deep breathing.
- Strong fruity odor from the mouth.
- Loss of appetite, abdominal pain, vomiting.
- Disorientation in time and space.
Visit our Endocrinology page
What to do with ketoacidosis
What you can do at home:
- make correction insulin injections with a syringe pen
- when blood sugar drops, take fast carbohydrates with a joke
- drink more water
- measure blood sugar more often
- give yourself time to rest, come to your senses
- eliminate the cause of DKA (replace the infusion set, change insulin to a more recent one, etc.)
- Monitor ketone levels for at least 24 hours after the incident
If you have symptoms of a hypersmolar condition / if, despite the measures taken, the condition does not improve, call 112!
Who can develop ketoacidosis?
- Type 1 diabetes, especially in children, is often recognized when the patient is admitted to the hospital in a state of ketoacidosis. The patient feels unwell several days or even several weeks before, but does not suspect that the poor health is due to increased blood sugar.
- Ketoacidosis develops in all patients with type 1 diabetes if they stop taking insulin. As a rule, less than a day passes from stopping insulin administration to the development of ketoacidosis.
- In patients with type 1 and type 2 diabetes mellitus with severe infections, purulent processes, heart attacks, strokes and other severe concomitant diseases.
- In patients with type 1 diabetes mellitus during pregnancy.
- In case of inadequate treatment of type 1 diabetes mellitus - infrequent control of blood sugar, skipping insulin doses, poor diet, use of spoiled or expired insulin.
Most patients with type 1 diabetes will experience diabetic ketoacidosis at least once during their lifetime.
Prevention of diabetic ketoacidosis
Nothing super complicated or supernatural is required from you. You just need to be more careful about yourself and your health:
- measure your sugar more often and try to keep it within your target
- check ketones with visual test strips a couple of times a week
- Eat carbohydrates with every meal (if you have type 2, ask your doctor YOUR carbohydrate allowance per meal)
- improve your insulin injection and infusion technique
- do not overuse infusion sets
- When changing your infusion set, check your blood sugar 2-3 hours after installation to make sure insulin is reaching your body.
- do not change your infusion before bed
- minimize errors in calculating carbohydrates and dosages
- Do not skip insulin injections or take glucose-lowering medications!
Let us remember that ketoacidosis is a potentially dangerous, life-threatening condition.
Take care of yourself, Your DiaMarka!
KETOACIDOSIS AND KETOACIDOTIC COMA
To diagnose diabetic ketoacidosis in documented diabetes mellitus presents no difficulties. Emphasis should be laid on the cases in which diabetes mellitus is manifest in the presence of ketoacidosis. Recommendations for treatment of this condition and its complications are given.
I.Yu.
Demidov - Department of Endocrinology MMA named after. THEM. Sechenov (Head - Academician of the Russian Academy of Medical Sciences, Prof. I.I. Dedov)
I.Yu. Demidova – Department of Endocrinology (Head Prof. IIDedov, Academician of the Russian Academy of Medical Sciences, IMSechenov Moscow Medical Academy
TO
Etoacidosis and ketoacidotic coma are one of the main causes of death in patients with diabetes mellitus (DM) under the age of 20 years. More than 16% of patients suffering from insulin-dependent diabetes (IDDM) die from ketoacidosis or ketoacidotic coma. The risk of death from ketoacidosis especially increases in cases where the factor provoking the occurrence of this acute complication of diabetes is a severe intercurrent disease. Detection of IDDM in the early stages reduced the incidence of manifestation of this disease in a state of ketoacidosis to 20%. Training patients suffering from diabetes in the principles of self-control and behavioral tactics in emergency situations has significantly reduced the risk of ketoacidosis - up to 0.5-2% of cases per year. Studying the nuances of the pathogenesis of ketoacidosis and creating optimal treatment regimens for this condition have led to a decrease in the incidence of deaths, however, mortality from ketoacidotic coma is 7–19%, and in non-specialized medical institutions this figure is higher.
Pathogenesis
The most common provoking factors for decompensation of diabetes and the development of ketoacidosis are any intercurrent diseases (acute inflammatory processes, exacerbations of chronic diseases, infectious diseases), surgical interventions, injuries, violations of the treatment regimen (administration of expired or improperly stored insulin, errors in prescribing or administering the dose of the drug, malfunction in insulin administration systems, emotional stressful situations, pregnancy and cessation of insulin administration for suicidal purposes. A leading role in the pathogenesis of ketoacidosis
Absolute insulin deficiency plays a role, leading to a decrease in glucose utilization by insulin-dependent tissues and, accordingly, hyperglycemia and severe energy starvation in them.
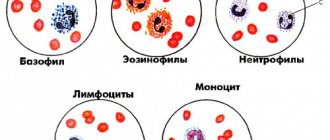
The latter circumstance is the reason for a sharp increase in the blood level of all counter-insulin hormones (glucagon, cortisol, catecholamines, ACTH, STH), stimulation of the processes of glycogenolysis, proteolysis and lipolysis, supplying substrates for gluconeogenesis in the liver and, to a lesser extent, in the kidneys. Gluconeogenesis, combined with direct impairment of glucose utilization by tissues due to absolute insulin deficiency, is the most important cause of rapidly increasing hyperglycemia, increased plasma osmolarity, intracellular dehydration and osmotic diuresis. These factors lead to severe extracellular dehydration, hypovolemic shock and significant electrolyte disturbances. Dehydration and hypovolemia cause a decrease in cerebral, renal and peripheral blood flow, which, in turn, increases the existing hypoxia of the central nervous system and peripheral tissues and leads to the development of oliguria and anuria. Hypoxia in peripheral tissues promotes the activation of anaerobic glycolysis processes in them and a gradual increase in lactate levels. The relative deficiency of lactate dehydrogenase with insulin deficiency and the inability to completely utilize lactate in the Measles cycle are the cause of lactic acidosis during decompensation of IDDM. Insulin deficiency and a sharp increase in the concentration of all counter-insulin hormones cause the activation of lipolysis and the mobilization of free fatty acids (FFA), which contributes to the active production of ketone bodies. Enhanced formation of acetyl-CoA, a precursor of acetoacetate (and acetone during its decarboxylation), and B-hydroxybutyrate is ensured under these conditions by the active entry of FFA into the liver due to their mobilization from peripheral tissues and the predominance of lipolysis processes over lipogenesis in the liver cell itself. The rapid increase in the concentration of ketone bodies during decompensation of diabetes is due not only to their increased production, but also to a decrease in their peripheral utilization and excretion in the urine due to dehydration and oliguria, which replaced polyuria. The dissociation of ketone bodies is accompanied by equimolar production of hydrogen ions. Under conditions of decompensated diabetes, the production of ketone bodies and, consequently, the formation of hydrogen ions exceeds the buffering capacity of tissues and body fluids, which leads to the development of severe metabolic acidosis [1]. The severity of the condition with ketoacidosis is due to sudden dehydration of the body, decompensated metabolic acidosis, severe deficiency of electrolytes (potassium, sodium, phosphorus, magnesium, etc.), hypoxia, hyperosmolarity (in most cases) and often concomitant intercurrent disease.
Clinical picture
Ketoacidosis develops gradually over several days. In the presence of severe concomitant infection, the clinical picture of ketoacidosis develops in a shorter period of time. Early clinical symptoms
ketoacidosis are typical signs of decompensation of diabetes, such as increasing dryness of the mucous membranes and skin, thirst, polyuria, subsequently giving way to oliguria and anuria, weakness, headache, drowsiness, loss of appetite, weight loss, and the appearance of a slight odor of acetone in the exhaled air. If timely assistance is not provided, metabolic disorders worsen, and the clinical signs described above are supplemented by nonspecific symptoms of intoxication and acidosis, such as headache, dizziness, nausea and vomiting, which soon becomes more frequent and becomes indomitable. Vomit in ketoacidosis often has a bloody-brownish tint, and doctors mistake this for vomiting “coffee grounds.” As ketoacidosis increases, the smell of acetone in the exhaled air intensifies, and breathing becomes frequent, noisy and deep (respiratory compensation, Kussmaul breathing). The symptom that is observed in more than half of the patients deserves special attention - the so-called “abdominal syndrome” of ketoacidosis, manifested by the clinical picture of “acute abdomen”. Often, the combination of abdominal pain, vomiting and leukocytosis observed in ketoacidosis leads to diagnostic errors and surgical interventions that are unacceptable in this condition, often resulting in death. The risk of such errors is especially high in the case of diabetes manifestation in a state of ketoacidosis. An objective examination reveals pronounced signs of dehydration (in severe cases, patients lose up to 10–12% of body weight). Tissue turgor decreases sharply. The eyeballs become soft, and the skin and visible mucous membranes become dry. The tongue is covered with a thick brown coating. Muscle tone, tendon reflexes, body temperature and blood pressure are reduced. A rapid pulse of weak filling and tension is detected. The liver, as a rule, protrudes significantly from under the edge of the costal arch and is painful on palpation. Kussmaul's breath is accompanied by a pungent odor of acetone in the exhaled air. When examining patients in a state of ketoacidosis, it is necessary to clarify as quickly as possible the cause that provoked decompensation of diabetes. If there is a concomitant intercurrent disease, its treatment should be started immediately. From the first signs of decompensation of diabetes, patients show signs of first mild, and then more and more pronounced depression of the central nervous system. So, first, patients complain of a headache, become irritable, and then lethargic, apathetic, and drowsy. The developing state of stupor is characterized by decreased levels of wakefulness, slower conscious responses to stimuli, and increased periods of sleep. As metabolic disorders worsen, the state of stunned stupor, often called a precomatous state, clinically manifested by deep sleep or unresponsiveness similar to it in behavioral reactions. The final stage of increasing depression of the central nervous system is coma, characterized by a complete lack of consciousness. A blood test reveals hyperglycemia, hyperketonemia, increased levels of urea nitrogen, creatinine and, in some cases, lactate. Plasma sodium levels are usually reduced. Despite the significant loss of potassium through osmotic diuresis, vomit and stool, leading to a pronounced deficiency of this electrolyte in the body, its plasma concentration may be normal or even slightly increased in anuria. Urine examination reveals glycosuria, ketonuria and proteinuria. Acid-base status (ABS) reflects decompensated metabolic acidosis, with blood pH falling below 7.0 in severe cases. The ECG may show signs of myocardial hypoxia and conduction disturbances. If it is known that the patient has diabetes, diagnosing ketoacidosis and ketoacidotic coma is not difficult. The diagnosis is confirmed by the clinical picture described above, laboratory parameters (primarily hyperglycemia, the presence of glucose and ketone bodies in the urine) and CBS, indicating the presence of decompensated metabolic acidosis. In the case of diabetes manifestation immediately in a state of ketoacidosis or coma, one should first of all focus on the presence of severe dehydration, signs of acidosis (Kussmaul breathing) and significant loss of body weight in a short period of time. In this case, the CBS study excludes respiratory alkalosis as the cause of hyperventilation and confirms the presence of metabolic acidosis in the patient. In addition, the smell of acetone in the exhaled air should lead the doctor to believe that the patient has ketoacidosis. Lactate acidosis, uremia, alcoholic ketoacidosis, poisoning with acids, methanol, ethylene glycol, paraldehyde, salicylates (other causes of metabolic acidosis) are not accompanied by such pronounced dehydration and significant loss of body weight, and also manifest themselves with a typical clinical picture. The presence of hyperglycemia and ketonuria confirms the diagnosis of diabetes and ketoacidosis.
Treatment
Treatment of patients in a state of decompensated diabetes, and even more so in a state of ketoacidosis or ketoacidotic coma, should begin immediately. Patients are hospitalized in a specialized department, and in a state of coma - in the intensive care unit. The main goals of therapy for ketoacidosis are the fight against dehydration and hypovolemic shock, restoration of physiological CBS, normalization of electrolyte balance, elimination of intoxication and treatment of concomitant diseases.
Immediately before starting therapy, the patient's stomach is washed with a solution of sodium bicarbonate.
A urinary catheter is inserted to monitor renal function and urine output. In order to improve tissue oxygenation, oxygen inhalation is established. Given hypothermia, the patient must be covered warmly, and solutions should be administered warmed. To monitor the effectiveness of the therapy, before starting treatment, monitor glycemia, blood pH, pCO2, levels of K, Na, lactate and ketone bodies in the blood, glucosuria and ketonuria, blood pressure, ECG, hemoglobin level, hematocrit, respiratory rate (RR), pulse. Subsequently, it is necessary to monitor glycemia, blood pH, pCO2, blood pressure, ECG, respiratory rate, and pulse hourly. Other indicators can be assessed every 2–3 hours. An assessment of the reaction of the pupils to light has an important prognostic value (especially in a coma). A weak reaction or its complete absence indicates developed structural changes in the brain stem and a low probability of a favorable outcome of the disease. Rehydration
is very important in the treatment of diabetic ketoacidosis due to the large role of dehydration in the chain of metabolic disorders in this condition.
The volume of lost fluid is replenished with physiological (or hypotonic with hyperosmolarity) and 5–10% glucose solutions. Termination of infusion therapy is possible only with complete restoration of consciousness, absence of nausea, vomiting, and the patient is able to take fluids per os. During the first hour, 1 liter of 0.9% NaCl solution is administered intravenously. In the presence of hyperosmolarity, saline solution can be replaced with a hypotonic 0.45% NaCl solution. Effective osmolarity is calculated using the following formula: Osmolarity = 2 + blood glucose (mOsm) (mmol/l), normal value = 297 ± 2 mOsm/l Over the next two hours from the start of therapy, 500 ml of 0.9% NaCl solution is administered hourly . In the following hours, the rate of fluid administration should usually not exceed 300 ml/h. After the glycemic level decreases below 14 mmol/l, the saline solution is replaced with a 5–10% glucose solution and administered at the rate indicated above. The administration of glucose at this stage is dictated by a number of reasons, among which the main one is maintaining the required blood osmolarity. A rapid decrease in glycemia and the concentration of other high-osmolar blood components during infusion therapy often causes an undesirable rapid decrease in plasma osmolarity. Insulin therapy
begins immediately after the diagnosis of ketoacidosis.
When treating ketoacidosis, like any other urgent condition in diabetes, only short-acting insulin is used (Actrapid MS, Actrapid NM, Humulin R, Insuman Rapid, etc.). Until the CBS is normalized and the glycemic level is reduced below 14.0 mmol/l, insulin is administered only intravenously or intramuscularly into the rectus abdominis muscle. Upon reaching the specified level of glycemia and normalization of the CBS, the patient is transferred to subcutaneous administration of short-acting insulin. The dose of insulin in the first hour of treatment is 10 units intravenously or 20 units intramuscularly. In case of concomitant severe purulent infection, the first dose of insulin can be doubled. Subsequently, an average of 6 units of short-acting insulin is injected hourly intramuscularly or together with physiological NaCl solution intravenously. To do this, add 10 units of insulin for every 100 ml of saline solution to a separate container with a 0.9% NaCl solution. The resulting mixture is thoroughly shaken. In order to adsorb insulin on the walls of the system, 50 ml of the mixture is passed through it in a stream. The use of previously used albumin solutions for the same purpose is currently considered optional. 60 ml of the specified mixture is administered intravenously every hour. If during the first 2–3 hours from the start of therapy the glycemic level does not decrease, it is recommended to double the insulin dose in the next hour. When the glycemic level reaches 12 - 14 mmol/l, the dose of administered insulin is reduced by 2 times - to 3 units hourly (30 ml of a mixture of insulin and saline solution). At this stage of therapy, it is possible to transfer the patient to intramuscular injections of insulin, but it should be borne in mind that the insulin syringes used and various individual systems for administering the hormone are equipped with needles only for subcutaneous administration of insulin. You should not strive to reduce the glycemic level below 10 mmol/l, since this increases the risk of not only hypoglycemia, but, above all, hyposmolarity. However, if the glycemic level decreases below 10 mmol/L with persistent acidosis, it is recommended to continue to administer insulin hourly and reduce the dose to 2 - 3 units/hour. When the CBS is normalized (mild ketonuria may persist), the patient should be transferred to subcutaneous insulin injections of 6 units every 2 hours, and then every 4 hours at the same dose. In the absence of ketoacidosis, on the 2nd - 3rd day of treatment, the patient can be transferred to 5 - 6 single injections of short-acting insulin, and subsequently to conventional combination insulin therapy. Restoring electrolyte balance
, primarily potassium deficiency, is an important component of the comprehensive treatment of ketoacidosis.
Typically, KCl administration begins 2 hours after the start of infusion therapy. However, if before the start of treatment there are already ECG or laboratory signs confirming hypokalemia in the obligatory absence of anuria, potassium administration can be started immediately, since the administration of fluid and insulin helps to quickly reduce the level of potassium in the blood by diluting its concentration and normalizing the transport of potassium into the cell . The dose of KCL solution administered intravenously depends on the concentration of potassium in the plasma. So, when the potassium level is below 3 mmol/l, it is necessary to administer 3 g/h (dry matter), at 3 – 4 mmol/l – 2 g/h, at 4 – 5 mmol/l – 1.5 g/h, at 5 – 6 mmol/l – 0.5 g/hour. When the plasma potassium level reaches 6 mmol/l, the administration of the KCl solution should be stopped. As a rule, patients do not need additional correction of hypophosphatemia. The question of the need to administer potassium phosphate arises only if the level of phosphorus in the plasma decreases below 1 mg%. Restoration of CBS
begins literally from the first minutes of treatment for ketoacidosis, thanks to the administration of fluids and the administration of insulin.
Restoring fluid volume triggers physiological buffer systems, in particular, the ability of the kidneys to reabsorb bicarbonates is restored. Insulin administration suppresses ketogenesis and thereby reduces the concentration of hydrogen ions in the blood. However, in a number of cases the question arises about the need to prescribe sodium bicarbonate in order to correct CBS. It was noted above that even significant peripheral metabolic acidosis is not always accompanied by an equally pronounced acidosis of the central nervous system, due to the presence of a number of protective and adaptive mechanisms. According to J. Ohman et al. J. Posner and F. Plum [2], in patients with diabetic ketoacidosis, before the start of therapy, the pH of the cerebrospinal fluid is usually within normal limits. Attempts to correct plasma acidosis with intravenous administration of sodium bicarbonate can lead to the rapid development of central nervous system acidosis and a sharp deterioration in the patient’s state of consciousness. Taking into account the described side effects when administering soda, very strict criteria for prescribing sodium bicarbonate for diabetic ketoacidosis have been developed. The question of the advisability of administering soda should be considered only when the blood pH level is below 7.0. It must be emphasized that in this case it is very important to constantly monitor changes in the CBS, and when the pH value reaches 7.0, the introduction of bicarbonate should be stopped. Use a 4% solution of sodium bicarbonate at the rate of 2.5 ml per 1 kg of actual body weight intravenously, very slowly. When administering sodium bicarbonate, an additional KCl solution is injected intravenously at the rate of 1.5–2 g of KCl dry matter [2]. For the treatment or prevention of inflammatory diseases,
broad-spectrum antibiotics are prescribed.
To improve the rheological properties of blood
and prevent disseminated intravascular coagulation, 5000 units of heparin are administered intravenously twice on the first day of treatment under the control of a coagulogram. In order to normalize oxidative processes, add 150–200 ml of cocarboxylase and 5 ml of a 5% ascorbic acid solution. For low blood pressure and other symptoms of shock, therapy is aimed at increasing and maintaining blood pressure and cardiac activity. After removing the patient from the state of ketoacidosis, a gentle diet rich in carbohydrates, proteins, and potassium is prescribed. Avoid fats from the diet for at least a week.
Complications of ketoacidosis
Among the complications that arise during the treatment of ketoacidosis, the greatest danger is cerebral edema, which is fatal in 70% of cases (R. Couch et al., 1991; A. Glasgow, 1991). The most common cause of cerebral edema is a rapid decrease in plasma osmolarity and glycemic levels during infusion therapy and insulin administration. In the case of using sodium bicarbonate to correct acidosis, additional prerequisites are created for the occurrence of this formidable complication. An imbalance between the pH of peripheral blood and cerebrospinal fluid increases the pressure of the latter and facilitates the transport of water from the intercellular space into brain cells, the osmolarity of which is increased. Typically, cerebral edema develops 4–6 hours after the start of treatment for diabetic ketoacidosis. In the case when the patient’s consciousness is preserved, signs of incipient cerebral edema are deterioration in health, severe headache and dizziness, nausea, vomiting, visual disturbances, as well as tension in the eyeballs, instability of hemodynamic parameters, and increasing fever. As a rule, the listed clinical symptoms appear after a “bright” period of improvement in health against the background of obvious positive dynamics in laboratory parameters. It is much more difficult to suspect incipient cerebral edema in patients in a state of ketoacidotic coma. A sure sign of this complication at the initial stage is the absence of positive dynamics in the patient’s state of consciousness against the background of an objective improvement in carbohydrate metabolism. The clinical signs of cerebral edema described above are accompanied by a decrease or absence of pupillary response to light, ophthalmoplegia and papilledema. Ultrasound encephalography and computed tomography confirm the diagnosis. Treatment of cerebral edema is much more difficult than diagnosing this condition. If it is confirmed that the patient has cerebral edema, osmotic diuretics are prescribed - intravenous drip administration of a mannitol solution at a rate of 1 - 2 g/kg. Following this, 80–120 mg of Lasix and 10 ml of hypertonic sodium chloride solution are administered intravenously [4]. The question of the advisability of prescribing glucocorticoids (preference is given exclusively to dexamethasone due to its minimal mineralocorticoid properties) has not been fully resolved. It is believed that the greatest effect from the administration of these hormones is observed in cases of cerebral edema due to injury or tumor. However, given the ability of glucocorticoids to reduce pathologically increased vascular permeability and the blood-brain barrier, normalize ion transport through the cell membrane and inhibit the activity of lysosomal enzymes of brain cells, the question of the advisability of their use for cerebral edema in ketoacidosis should be decided individually. Brain hypothermia and active hyperventilation of the lungs are added to the therapeutic measures taken to reduce intracranial pressure due to the resulting vasoconstriction. In some cases, craniotomy should be considered. Other complications of ketoacidosis and its therapy include disseminated intravascular coagulation, pulmonary edema, acute cardiovascular failure, hypokalemia, metabolic alkalosis, and asphyxia due to aspiration of gastric contents.
Strict monitoring of hemodynamic parameters, hemostasis, electrolyte content, changes in osmolarity and neurological symptoms allows us to suspect the above complications in the early stages and immediately take effective measures aimed at eliminating them.
Literature:
1. Krane E. Diabetic Ketoacidosis. Ped Clinics N Amer 1987;34:935–60. 2. Plum F., Posner J.B. Diagnosis of stupor and coma. Translated from English: Medicine, 1986. – 544 p. ill. 3. Beaser R. Diabetic emergencies. Joslin Diabetes Center. Lecture Notes. October, 1992:12. 4. Diabetic ketoacidosis – A Scheme for management. In: Diabetes in the Young. ISGD. Official Bulletin 1990;23:13–5.
Mechanism of development of decompensation
The development of ketoacidosis in diabetes is associated with insufficient insulin in the body. Without the influence of this pancreatic hormone, the utilization of glucose is impossible, so a situation develops that can be called “hunger among plenty.” In this pathological condition, there is enough sugar in the body, but its use as a source of energy is impossible.
At the same time, the release of adrenaline, cortisol, somatotropic and adrenocorticotropic hormone, and glucagon increases. This leads to a rapid increase in glucose levels in the body. Once the renal threshold is exceeded, it begins to be excreted through the kidneys along with a large volume of fluid and ions.
Due to blood thickening, tissue hypoxia develops, due to which glucose molecules are oxidized through the anaerobic pathway. This contributes to an increase in lactate concentration and the subsequent development of lactic acidosis. At the same time, the body tries to use fatty acids as an alternative source of energy, which serve as the basis for the formation of ketone bodies, which leads to the development of acidosis.
3.Diagnosis and treatment of the disease
How is ketoacidosis diagnosed?
Laboratory tests, including blood and urine tests, are used to confirm the diagnosis of diabetic ketoacidosis. Home urine ketone tests are also available for use. Keep them on hand in case your blood sugar levels rise.
Treatment of diabetic ketoacidosis
Acute ketoacidosis is a serious condition and must be treated in a hospital. Often patients require not just hospitalization, but treatment in the intensive care unit. Treatment for ketoacidosis involves administering insulin and other drugs intravenously. The levels of certain chemicals in the blood (electrolytes) should be closely monitored. It may take several days for your blood sugar levels to stabilize.
About our clinic Chistye Prudy metro station Medintercom page!
Causes of the pathological condition
Ketoacidosis appears in the following cases:
- When a very low dose of insulin is administered.
- Eating large amounts of carbohydrates.
- Missing a dose of insulin.
- Excessive physical activity.
- Severe stress.
- Excessive alcohol consumption.
- The presence of an infectious disease.
- Using ecstasy or cocaine.
When blood sugar levels are significantly higher than normal, hyperglycemia occurs in the body and the number of ketone bodies increases.