Morgagni-Adams-Stokes syndrome (MAS syndrome) is a syncope that occurs when there is a sudden disturbance of the heart rhythm, and which entails cerebral ischemia and a sharp decrease in cardiac output.
Morgagni syndrome occurs due to cerebral ischemia, which occurs when cardiac output is sharply reduced. This occurs when the heart rhythm or heart rate is abnormal.
Often, Morgagni Adams Stokes attacks are caused by atrioventricular block. An attack occurs when a block occurs, followed by the development of sinus rhythm or supraventricular arrhythmia.
Causes, provoking diseases and factors
Attacks of the syndrome occur during the following processes in the body:
- atrioventricular block;
- transition of incomplete atrioventricular block to complete;
- disturbance of the heart rhythm, which is accompanied by a decrease in myocardial contractility (febrile, ventricular flutter, paroxysmal tachycardia, asystole);
- tachyarrhythmia and tachycardia with a heart rate of more than 200 beats;
- bradyarrhythmia and bradycardia with a heart rate of less than 30 beats.
The risk of developing the syndrome exists if the following conditions are present in the anamnesis:
- Chagas disease;
- inflammatory processes localized in the heart muscle and spreading to the conduction system;
- diffuse proliferation of scar tissue and subsequent heart damage in Lew-Legener disease, rheumatoid arthritis, Libman-Sachs disease, systemic scleroderma;
- diseases with general neuromuscular changes (genetic diseases, myotonia);
- intoxication with medications (beta-blockers, calcium antagonists, cardiac glycosides, Amiodarone, Lidocaine);
- ischemia of the heart muscle in cardiomyopathies, myocardioclerosis, heart attack;
- increased iron deposition in hemochromatosis and hemosiderosis;
- systemic amyloidosis;
- functional conduction disorders in the atrioventricular node.
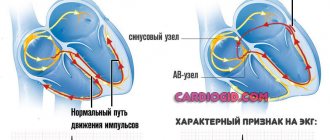
Causes of MAS syndrome
The conduction system of the heart is represented by nerve fibers, impulses along which move in a strictly specified direction - from the atria to the ventricles. This ensures synchronous operation of all chambers of the heart. When obstacles arise in the myocardium (scars, for example), additional conduction bundles formed in utero, the mechanisms of contractility are disrupted, and preconditions for arrhythmia appear.
example of MAS syndrome due to bradycardia
In children, the causes of conduction disorders include congenital defects, disorders of the intrauterine conduction system, in adults - acquired pathology (diffuse or focal cardiosclerosis, electrolyte disturbances, intoxication).
An attack of MAS syndrome is usually provoked by various factors, including:
- Complete AV block, when the impulse from the atria does not reach the ventricles;
- Transformation of incomplete blockade into complete;
- Paroxysmal tachycardia, ventricular fibrillation, when the contractility of the heart muscle drops sharply;
- Tachycardia over 200 and bradycardia below 30 heart beats per minute.
It is clear that such severe arrhythmias do not arise on their own; they require a substrate, which appears when the myocardium is damaged due to ischemic disease, after a heart attack, or inflammatory processes (myocarditis). Intoxication with drugs from the group of beta-blockers and cardiac glycosides may play a certain role. Patients with rheumatic diseases (systemic scleroderma, rheumatoid arthritis) deserve increased attention, when cardiac involvement with inflammation and sclerosis is likely.
Depending on the predominant symptoms, it is customary to distinguish several variants of the course of MAS syndrome:
- Tachyarrhythmic, when the heart rate reaches 200-250, the function of blood ejection into the aorta is sharply affected, the organs experience hypoxia and ischemia.
- Bradyarrhythmic form - the pulse decreases to 30-20 per minute, and the cause is usually complete atrioventricular block, weakness of the sinus node and its complete stop.
- Mixed type with alternating paroxysms of asystole and tachycardia.
Features of the clinical picture
The syndrome is observed in 25-60% of patients with complete atrioventricular block. The frequency and number of attacks varies in each clinical case. Attacks of Morgagni Edema Stokes can occur every few years, or can occur several times within one day.
An attack can be triggered by sudden movements, sudden changes in body position, nervous overload, anxiety, and emotional stress.
The attack is preceded by the following signs:
- dizziness;
- sudden concern;
- weakness;
- darkening of the eyes;
- headache;
- noises in the ears and head;
- increased sweating;
- nausea, vomiting;
- pale skin;
- blue lips;
- impaired coordination of movements.
After some time (about 1 minute), the patient has an attack and loses consciousness. Fainting occurs when the heart rate is less than 30.
Fainting is often short-lived and does not last more than a few seconds. During this time, compensatory mechanisms are activated, which make it possible to eliminate the arrhythmia. After emerging from this state, the patient experiences retrograde amnesia and has no memory of what happened.
Stopping the heart for more than 1-2 minutes leads to clinical death.
During an attack of Morgagni Adams Stokes syndrome, the following symptoms are characteristic:
- pale skin;
- swelling of the neck veins;
- blue lips and fingertips;
- spontaneous bowel movements and urination;
- cold sweat (clammy);
- weak muscle tone, cramps;
- inability to determine pulse;
- reduced blood pressure;
- dull and arrhythmic heart sounds;
- dilated pupils;
- rare and deep breathing.
Depending on the intensity of symptoms, there are several forms of attack:
- Mild – there is no loss of consciousness, the patient experiences dizziness, sensitivity is impaired, and noise appears in the ears and head.
- Moderate severity - the patient experiences loss of consciousness, but there are no signs such as voluntary urination and defecation, and convulsions are also not observed.
- Severe – the entire symptom complex is present.
Publications in the media
Morgagni–Adams–Stokes syndrome (MAS syndrome) is a disturbance of consciousness caused by a sharp decrease in cardiac output and cerebral ischemia due to an acute cardiac arrhythmia
Classification
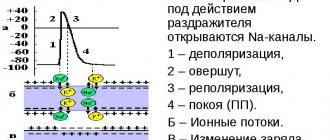
• Bradyarrhythmic form (see Atrioventricular block, Sick sinoatrial node syndrome). The severity of MAS syndrome depends on two factors: •• the duration of asysitolia ••• with a duration of 4–4.5 s there may be no clear symptoms ••• 5–9 s - dizziness, darkening of the eyes ••• 10–15 s - loss consciousness; •• states of cerebral circulation (each patient has his own individual threshold for the onset of an attack).
• Tachyarrhythmic form - occurs at a high heart rate (200 per minute or more), especially with reduced myocardial contractile function. High heart rate often occurs in the presence of additional pathways with a short effective refractory period (>270 ms), with the development of fibrillation, atrial flutter, reentrant AV tachycardia (see Wolff-Parkinson-White syndrome, Atrial fibrillation, Atrial flutter, Tachycardia ventricular, Long QT interval syndrome).
Clinical manifestations • Sudden dizziness or loss of consciousness • Pallor • Arterial hypotension • Tonic-clonic convulsions (with ventricular asystole lasting more than 15 s) • Severe bradycardia or tachycardia.
Special studies • ECG • 24-hour ECG monitoring • EchoCG • Electrophysiological study
TREATMENT
Bradyarrhythmic form • Temporary endocardial or transthoracic external pacemaker • Drug therapy allows you to gain time to prepare for pacemaker •• Atropine - 1 mg IV, repeated after 3-5 minutes until the effect is achieved or a total dose of 0.04 mg/kg is achieved • • If there is no effect - aminophylline IV slowly at a dose of 240-480 mg •• If there is no effect - either dopamine at a dose of 100 mg, or epinephrine at a dose of 1 mg (isoprenaline 1 mg) in 250 ml of 5% glucose solution IV, gradually increasing the infusion rate until a minimum sufficient heart rate is achieved • Surgical treatment - pacemaker implantation is indicated.
Tachyarrhythmic form • Relief of tachycardia paroxysm by electrical pulse therapy. In case of long Q-T interval syndrome complicated by ventricular tachycardia of the “pirouette” type, intravenous administration of magnesium is indicated (see Ventricular tachycardia, Long Q-T interval syndrome) • Surgical treatment •• For Wolff-Parkinson-White syndrome - ablation of additional conductions pathways •• For atrial fibrillation and flutter - ablation of the His bundle with pacemaker implantation (in VVI mode) •• For ventricular tachycardia - implantation of a cardioverter-defibrillator.
Synonyms • Adams–Stokes syndrome • Adams–Morgagni–Stokes syndrome • Spence syndrome • Stokes syndrome.
ICD-10 • I45.9 Conduction disorder, unspecified
Emergency first aid
During an attack of Morgagni-Adams-Stokes syndrome, the patient needs emergency medical care, which will determine the duration of the attack itself and the patient’s life.
The first step is mechanical defibrillation, also called precordial shock. It is necessary to strike with your fist in the chest, namely in its lower part. You cannot hit the heart area. After mechanical defibrillation, the heart reflexively begins to contract.
If there is no effect, electrical defibrillation is performed. To do this, electrodes are placed on the patient's chest and an electric shock is given. After this, the correct heart rate should return.
In the absence of breathing, artificial ventilation is performed. To do this, air is blown into the patient’s mouth using a special device, or using the “mouth to mouth” technique.
Cardiac arrest is an indication for injection of Epinephrine (intracardiac) or Atropine (subcutaneous).
Resuscitation measures continue until the attack stops or until death occurs.
If the patient remains conscious, then he needs to be given the drug Izadrin under the tongue (the effect is similar to Adrenaline, Ephedrine, Norepinephrine, but there is no increase in blood pressure).
The patient must be taken to the intensive care unit of the hospital. In the hospital, emergency care is accompanied by monitoring on an ECG machine. The patient is injected subcutaneously with Atropine sulfate and Ephedrine several times a day, and Izadrin is given under the tongue. If necessary, electrical stimulation is performed.
Mycobacterium avium and Mycobacterium avium complex
| Mycobacterium avium infection . Microscopic picture of non-necrotizing granuloma in the lymph node in the neck |
Mycobacterium avium
(English and Latin
Mycobacterium avium
) is a type of gram-positive, non-motile, aerobic, slow-growing, acid-fast, rod-shaped mycobacteria, which are characterized by a high lipid content in the cell and, especially, in the cell wall.
Mycobacterium avium
are typical inhabitants of the environment and, at the same time, causative agents of mycobacteriosis, opportunistic pathogens of wild and domestic animals (pigs, etc.), birds and humans. They belong to the so-called non-chromogenic non-tuberculous mycobacteria (NTMB).
Mycobacterium avium in gastroenterology
Mycobacterium avium
are also causative agents of infectious diseases of the gastrointestinal tract, in particular infectious gastritis and duodenitis.
In ICD-10 Mycobacterium avium
isolated only as a causative agent of pulmonary infection [A31.0].
The draft ICD-11ß (dated January 20, 2015) mentions “Mycobacterium avium-intracellulare gastritis” (“Gastritis due to infection with Mycobacterium avium”) and “Non-tuberculous mycobacterial duodenitis” (“non-tuberculous mycobacterial” duodenitis) in separate lines. The classification of gastritis and duodenitis, based on the etiological principle, proposed by the 2015 Kyoto consensus also includes “Mycobacteria gastritis” (“mycobacterial” gastritis) and “Mycobacterial duodenitis” (“mycobacterial” duodenitis) (Sugano K. et al., Mayev I .V. and others).
Mycobacterium avium
, unlike other mycobacteria, including those included in the
Mycobacterium avium complex
(MAC)
Mycobacterium intracellulare
, are able to penetrate the human body not only through the respiratory, but also through the gastrointestinal tract, getting into the oral cavity with food or water, is capable persist in the acidic environment of the stomach and affect the intestinal mucosa.
For gastritis caused by Mycobacterium avium
, the following microscopic changes are observed: in the lamina propria there is a monotonous infiltrate of foamy histiocytes, there are no granulomas. There is also positive staining of the pathogen with strong acidic dyes.
Berrill Bernard Krohn (1884-1983), who first (together with his colleagues) described the disease that was later named after him, believed that it was caused by the bacterium Mycobacterium avium subsp. paratuberculosis
. But with later research this was refuted.
MAC infections of the gastrointestinal tract in HIV-infected patients
People living with HIV have an increased risk of infections caused by atypical mycobacteria, especially Mycobacterium avium complex
(MAC). Disseminated MAC infection is accompanied by both general manifestations and gastrointestinal symptoms: night sweats, abdominal pain, diarrhea and weight loss. If these symptoms are present, X-ray contrast examination of the gastrointestinal tract and computed tomography (CT) of the abdomen are usually prescribed. CT most often reveals enlarged retroperitoneal and mesenteric lymph nodes (42%), hepatomegaly (50%), splenomegaly (46%) and thickening of the wall of the small intestine (14%). X-ray contrast examination of the upper gastrointestinal tract can detect ulcers of the esophagus or pathology of the small intestine - thickening and deformation of the folds of the mucosa, as well as signs of increased secretion. CT scan of the abdomen often (in more than 80% of cases) reveals significantly enlarged retroperitoneal and mesenteric lymph nodes. Lymph nodes in MAC infection tend to form conglomerates and are uniform in density, whereas in tuberculosis they are larger and have areas of low density in the center. Severe hepatomegaly is possible. It is more common with MAC infection than with tuberculosis. In most cases, biopsies obtained under CT guidance reveal large macrophages with foamy cytoplasm containing acid-fast bacteria. Intracellularly located rods can give a positive CHIC reaction. This, together with the clinical and radiological presentation, makes the gastrointestinal involvement of MAC infection similar to Whipple's disease. All of the above suggests that the gastrointestinal tract may be a portal of entry for MAC (Goodman F.S.).
Mycobacterium avium in modern taxonomy of bacteria. Mycobacterium avium complex (MAC)
The species Mycobacterium avium
according to modern taxonomy* is included in the
Mycobacterium avium complex
(MAC), which belongs to the genus of mycobacteria (lat.
Mycobacterium
), family
Mycobacteriaceae
, order
Corynebacteriales
, class
Actinobacteria
, phylum
Actinobacteria
, <group without rank>
Terrabacteria group
, kingdom Bacteria .
In Mycobacterium avium complex
currently* species included (only species with proper names are listed, species designated by alphanumeric code are omitted):
- Mycobacterium arosiense
- Mycobacterium avium
- Mycobacterium avium-intracellulare
- Mycobacterium bouchedurhonense
- Mycobacterium chimaera
- Mycobacterium colombiense
- Mycobacterium indicus pranii
- Mycobacterium intracellulare
- Mycobacterium lepraemurium
- Mycobacterium mantenii
- Mycobacterium marseillense
- Mycobacterium paraintracellulare
- Mycobacterium timonense
Mycobacterium avium
species has the following subspecies:
- Mycobacterium avium subsp. avium
- Mycobacterium avium subsp. hominissuis
- Mycobacterium avium subsp. paratuberculosis
- Mycobacterium avium subsp. silvaticum
The species Mycobacterium intracellulare
has the following subspecies:
- Mycobacterium avium subsp. intracellulare
- Mycobacterium intracellulare subsp. yongonense
* Discussion of various approaches in the taxonomy of living organisms is beyond the scope of the “Functional Gastroenterology” site. For reasons of certainty and ease of use, we focus on the taxonomy of the National Center for Biotechnology Information, without claiming that it is in any way better or worse than others.
Establishing diagnosis
Loss of consciousness is possible with various diseases. Therefore, when conducting diagnostics, Adams-Stokes-Morgagni syndrome must be differentiated from the following conditions:
- Meniere's syndrome;
- hypoglycemic state;
- stroke;
- hysteria;
- orthostatic hypotension;
- attack of transistor ischemic attack of the brain;
- severe aortic stenosis;
- pulmonary embolism;
- thrombosis of the heart chambers;
- epilepsy.
To determine the syndrome, the following diagnostic methods are used:
- electrocardiogram (ECG) in dynamics;
- ECG monitoring using a Holter device (allows you to identify temporary changes, a combination of atrial flutter and fibrillation);
- long-term electroencephalogram monitoring;
- contrast coronography of vessels;
- myocardial biopsy.
Treatment of the syndrome
Initiation of treatment implies emergency assistance during an attack. This is followed by therapy, the purpose of which is to prevent recurrence of attacks of Morgagni Adams Stokes syndrome. Treatments are carried out in the cardiology department.
Initially, the causes of attacks are identified, a detailed examination of the heart is carried out, the diagnosis is clarified and a set of therapeutic measures is prescribed. The following methods of treating the syndrome are used.
Drug treatment
After the patient is admitted to the intensive care unit, he is treated with medications. Droppers with the introduction of Ephedrine and Orciprenaline are used. Every 4 hours the patient is given Izadrin. Injections of Ephedrine and Atropine are given.
Inflammatory processes are relieved with corticosteroids. Since bradycardia is accompanied by tissue acidosis and hyperkalemia, it is necessary to take diuretics and an alkaline solution. This helps remove potassium from the body and normalize blood pressure.
After the attack has stopped, preventive therapy is prescribed with the use of antiarrhythmic drugs, and therapeutic measures are also directed to get rid of the main cause of the syndrome (ischemia, intoxication, inflammatory process).
Surgery
If there is a risk of sudden cardiac arrest and recurrence of attacks, then the necessary measure is the implantation of a pacemaker. It is possible to use two types of pacemakers: with a complete blockade - a device that provides constant stimulation of the heart, with an incomplete blockade - a device that is triggered in case of abnormalities.
During surgery, an electrode is inserted through a vein and secured into the right ventricle of the heart. The stimulator body is fixed in the rectus abdominis muscle (in men) or in the retromammary space (in women).
The pacemaker must be checked for functionality every 3-4 months.
How to make the correct diagnosis?
In the diagnosis of MAS syndrome, the main importance is given to electrocardiographic techniques - ECG at rest, 24-hour monitoring. To clarify the nature of the heart pathology, ultrasound examination and coronary angiography may be prescribed. Auscultation is of no small importance, when the doctor can listen to peculiar noises, intensification of the first tone, the so-called three-member rhythm, etc., but all auscultation signs must be correlated with electrocardiographic data.
Since Morgagni-Adams-Stokes syndrome is a consequence of various types of conduction disorders, it does not have electrocardiographic diagnostic criteria as such, and the phenomena on the ECG are associated with the type of arrhythmia that is provoked in a particular patient.
In case of conduction disturbance from the atrial node, the ECG evaluates, first of all, the duration of the PQ interval, which reflects the time of passage of the impulse through the conduction system from the sinus node to the ventricles of the heart.
With the first degree of blockade, this interval exceeds 0.2 seconds; with the second degree, the interval gradually lengthens or exceeds the norm in all cardiac complexes, while QRST periodically falls out, which indicates that the next impulse simply did not reach the ventricular myocardium. In the third, most severe degree of blockade, the atria and ventricles contract on their own, the number of ventricular complexes does not correspond to the P waves, that is, impulses from the sinus node do not reach their end point in the conductive fibers of the ventricles.
variety of arrhythmias causing MAS syndrome
Tachycardia and bradycardia are established based on counting the number of heart contractions, and ventricular fibrillation is accompanied by a complete absence of normal waves, intervals and ventricular complex on the ECG.
Prevention of attacks and relapses
The use of preventive measures is possible for attacks that are caused by paroxysms of tachyarrhythmia or tachycardia. In this case, patients are prescribed various antiarrhythmic drugs.
It is also necessary to exclude factors that lead to an attack - sudden movements, sudden changes in body position, anxiety, nervous overload, emotional stress, intoxication.
In case of complete atrioventricular block, the main preventive method is the installation of a pacemaker.
Features of symptoms
With MAS syndrome, attacks occur suddenly and may be preceded by stress, severe nervous tension, fear, or excessive physical activity. A sudden change in body position, when the patient quickly gets up, can also contribute to the manifestation of heart pathology.
Usually, in the midst of complete health, a characteristic symptom complex of MAS appears, including cardiac disorders and brain dysfunction with loss of consciousness, convulsions, involuntary bowel movements and urine output.
The main symptom of the disease is loss of consciousness, but before it the patient feels some changes , which he can then talk about. Approaching fainting is indicated by darkening of the eyes, severe weakness, dizziness and noise in the head. Cold sticky sweat appears on the forehead, a feeling of nausea or lightheadedness appears, and there may be a feeling of palpitations or constriction in the chest.
20-30 seconds after the paroxysm of arrhythmia, the patient loses consciousness, and the signs of the disease are recorded by others:
- Lack of consciousness;
- The skin turns pale, cyanosis is possible;
- Breathing is shallow and may stop completely;
- Blood pressure drops;
- The pulse is threadlike and often cannot be felt at all;
- Convulsive muscle twitching is possible;
- Involuntary emptying of the bladder and rectum.
If the attack lasts only briefly, and the rhythmic contractions of the heart are restored on their own, then consciousness returns, but the patient does not remember what exactly happened to him. With prolonged asystoles, lasting up to five minutes or longer, clinical death and acute cerebral ischemia occur, and emergency measures cannot be avoided.
The disease can occur without loss of consciousness. This is typical for young patients in whom the vascular walls of the cerebral and coronary arteries are not damaged, and the tissues are relatively resistant to hypoxia. The syndrome is manifested by severe weakness, nausea, dizziness with preservation of consciousness.
Elderly patients with atherosclerosis of the cerebral arteries have a worse prognosis, and their attacks are more severe, with a rapid increase in symptoms and a high risk of clinical death, when there is no heartbeat and breathing, pulse and pressure are not detected, the pupils are dilated and do not respond to light.
What does this mean?
The severity of the consequences directly depends on the frequency of seizures and their duration. Frequent and prolonged brain hypoxia entails a negative prognosis for the disease.
Hypoxia lasting more than 4 minutes causes irreversible brain damage. The absence of resuscitation measures (indirect cardiac massage, artificial respiration) can lead to cessation of cardiac activity, disappearance of bioelectrical activity and death.
The prognosis for surgery is positive. Implantation of a pacemaker allows you to restore the patient’s quality of life, ability to work and health.