Irregularities in the heart rhythm can occur not only as a result of stress and physical overload, but also under the influence of various pathologies.
One of the most common forms of arrhythmia is supraventricular tachycardia. Most often, an attack occurs abruptly and lasts for some time - such a failure occurs in the supraventricular space and is considered not as dangerous as the ventricular form of pathology.
What does it represent?
The problem of supraventricular tachycardia has been well studied by cardiologists for a long time.
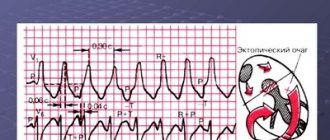
The heart begins to contract vigorously - up to 250 beats per minute, and then also sharply returns to normal function. Normally, the impulses that cause the heart muscle to contract are formed in the area of the sinus node, but sometimes they occur in other areas of the heart - tachycardia develops. This pathology varies according to the location where the impulses are localized. With supraventricular tachycardia, the impulse is formed in the atrioventricular node. Reference! Pathology can be observed at any age, including children.
Description of the violation
The mechanism of development of pathology is as follows:
- According to the re-entry type, cyclic movements of impulses are formed, resulting in the formation of ectopic foci that disrupt the normal heart rhythm.
- The trigger activity of the heart increases, and the sinus rhythm becomes more muffled, as it is interrupted by more intense pathological impulses.
- An additional pathway is formed, which enhances the flow of impulses from one cardiac section to another.
The re-entry mechanism is based on the refractoriness of the heart muscle and heterogeneous conduction, while a higher frequency of contractions of the heart muscle is observed than with other atrial arrhythmias. This is explained by the fact that the re-entry path is not so long and constant.
Reference! Supraventricular tachycardia has ICD-10 code 147.1 (International Classification of Diseases).
Forms
The disease can develop as follows:
- acceleration of impulses in the sinus node - sinus tachycardia;
- depression or complete cessation of the sinus node - atrial tachycardia;
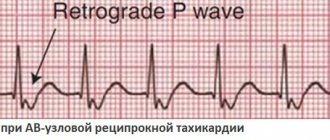
- dysfunction of the atrioventricular connection.
According to the frequency of development of an attack, they are distinguished:
- Paroxysmal tachycardia - attacks develop unexpectedly and very quickly, if the duration of the attack is longer than 30 seconds - this is a stable tachycardia, if less - unstable.
- Chronic - the patient cannot say at what exact moment the heart began to contract more often; there is also no clear boundary for the end of the attack. This condition can last for years, with normal heart rhythm alternating with pathological ones.
Classification of the syndrome
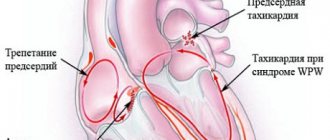
- intermittent - signs of premature excitation of the ventricles on the electrocardiogram may appear and disappear;
- hidden (latent) - the ECG shows signs only of paroxysmal tachycardia with the participation of an anomalous Kent bundle;
- WPW phenomenon - the presence of signs of premature excitation of the ventricles without paroxysms (over time it can transform into a syndrome);
- multiple - established in the case of two or more additional atrioventricular connections (AVJ), which are involved in maintaining retrograde impulse conduction.
Causes
Arrhythmia can develop for many reasons; supraventricular tachycardia is most often observed when the passage of a nerve impulse is disrupted. A pathological focus arising in the atria interferes with the normal functioning of the myocardium.
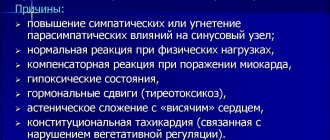
The main causes of supraventricular tachycardia are:
- Damage to the cardiovascular system of an organic nature , as a rule, is morphological changes. These include invasive and viral diseases, complications of coronary circulatory disorders, necrotic changes in the myocardium, ischemic processes that lead to the replacement of the myocardium with connective tissue. All these processes destroy the normal structure of the heart muscle, which naturally leads to disruption of its contractility. This group also includes various defects, Wolff-Parkinson-Wyde syndrome and other congenital developmental anomalies.
- Functional disorders may also be an ethological factor in the development of this disease . They develop as a result of neurogenic dysfunctions. These are vegetative-vascular dystonia, asthenia, cardiovascular nervousness.
- Another cause of pathology is endocrine disorders . If there is no balance in the hormones of the thyroid gland, adrenal glands or pituitary gland, disturbances in the rhythm of heart contractions can also occur. If these failures are permanent, the arrhythmia will be persistent. In addition, diseases of the endocrine system provoke a restructuring of a large number of metabolic processes, and this has a direct impact on the functioning of the heart, and myocardial dystrophy develops.
Reference! If all causes for the development of pathology are excluded, doctors talk about the idiopathic form of the disease.
Supraventricular extrasystole - symptoms and treatment
NVE may be benign. In this case, the risk of sudden death is very low, sometimes the patient does not even feel the rhythm disturbance. Such extrasystole does not always require treatment.
If possible, the etiological factor must be eliminated:
- normalize sleep;
- limit or completely stop taking provoking medications and drinks;
- quit smoking:
- normalize thyroid function in hyperthyroidism;
- adjust the level of potassium in the blood;
- remove the gallbladder in case of cholelithiasis;
- Avoid a horizontal position after eating if you have a hiatal hernia;
- normalize blood pressure;
- increase physical activity according to the body’s capabilities;
- Avoid excessive physical activity (weightlifting, heavy lifting).
The patient is advised to establish a daily routine. The diet should be supplemented with foods rich in potassium and magnesium; they have a beneficial effect on the cardiovascular system.
| Products containing potassium | Products containing magnesium |
| ⠀•⠀dried apricots; ⠀•⠀cocoa powder; ⠀•⠀wheat bran; ⠀•⠀raisins; ⠀•⠀sunflower seeds; ⠀•⠀nuts (pine nuts, almonds, peanuts, walnuts); ⠀•⠀legumes (peas, lentils, beans); ⠀•⠀jacket potatoes; ⠀•⠀avocado; ⠀•⠀ceps; ⠀•⠀bananas; ⠀•⠀citrus fruits; ⠀•⠀Brussels sprouts and kohlrabi; ⠀•⠀milk and fermented milk products; ⠀•⠀cereals (oatmeal, buckwheat, pearl barley, rice); ⠀•⠀fruits (peaches, pears, watermelon, apples, prunes, apricots, melon); ⠀•⠀chicory; ⠀•⠀vegetables (carrots, spinach, green onions, eggplant, cucumbers); ⠀•⠀chicken eggs; ⠀•⠀fish and meat; ⠀•⠀apple juice. | ⠀•⠀oil (sesame, flaxseed, peanut); ⠀•⠀cheese (Dutch, Poshekhonsky, goat, with mold); ⠀•⠀cottage cheese (low-fat and low-fat, curd cheese); ⠀•⠀bitter chocolate; ⠀•⠀almost all types of meat; ⠀•⠀fish (halibut, sturgeon, perch, haddock, cod, saury); ⠀•⠀duck eggs; ⠀•⠀cereals (rolled oats, chickpeas, peas, buckwheat, brown rice, lentils); ⠀•⠀fruits and berries (cherries, kiwi, pineapple, feijoa, raspberries, pears, peach, persimmon); ⠀•⠀many varieties of tea (for example, “Ivan-tea”) and juices; ⠀•⠀ginger; ⠀•⠀mustard; ⠀•⠀vanilla. |
Indications for antiarrhythmic therapy are:
1. Poor tolerance of supraventricular extrasystole. In this case, it is necessary to determine in what situations and at what time of day heart rhythm disturbances most often occur, and then time the drug intake to this time.
2. The occurrence of VVC (not necessarily frequent) in patients with heart defects (primarily mitral stenosis) and other organic heart diseases. In such patients, atrial overload and dilatation progress. Supraventricular extrasystole in this case serves as a harbinger of the occurrence of atrial fibrillation.
3. Supraventricular extrasystole, which arose as a result of a long-term etiological factor in patients without previous organic heart disease and atrial enlargement (with thyrotoxicosis, inflammatory process in the heart muscle, etc.). If antiarrhythmic treatment (along with etiotropic treatment) is not carried out, the risk of persistent EVE increases. Frequent supraventricular extrasystole in such situations is potentially malignant in relation to the development of atrial fibrillation.
4. Frequent (700-1000 extrasystoles per day or more) EVA also requires antiarrhythmic therapy, even if it is regarded as idiopathic, since there is a risk of complications. The approach in these cases should be differentiated. It is also possible to refuse antiarrhythmic therapy if there are reasons for this:
- absence of subjective symptoms and complaints;
- borderline number of extrasystoles;
- intolerance to antiarrhythmic drugs;
- signs of sick sinus syndrome or impaired AB conduction.
Antiarrhythmic drugs used for EVA:
- Beta blockers (Metoprolol, Bisoprolol), calcium antagonists (Verapamil). It is pathogenetically justified to prescribe drugs from this group to patients with hyperthyroidism, a tendency to tachycardia, when EVE occurs against the background of stress and is provoked by sinus tachycardia. Beta blockers are indicated for ischemic heart disease, arterial hypertension, and sympathoadrenal crises. "Verapamil" is prescribed for concomitant bronchial asthma, variant angina, nitrate intolerance, and patients with coronary artery disease.
- “Belloid”, “Teopek” are indicated for patients with vagal-mediated VHE, which develops at night against the background of a decrease in heart rate. These drugs increase the rhythm and are prescribed at night.
- Sotalol (“Sotalex”, “Sotagexal”). It is necessary to select a dose depending on blood pressure and heart rate, the duration of the PQ and QT intervals. Indicated for a combination of ventricular extrasystole and ventricular extrasystole.
- Antiarrhythmics of IA and IC classes (“Dizopyramide”, “Allapinin”, “Propanorm”, “Etatsizin”). Use is not indicated in patients with coronary artery disease who have recently suffered a myocardial infarction due to its arrhythmogenic effect on the ventricles.
- Amiodarone (“Cordarone”). Amiodarone is the most effective antiarrhythmic drug available. Can be prescribed to patients with organic heart damage.
- If monotherapy is insufficiently effective (i.e., using one antiarrhythmic), combinations of drugs can be used.
If the prescribed therapy has a good effect, antiarrhythmics should not be discontinued quickly. Treatment lasts several weeks (months). If there is a threat of developing atrial fibrillation or if there are episodes of it in the anamnesis, NVE therapy is carried out for life. In the case of continuous antiarrhythmic therapy, the minimum effective doses are selected. Patients with an undulating course of EVE should strive to discontinue the antiarrhythmic during periods of improvement (excluding cases of severe organic myocardial damage). The withdrawal of antiarrhythmics is carried out gradually with a decrease in dosage and number of doses per day. After discontinuation, the patient is recommended to have the drug with him (the “pill in his pocket” strategy) for the purpose of rapid administration when the arrhythmia resumes [11].
If there is no effect from antiarrhythmic therapy, with frequent NVE (up to 10,000 per day), the issue of surgical treatment is considered - radiofrequency ablation of arrhythmogenic foci (destruction of foci using electric current) [5].
Symptoms
Paroxysms during supraventricular tachycardia can last from several seconds to several days; the duration of the attack is directly influenced by the cause of the pathology.
The clinical picture of the disease is as follows:
- a sharp increase in the frequency of rhythmic contractions of the heart;
- darkening of the eyes, dizziness, lightheadedness or fainting;
- trembling of the upper extremities;
- speech disorders;
- temporary unilateral muscle paralysis;
- increased work of the sebaceous glands;
- active contraction of blood vessels, which can be seen with the naked eye;
- rapid fatigue and deterioration in performance;
- frequent urination;
- shallow breathing.
It must be said that supraventricular tachycardia is not accompanied by severe symptoms in all cases, and even the presence of symptoms may vary from person to person. In old age, patients very rarely notice any signs of the disease, and the pathology is most often diagnosed accidentally, during a routine ECG.
During pregnancy , supraventricular tachycardia is observed quite often, this is explained by hormonal imbalances and changes.
Wolff-Parkinson-White syndrome: symptoms
Most often, there are no symptoms of this disease; signs are detected already during an electrocardiogram. In more than half of people with this pathology, after stress or physical exertion, cardiologists at the Yusupov Hospital identify complaints of sudden attacks of palpitations, alternating with a feeling of “freezing” in the chest. Chest pain, a feeling of shortness of breath, dizziness, and, less commonly, loss of consciousness may occur. If the symptoms are not severe, they can be relieved by taking a deep breath or holding your breath. In rare cases, complications may occur: ventricular fibrillation and cardiac arrest.
Treatment
Treatment of the pathology should be carried out under ECG monitoring and prescribed by the attending physician.
The use of special medications is required in the following cases:
- paroxysms that pose a threat to the patient’s life;
- significant hemodynamic impairment;
- the patient does not tolerate the attacks well.
Medicines can improve the patient’s quality of life, relieve negative symptoms and restore blood circulation.
To stop attacks the following are prescribed:
- calcium channel antagonists – Diltiazem, Lacidipine;
- sodium channel blockers – Diphenine, Quinidine;
- adrenergic receptor blockers - Coronal, Anaprilin;
- cardiac glycosides - Korglykon, Digoxin.
Maintenance therapy is often prescribed for life, and is combined with emergency medications. It is especially advisable to prescribe it for hypertension, metabolic disorders, atherosclerosis:
- fibrates – Gemfibrozil, Fenofibrate;
- ACE inhibitors – Quinapril, Benazepril;
- statins – Rosuvastin, Pravastatin;
- angiotensin receptor blockers - Azilsartan, Irbesartan.
Electropulse treatment is also indicated , it is carried out as follows:
- after local anesthesia, an electrode connected to an electrocardiograph is inserted into the patient’s esophagus;
- the supraventicular space is stimulated;
- After the procedure, the electrode is removed.
Moreover, according to statistics, even severe forms of tachycardia are eliminated in 95% of cases.
In case of urgent need, surgical treatment can be carried out using the method of cauterization of the pathological focus of catheter ablation.
First aid for an attack is as follows:
- unbutton the top buttons of the patient’s clothing to make breathing easier;
- open the window for fresh air;
- place the patient in a reclining position;
- put a cold compress on your head;
- give a mild sedative, such as hawthorn or valerian;
- For pain in the chest area, put Nitroglycerin under the tongue.